Abstract
Background
Bicuspid aortic valve may be associated with increased complications during transcatheter aortic valve implantation (TAVI).
Aims
Compare balloon-expandable transcatheter heart valve (THV) safety and efficacy in severe tricuspid (TAV) and bicuspid (BAV) aortic stenosis.
Methods
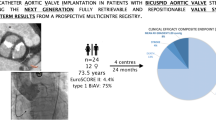
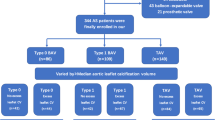
Transfemoral TAVI was performed in 743 patients (Jan 2014–June 2019) using the SAPIEN 3 THV. Aortic valve morphology was determined using computed tomography. Valve Academic Research Consortium-2 (VARC-2) derived safety and efficacy endpoints at 1 year were evaluated.
Results
BAV patients (n = 78), were younger (77 [72, 81] vs. 81 [78, 85] years, p < 0.001) with lower surgical risk (EuroSCORE II 2.96% vs. 4.51% p < 0.001). Bicuspid valves were more calcified (BAV 1308mm3, TAV 848mm3 p < 0.001) with more asymmetric calcification (BAV 63/78 (81%), TAV 239/665 (36%), p < 0.001). Device success (BAV 94%, TAV 90%, p = 0.45) and major vascular complications (BAV 6%, TAV 9%, p = 0.66) were comparable. At 1 year, there was a trend toward lower combined all-cause mortality and rehospitalization for congestive heart failure in BAV patients (BAV 7%, TAV 13%, p = 0.08) with significantly lower all-cause mortality in this cohort (BAV 1%, TAV 9%, p = 0.020). VARC-2 time-related valve safety (BAV 22%, TAV 20%, p = 0.60) was comparable; however, bioprosthetic valve thrombosis remained more common in BAV patients (BAV 7%, TAV 2%, p = 0.010, Hazard ratio 3.57 [95% confidence interval 1.26, 10.10]). After propensity score matching, only bioprosthetic valve thrombosis remained significantly different.
Conclusions
Safety and efficacy of the SAPIEN 3 balloon-expandable THV in BAV is comparable with TAV. Higher rates of bioprosthetic valve thrombosis require further investigation.
Graphic abstract





Similar content being viewed by others
Availability of data and materials
For data privacy reasons, original data not available.
Abbreviations
- THV:
-
Transcatheter heart valve
- BAV:
-
Bicuspid aortic valve
- TAV:
-
Tricuspid aortic valve
- TAVI:
-
Transcatheter aortic valve implantation
- VARC-2:
-
Valve academic research consortium-2
- MDCT:
-
Multi-detector computed tomography
- IQR:
-
Interquartile range
- BMI:
-
Body mass index
- TIA:
-
Transient ischemic attack
- LVEF:
-
Left ventricular ejection fraction
- CV:
-
Calcium volume
- CI:
-
Confidence interval
- NYHA:
-
New York heart association
- BVT:
-
Bioprosthetic valve thrombosis
- SAVR:
-
Surgical aortic valve replacement
- RIFLE:
-
Risk, injury, failure, loss of kidney function, and end-stage kidney disease
References
Siu SC, Silversides CK (2010) Bicuspid aortic valve disease. J Am Coll Cardiol 55:2789–2800
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39:1890–1900
Horstkotte D, Loogen F (1988) The natural history of aortic valve stenosis. Eur Heart J 9 Suppl E:57–64
Sabet HY, Edwards WD, Tazelaar HD, Daly RC (1999) Congenitally bicuspid aortic valves: a surgical pathology study of 542 cases (1991 through 1996) and a literature review of 2,715 additional cases. Mayo Clin Proc 74:14–26
Philip F, Faza NN, Schoenhagen P, Desai MY, Tuzcu EM, Svensson LG, Kapadia SR (2015) Aortic annulus and root characteristics in severe aortic stenosis due to bicuspid aortic valve and tricuspid aortic valves: implications for transcatheter aortic valve therapies. Catheter Cardiovasc Interv 86:E88-98
