Abstract
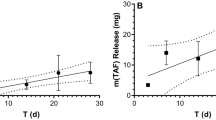
Islatravir (MK-8591) is a highly potent type 1 human immunodeficiency virus (HIV-1) nucleoside reverse transcriptase translocation inhibitor with a long intracellular half-life that is in development for the prevention and treatment of HIV-1. We conducted a randomized, double-blind, placebo-controlled, phase 1 trial in adults without HIV-1 infection. Participants received islatravir or placebo subdermal implants for 12 weeks and were monitored throughout this period and after implant removal. The co-primary end points were safety and tolerability of the islatravir implant and pharmacokinetics, including concentration at day 85, of islatravir triphosphate in peripheral blood mononuclear cells (PBMCs). Secondary end points included additional pharmacokinetic parameters for islatravir triphosphate in PBMCs and the plasma pharmacokinetic profile of islatravir. Based on preclinical data, two doses were assessed: 54 mg (n = 8, two placebo) and 62 mg (n = 8, two placebo). The most frequently reported adverse events were mild-to-moderate implant-site reactions (induration, hematoma, pain). Throughout the 12-week trial, geometric mean islatravir triphosphate concentrations were above a pharmacokinetic threshold of 0.05 pmol per 106 PBMCs, which was estimated to provide therapeutic reverse transcriptase inhibition (concentration at day 85 (percentage of geometric coefficient of variation): 54 mg, 0.135 pmol per 106 cells (27.3); 62 mg, 0.272 pmol per 106 cells (45.2)). Islatravir implants at both doses were safe and resulted in mean concentrations above the pharmacokinetic threshold through 12 weeks, warranting further investigation of islatravir implants as a potential HIV prevention strategy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
MSD is committed to providing qualified scientific researchers access to anonymized data and clinical study reports from the company’s clinical trials for the purpose of conducting legitimate scientific research. MSD is also obligated to protect the rights and privacy of trial participants and, as such, has a procedure in place for evaluating and fulfilling requests for sharing company clinical trial data with qualified external scientific researchers. The MSD data sharing website (http://engagezone.msd.com/ds_documentation.php) outlines the process and requirements for submitting a data request. Although phase 1 trials in healthy volunteers are out of scope as per the MSD data sharing policy, an exception will be made in this case. Applications will be promptly assessed for completeness and policy compliance. Feasible requests will be reviewed by a committee of MSD subject matter experts to assess the scientific validity of the request and the qualifications of the requesters. In line with data privacy legislation, submitters of approved requests must enter into a standard data sharing agreement with MSD before data access is granted. Data will be made available for request after product approval in the US and European Union or after product development is discontinued. There are circumstances that may prevent MSD from sharing requested data, including country- or region-specific regulations. If the request is declined, it will be communicated to the investigator. Access to genetic or exploratory biomarker data requires a detailed, hypothesis-driven statistical analysis plan that is collaboratively developed by the requester and MSD subject matter experts; after approval of the statistical analysis plan and execution of a data sharing agreement, MSD will either perform the proposed analyses and share the results with the requester or will construct biomarker covariates and add them to a file with clinical data that is uploaded to an analysis portal so that the requester can perform the proposed analyses.
References
DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV (Office of AIDS Research Advisory Council, 2019); https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/AdultandAdolescentGL.pdf
Reynolds, S. J. et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS 25, 473–477 (2011).
Joint United Nations Programme on HIV/AIDS. Fact Sheet 2021 (UNAIDS, 2021); https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
Fonner, V. A. et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS 30, 1973–1983 (2016).
Grant, R. M. et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 363, 2587–2599 (2010).
Baeten, J. M. et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 367, 399–410 (2012).
Owens, D. K. et al. Preexposure prophylaxis for the prevention of HIV infection: US Preventive Services Task Force recommendation statement. JAMA 321, 2203–2213 (2019).