Roberts WC, Ko JM (2005) Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation 111:920–925
Mahadevia R, Barker AJ, Schnell S, Entezari P, Kansal P, Fedak PW, Malaisrie SC, McCarthy P, Collins J, Carr J, Markl M (2014) Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation 129:673–682
Perlman GY, Blanke P, Dvir D, Pache G, Modine T, Barbanti M, Holy EW, Treede H, Ruile P, Neumann FJ, Gandolfo C, Saia F, Tamburino C, Mak G, Thompson C, Wood D, Leipsic J, Webb JG (2016) Bicuspid aortic valve stenosis: favorable early outcomes with a next-generation transcatheter heart valve in a multicenter study. J Am Coll Cardiol Intv 9:817–824
Isner JM, Chokshi SK, DeFranco A, Braimen J, Slovenkai GA (1990) Contrasting histoarchitecture of calcified leaflets from stenotic bicuspid versus stenotic tricuspid aortic valves. J Am Coll Cardiol 15:1104–1108
Yoon SH, Kim WK, Dhoble A, Milhorini Pio S, Babaliaros V, Jilaihawi H, Pilgrim T, De Backer O, Bleiziffer S, Vincent F, Shmidt T, Butter C, Kamioka N, Eschenbach L, Renker M, Asami M, Lazkani M, Fujita B, Birs A, Barbanti M, Pershad A, Landes U, Oldemeyer B, Kitamura M, Oakley L, Ochiai T, Chakravarty T, Nakamura M, Ruile P, Deuschl F, Berman D, Modine T, Ensminger S, Kornowski R, Lange R, McCabe JM, Williams MR, Whisenant B, Delgado V, Windecker S, Van Belle E, Sondergaard L, Chevalier B, Mack M, Bax JJ, Leon MB, Makkar RR (2020) Bicuspid AVSTAVRRI. Bicuspid aortic valve morphology and outcomes after transcatheter aortic valve replacement. J Am Coll Cardiol 76:1018–1030
Praz F, Windecker S, Huber C, Carrel T, Wenaweser P (2015) Expanding indications of transcatheter heart valve interventions. J Am Coll Cardiol Intv 8:1777–1796
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Brown DL, Block PC, Guyton RA, Pichard AD, Bavaria JE, Herrmann HC, Douglas PS, Petersen JL, Akin JJ, Anderson WN, Wang D, Pocock S, PARTNER TI (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, Williams M, Dewey T, Kapadia S, Babaliaros V, Thourani VH, Corso P, Pichard AD, Bavaria JE, Herrmann HC, Akin JJ, Anderson WN, Wang D, Pocock SJ, PARTNER TI (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364:2187–2198
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, Thourani VH, Tuzcu EM, Miller DC, Herrmann HC, Doshi D, Cohen DJ, Pichard AD, Kapadia S, Dewey T, Babaliaros V, Szeto WY, Williams MR, Kereiakes D, Zajarias A, Greason KL, Whisenant BK, Hodson RW, Moses JW, Trento A, Brown DL, Fearon WF, Pibarot P, Hahn RT, Jaber WA, Anderson WN, Alu MC, Webb JG, PARTNER I (2016) Transcatheter or Surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 374:1609–1620
Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Søndergaard L, Mumtaz M, Adams DH, Deeb GM, Maini B, Gada H, Chetcuti S, Gleason T, Heiser J, Lange R, Merhi W, Oh JK, Olsen PS, Piazza N, Williams M, Windecker S, Yakubov SJ, Grube E, Makkar R, Lee JS, Conte J, Vang E, Nguyen H, Chang Y, Mugglin AS, Serruys PW, Kappetein AP, SURTAVI I (2017) Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med 376:1321–1331
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P (2019) Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 380:1695–1705
Yoon SH, Bleiziffer S, De Backer O, Delgado V, Arai T, Ziegelmueller J, Barbanti M, Sharma R, Perlman GY, Khalique OK, Holy EW, Saraf S, Deuschl F, Fujita B, Ruile P, Neumann FJ, Pache G, Takahashi M, Kaneko H, Schmidt T, Ohno Y, Schofer N, Kong WKF, Tay E, Sugiyama D, Kawamori H, Maeno Y, Abramowitz Y, Chakravarty T, Nakamura M, Kuwata S, Yong G, Kao HL, Lee M, Kim HS, Modine T, Wong SC, Bedgoni F, Testa L, Teiger E, Butter C, Ensminger SM, Schaefer U, Dvir D, Blanke P, Leipsic J, Nietlispach F, Abdel-Wahab M, Chevalier B, Tamburino C, Hildick-Smith D, Whisenant BK, Park SJ, Colombo A, Latib A, Kodali SK, Bax JJ, Søndergaard L, Webb JG, Lefèvre T, Leon MB, Makkar R (2017) Outcomes in transcatheter aortic valve replacement for bicuspid versus tricuspid aortic valve stenosis. J Am Coll Cardiol 69:2579–2589
Mylotte D, Lefevre T, Søndergaard L, Watanabe Y, Modine T, Dvir D, Bosmans J, Tchetche D, Kornowski R, Sinning JM, Thériault-Lauzier P, O’Sullivan CJ, Barbanti M, Debry N, Buithieu J, Codner P, Dorfmeister M, Martucci G, Nickenig G, Wenaweser P, Tamburino C, Grube E, Webb JG, Windecker S, Lange R, Piazza N (2014) Transcatheter aortic valve replacement in bicuspid aortic valve disease. J Am Coll Cardiol 64:2330–2339
Costopoulos C, Latib A, Maisano F, Testa L, Bedogni F, Buchanan L, Naganuma T, Sticchi A, Sato K, Miyazaki T (2014) Comparison of results of transcatheter aortic valve implantation in patients with severely stenotic bicuspid versus tricuspid or nonbicuspid valves. Am J Cardiol 113:1390–1393
Jilaihawi H, Chen M, Webb J, Himbert D, Ruiz CE, Rodés-Cabau J, Pache G, Colombo A, Nickenig G, Lee M, Tamburino C, Sievert H, Abramowitz Y, Tarantini G, Alqoofi F, Chakravarty T, Kashif M, Takahashi N, Kazuno Y, Maeno Y, Kawamori H, Chieffo A, Blanke P, Dvir D, Ribeiro HB, Feng Y, Zhao ZG, Sinning JM, Kliger C, Giustino G, Pajerski B, Imme S, Grube E, Leipsic J, Vahanian A, Michev I, Jelnin V, Latib A, Cheng W, Makkar R (2016) A bicuspid aortic valve imaging classification for the TAVR Era. J Am Coll Cardiol Img 9:1145–1158
Forrest JK, Kaple RK, Ramlawi B, Gleason TG, Meduri CU, Yakubov SJ, Jilaihawi H, Liu F, Reardon MJ (2020) Transcatheter aortic valve replacement in bicuspid versus tricuspid aortic valves from the STS/ACC TVT registry. J Am Coll Cardiol Intv 13:1749–1759
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es GA, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodés-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the valve academic research consortium-2 consensus document. Eur Heart J 33:2403–2418
Erlebach M, Head SJ, Mylotte D, Leon MB, Serruys PW, Kappetein AP, Martucci G, Genereux P, Windecker S, Lange R, Piazza N (2016) VARC endpoint definition compliance rates in contemporary transcatheter aortic valve implantation studies. EuroIntervention 12:375–380
Zhang S, Kolominsky-Rabas PL (2017) How TAVI registries report clinical outcomes-A systematic review of endpoints based on VARC-2 definitions. PLoS ONE 12:e0180815
Frangieh AH, Ott I, Michel JM, Shivaraju A, Joner M, Mayr NP, Hengstenberg C, Husser O, Pellegrini C, Schunkert H, Kastrati A, Kasel AM (2017) Standardized minimalistic transfemoral transcatheter aortic valve replacement (TAVR) Using the SAPIEN 3 device: stepwise description, feasibility, and safety from a large consecutive single-center single-operator cohort. Structural Heart 1(3–4):169–178. https://doi.org/10.1080/24748706.2017.1358832