US Public Health Service. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States—2017 Update. A Clinical Practice Guideline (US Public Health Service, 2017); https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf
European AIDS Clinical Society. Guidelines for the Management of People Living with HIV (PLWH) in Europe. Version 10.1 October 2020 (EACS, 2020); https://www.eacsociety.org/files/guidelines-10.1.finalsept2020.pdf
U.S. Food and Drug Administration. Descovy (emtricitabine and tenofovir alafenamide) prescribing Information. https://www.gilead.com/-/media/files/pdfs/medicines/hiv/descovy/descovy_pi.pdf (2021).
Marrazzo, J. M. et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 372, 509–518 (2015).
Gandhi, M. et al. Strong correlation between concentrations of tenofovir (TFV) emtricitabine (FTC) in hair and TFV diphosphate and FTC triphosphate in dried blood spots in the iPrEx Open Label Extension: implications for pre-exposure prophylaxis adherence monitoring. J. Infect. Dis. 212, 1402–1406 (2015).
Liu, A. Y. et al. Strong relationship between oral dose and tenofovir hair levels in a randomized trial: hair as a potential adherence measure for pre-exposure prophylaxis (PrEP). PLoS ONE 9, e83736 (2014).
Riddell, J. 4th, Amico, K. R. & Mayer, K. H. HIV preexposure prophylaxis: a review. JAMA 319, 1261–1268 (2018).
Van Damme, L. et al. Preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 367, 411–422 (2012).
Patterson, K. B. et al. Penetration of tenofovir and emtricitabine in mucosal tissues: implications for prevention of HIV-1 transmission. Sci. Transl. Med. 3, 112re4 (2011).
Cottrell, M. L. et al. A translational pharmacology approach to predicting outcomes of preexposure prophylaxis against HIV in men and women using tenofovir disoproxil fumarate with or without emtricitabine. J. Infect. Dis. 214, 55–64 (2016).
Markowitz, M. & Sarafianos, S. G. 4′-Ethynyl-2-fluoro-2′-deoxyadenosine, MK-8591: a novel HIV-1 reverse transcriptase translocation inhibitor. Curr. Opin. HIV AIDS 13, 294–299 (2018).
Markowitz, M. & Grobler, J. A. Islatravir for the treatment and prevention of infection with the human immunodeficiency virus type 1. Curr. Opin. HIV AIDS 15, 27–32 (2020).
Grobler, J. A. et al. MK-8591 potency and PK provide high inhibitory quotients at low doses QD and QW (CROI abstract 481). CROI https://www.croiconference.org/abstract/mk-8591-potency-and-pk-provide-high-inhibitory-quotients-low-doses-qd-and-qw/ (2019).
Salie, Z. L. et al. Structural basis of HIV inhibition by translocation-defective RT inhibitor 4′-ethynyl-2-fluoro-2′-deoxyadenosine (EFdA). Proc. Natl Acad. Sci. USA 113, 9274–9279 (2016).
Michailidis, E. et al. 4′-Ethynyl-2-fluoro-2′-deoxyadenosine (EFdA) inhibits HIV-1 reverse transcriptase with multiple mechanisms. J. Biol. Chem. 289, 24533–24548 (2014).
Grobler, J. A., Huang, Q., Hazuda, D. & Lai, M. Efficacy of MK-8591 against diverse HIV-1 subtypes and NRTI-resistant clinical isolates. J. Int. AIDS Soc. 21, O343 (2018).
Stoddart, C. A. et al. Oral administration of the nucleoside EFdA (4′-ethynyl-2-fluoro-2′-deoxyadenosine) provides rapid suppression of HIV viremia in humanized mice and favorable pharmacokinetic properties in mice and the rhesus macaque. Antimicrob. Agents Chemother. 59, 4190–4198 (2015).
Grobler, J. A. et al. Long-acting oral and parenteral dosing of MK-8591 for HIV treatment or prophylaxis (CROI abstract 98). CROI https://www.croiconference.org/abstract/long-acting-oral-and-parenteral-dosing-mk-8591-hiv-treatment-or-prophylaxis/ (2016).
Schürmann, D. et al. Safety, pharmacokinetics, and antiretroviral activity of islatravir (ISL, MK-8591), a novel nucleoside reverse transcriptase translocation inhibitor, following single-dose administration to treatment-naive adults infected with HIV-1: an open-label, phase 1b, consecutive-panel trial. Lancet HIV 7, e164–e172 (2020).