Sievers HH, Schmidtke C (2007) A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg 133:1226–1233
Kim WK, Renker M, Rolf A, Liebetrau C, Van Linden A, Arsalan M, Doss M, Rieck J, Opolski MP, Möllmann H, Walther T, Hamm CW (2018) Accuracy of device landing zone calcium volume measurement with contrast-enhanced multidetector computed tomography. Int J Cardiol 263:171–176
Kasel AM, Cassese S, Leber AW, von Scheidt W, Kastrati A (2013) Fluoroscopy-guided aortic root imaging for TAVR: “follow the right cusp” rule. [letter]. J Am Coll Cardiol Img 6(2):274–275
Kasel AM, Shivaraju A, von Scheidt W, Kastrati A, Thilo C (2015) Anatomic guided crossing of a stenotic aortic valve under fluoroscopy: “right cusp rule, part III.”[letter]. J Am Coll Cardiol Intv 8(1 Pt A):119–120
Frangieh AH, Kasel AM (2017) TAVI in bicuspid aortic valves ‘made easy.’ Eur Heart J 38:1177–1181
Husser O, Pellegrini C, Kessler T, Burgdorf C, Thaller H, Mayr NP, Kasel AM, Kastrati A, Schunkert H, Hengstenberg C (2016) Predictors of permanent pacemaker implantations and new-onset conduction abnormalities with the SAPIEN 3 balloon-expandable transcatheter heart valve. J Am Coll Cardiol Intv 9:244–254
Kronzon I, Jelnin V, Ruiz CE, Saric M, Williams MR, Kasel AM, Shivaraju A, Colombo A, Kastrati A (2015) Optimal imaging for guiding TAVR: transesophageal or transthoracic echocardiography, or just fluoroscopy. J Am Coll Cardiol Img 8:361–370
Popma JJ, Deeb GM, Yakubov SJ, Mumtaz M, Gada H, O’Hair D, Bajwa T, Heiser JC, Merhi W, Kleiman NS (2019) Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 380:1706–1715
Himbert D, Pontnau F, Messika-Zeitoun D, Descoutures F, Détaint D, Cueff C, Sordi M, Laissy JP, Alkhoder S, Brochet E, Iung B, Depoix JP, Nataf P, Vahanian A (2012) Feasibility and outcomes of transcatheter aortic valve implantation in high-risk patients with stenotic bicuspid aortic valves. Am J Cardiol 110:877–883
Kochman J, Huczek Z, Ścisło P, Dabrowski M, Chmielak Z, Szymański P, Witkowski A, Parma R, Ochala A, Chodór P (2014) Comparison of one-and 12-month outcomes of transcatheter aortic valve replacement in patients with severely stenotic bicuspid versus tricuspid aortic valves (results from a multicenter registry). Am J Cardiol 114:757–762
Phan K, Wong S, Phan S, Ha H, Qian P, Yan TD (2015) Transcatheter aortic valve implantation (tavi) in patients with bicuspid aortic valve stenosis-systematic review and meta-analysis. Heart Lung Circ 24:649–659
Xie X, Shi X, Xun X, Rao L (2016) Efficacy and safety of transcatheter aortic valve implantation for bicuspid aortic valves: a systematic review and meta-analysis. Ann Thorac Cardiovasc Surg 22:203–215
Bauer T, Linke A, Sievert H, Kahlert P, Hambrecht R, Nickenig G, Hauptmann KE, Sack S, Gerckens U, Schneider S, Zeymer U, Zahn R (2014) Comparison of the effectiveness of transcatheter aortic valve implantation in patients with stenotic bicuspid versus tricuspid aortic valves (from the German TAVI Registry). Am J Cardiol 113:518–521
Zhao ZG, Jilaihawi H, Feng Y, Chen M (2015) Transcatheter aortic valve implantation in bicuspid anatomy. Nat Rev Cardiol 12:123–128