Markowitz, M., et al. Weekly oral islatravir provides effective PEP against IV challenge with SIVMAC251 (CROI abstract 89). CROI https://www.croiconference.org/abstract/weekly-oral-islatravir-provides-effective-pep-against-iv-challenge-with-sivmac251/ (2020).
Matthews, R. P. et al. Multiple daily doses of MK-8591 as low as 0.25 mg are expected to suppress HIV. In Special Issue: Abstracts From the 2018 Conference on Retroviruses and Opportunistic Infections. Top. Antivir. Med. 26, abstr. 26 (2018).
Matthews, R. P. et al. Safety, tolerability, and pharmacokinetics of single- and multiple-dose adminstration of islatravir (MK-8591) in adults without HIV. Clin. Transl. Sci. https://doi.org/10.1111/cts.13048 (2021).
Matthews, R. P. et al. Next-generation islatravir implants projected to provide yearly HIV prophylaxis (CROI abstract 88). CROI https://www.croiconference.org/abstract/next-generation-islatravir-implants-projected-to-provide-yearly-hiv-prophylaxis/ (2021).
Daniels, K. & Abma, J. C. Current Contraceptive Status Among Women Aged 15-49: United States, 2017-2019. NCHS Data Brief 388, 1–8 (2020).
Johnson, A. R. et al. Drug eluting implants in pharmaceutical development and clinical practice. Expert Opin. Drug Deliv. 18, 577–593 (2021).
Mansour, D., Inki, P. & Gemzell-Danielsson, K. Efficacy of contraceptive methods: a review of the literature. Eur. J. Contracept. Reprod. Health Care 15, S19–S31 (2010).
Li, L., Johnson, L. M., Krovi, S. A., Demkovich, Z. R. & van der Straten, A. Performance and stability of tenofovir alafenamide formulations within subcutaneous biodegradable implants for HIV pre-exposure prophylaxis (PrEP). Pharmaceutics 12, 1057 (2020).
Gunawardana, M. et al. Multispecies evaluation of a long-acting tenofovir alafenamide subdermal implant for HIV prophylaxis. Front. Pharmacol. 11, 569373 (2020).
Markowitz, M. et al. Once-weekly oral dosing of MK-8591 protects male rhesus macaques from intrarectal challenge with SHIV109CP3. J. Infect. Dis. 221, 1398–1406 (2020).
Barrett, S. E. et al. Extended-duration MK-8591-eluting implant as a candidate for HIV treatment and prevention. Antimicrob. Agents Chemother. 62, e01058-18 (2018).
Adams, K. & Beal, M. W. Implanon: a review of the literature with recommendations for clinical management. J. Midwifery Womens Health 54, 142–149 (2009).
Patel, M. et al. Islatravir PK threshold & dose selection for monthly oral HIV-1 PrEP (CROI abstract 87). CROI https://www.croiconference.org/abstract/islatravir-pk-threshold-dose-selection-for-monthly-oral-hiv-1-prep/ (2021).
Matthews, R. P. First-in-human trial of MK-8591-eluting implants demonstrates concentrations suitable for HIV prophylaxis for at least one year. (IAS abstract 4843) https://programme.ias2019.org/Abstract/Abstract/4843 (2019).
Rudd, D. J. et al. Modeling-supported islatravir dose selection for phase 3 (CROI abstract 462). CROI https://www.croiconference.org/abstract/modeling-supported-islatravir-dose-selection-for-phase-iii/ (2020).
Ramdhan, R. C. et al. Complications of subcutaneous contraception: a review. Cureus 10, e2132 (2018).
U.S. Food and Drug Administration. Nexplanon (etonogestrel implant) prescribing Information. https://www.organon.com/product/usa/pi_circulars/n/nexplanon/nexplanon_pi.pdf (2020).
Coelho, L. E., Torres, T. S., Veloso, V. G., Landovitz, R. J. & Grinsztejn, B. Pre-exposure prophylaxis 2.0: new drugs and technologies in the pipeline. Lancet HIV 6, e788–e799 (2019).
Baeten, J. M. et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N. Engl. J. Med. 375, 2121–2132 (2016).
Delany-Moretlwe, S. et al. Tenofovir 1% vaginal gel for prevention of HIV-1 infection in women in South Africa (FACTS-001): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Infect. Dis. 18, 1241–1250 (2018).
Markowitz, M. et al. Safety and tolerability of long-acting cabotegravir injections in HIV-uninfected men (ECLAIR): a multicentre, double-blind, randomised, placebo-controlled, phase 2a trial. Lancet HIV 4, e331–e340 (2017).
Pons-Faudoa, F. P. et al. 2-Hydroxypropyl-β-cyclodextrin-enhanced pharmacokinetics of cabotegravir from a nanofluidic implant for HIV pre-exposure prophylaxis. J. Control. Release 306, 89–96 (2019).
Johnson, L., Swarner, S. L., Van Der Straten, A. & Rothrock, G. D. Methods for Assessing the Adherence to Medical Devices. Publication No. MR-0036-1610 (RTI Press, 2016).
Cottrell, M. L. et al. Decreased tenofovir diphosphate concentrations in a transgender female cohort: implications for human immunodeficiency virus preexposure prophylaxis. Clin. Infect. Dis. 69, 2201–2204 (2019).
Acknowledgements
Funding for this research was provided by Merck Sharp & Dohme (MSD), a subsidiary of Merck & Co. We thank the participants and clinical research staff who participated in this trial. MSD pharmacokinetics, pharmacodynamics and drug metabolism scientists (L. Sun, I. Xie, B. Lu, R. Valesky, M. Lyman, K. Fillgrove and M. Anderson) and early clinical scientists (V. Weissler and G. Chen) are acknowledged for their contribution to the study. Additional statistical support was provided by Y. Liu (MSD). Medical writing and/or editorial assistance was provided by Y.-M. Ching in accordance with good publication practice guidelines. This assistance was funded by MSD.
Author information
Authors and Affiliations
Contributions
R.P.M., M.P., J.A.G., S.E.B. and S.Z. conceived and designed the overall trial. The trial was overseen by R.P.M., S.R., L.H., T.R., S.A.S. and M.I. S.R. collected the clinical data. A.G. conducted the in vitro characterization. R.P.M., M.P. and S.Z. analyzed the data. R.P.M., M.P., S.Z., R.C.V. and M.I. interpreted the data. All authors had full access to the raw data, performed all the analyses, prepared the manuscript and were responsible for the decision to submit for publication. All authors vouch for the completeness and accuracy of the data.
Corresponding author
Ethics declarations
Competing interests
R.P.M., M.P., S.E.B., L.H., T.R., S.Z., A.G., R.C.V., J.A.G., S.A.S. and M.I. were current or former employees of MSD when the study was conducted. S.R. declares no competing interests.
Additional information
Peer review information Nature Medicine thanks Douglas Richman and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Alison Farrell was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Table 1, Fig. 1 and Study Protocol.
Rights and permissions
About this article
Cite this article
Matthews, R.P., Patel, M., Barrett, S.E. et al. Safety and pharmacokinetics of islatravir subdermal implant for HIV-1 pre-exposure prophylaxis: a randomized, placebo-controlled phase 1 trial. Nat Med 27, 1712–1717 (2021). https://doi.org/10.1038/s41591-021-01479-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01479-3
This article is cited by
-
Incorporating end-users’ voices into the development of an implant for HIV prevention: a discrete choice experiment in South Africa and Zimbabwe
BMC Women's Health (2023)
-
Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems
Nature Reviews Drug Discovery (2023)
-
Preclinical Considerations for Long-acting Delivery of Tenofovir Alafenamide from Subdermal Implants for HIV Pre-exposure Prophylaxis
Pharmaceutical Research (2023)
-
Current State and Opportunities with Long-acting Injectables: Industry Perspectives from the Innovation and Quality Consortium “Long-Acting Injectables” Working Group
Pharmaceutical Research (2023)
-
Novel and Investigational HIV Therapies for Treatment and Prevention: Focus on Cabotegravir, Islatravir, and Lenacapavir
Current Infectious Disease Reports (2022)