Yoon SH, Lefèvre T, Ahn JM, Perlman GY, Dvir D, Latib A, Barbanti M, Deuschl F, De Backer O, Blanke P, Modine T, Pache G, Neumann FJ, Ruile P, Arai T, Ohno Y, Kaneko H, Tay E, Schofer N, Holy EW, Luk NHV, Yong G, Lu Q, Kong WKF, Hon J, Kao HL, Lee M, Yin WH, Park DW, Kang SJ, Lee SW, Kim YH, Lee CW, Park SW, Kim HS, Butter C, Khalique OK, Schaefer U, Nietlispach F, Kodali SK, Leon MB, Ye J, Chevalier B, Leipsic J, Delgado V, Bax JJ, Tamburino C, Colombo A, Søndergaard L, Webb JG, Park SJ (2016) Transcatheter aortic valve replacement with early- and new-generation devices in bicuspid aortic valve stenosis. J Am Coll Cardiol 68:1195–1205
Forrest JK, Ramlawi B, Deeb GM, Zahr F, Song HK, Kleiman NS, Chetcuti SJ, Michelena HI, Mangi AA, Skiles JA, Huang J, Popma JJ, Reardon MJ (2021) Transcatheter aortic valve replacement in low-risk patients with bicuspid aortic valve stenosis. JAMA Cardiol. 6(1):50–57
Makkar RR, Yoon SH, Leon MB, Chakravarty T, Rinaldi M, Shah PB, Skipper ER, Thourani VH, Babaliaros V, Cheng W, Trento A, Vemulapalli S, Kapadia SR, Kodali S, Mack MJ, Tang GHL, Kaneko T (2019) Association between transcatheter aortic valve replacement for bicuspid vs tricuspid aortic stenosis and mortality or stroke. JAMA 321:2193–2202
Halim SA, Edwards FH, Dai D, Li Z, Mack MJ, Holmes DR, Tuzcu EM, Thourani VH, Harrison JK, Brennan JM (2020) Outcomes of transcatheter aortic valve replacement in patients with bicuspid aortic valve disease: a report from the society of thoracic surgeons/american college of cardiology transcatheter valve therapy registry. Circulation 141:1071–1079
Pollari F, Hitzl W, Vogt F, Cuomo M, Schwab J, Söhn C, Kalisnik JM, Langhammer C, Bertsch T, Fischlein T, Pfeiffer S (2020) Aortic valve calcification as a risk factor for major complications and reduced survival after transcatheter replacement. J Cardiovasc Comput Tomogr 14:307–313
Pellegrini C, Rheude T, Trenkwalder T, Mayr NP, Joner M, Kastrati A, Schunkert H, Husser O, Hengstenberg C (2019) One year VARC-2-defined clinical outcomes after transcatheter aortic valve implantation with the SAPIEN 3. Clin Res Cardiol 108:1258–1265
Webb JG, Mack MJ, White JM, Dvir D, Blanke P, Herrmann HC, Leipsic J, Kodali SK, Makkar R, Miller DC, Pibarot P, Pichard A, Satler LF, Svensson L, Alu MC, Suri RM, Leon MB (2017) Transcatheter aortic valve implantation within degenerated aortic surgical bioprostheses: PARTNER 2 valve-in-valve registry. J Am Coll Cardiol 69:2253–2262
Latib A, Naganuma T, Abdel-Wahab M, Danenberg H, Cota L, Barbanti M, Baumgartner H, Finkelstein A, Legrand V, de Lezo JS, Kefer J, Messika-Zeitoun D, Richardt G, Stabile E, Kaleschke G, Vahanian A, Laborde JC, Leon MB, Webb JG, Panoulas VF, Maisano F, Alfieri O, Colombo A (2015) Treatment and clinical outcomes of transcatheter heart valve thrombosis. Circ Cardiovasc Interv 8(4):e001779. https://doi.org/10.1161/CIRCINTERVENTIONS.114.001779
Del Trigo M, Muñoz-Garcia AJ, Wijeysundera HC, Nombela-Franco L, Cheema AN, Gutierrez E, Serra V, Kefer J, Amat-Santos IJ, Benitez LM, Mewa J, Jiménez-Quevedo P, Alnasser S, Garcia del Blanco B, Dager A, Abdul-Jawad Altisent O, Puri R, Campelo-Parada F, Dahou A, Paradis J-M, Dumont E, Pibarot P, Rodés-Cabau J (2016) Incidence, timing, and predictors of valve hemodynamic deterioration after transcatheter aortic valve replacement. J Am Coll Cardiol 67:644–655
Jose J, Sulimov DS, El-Mawardy M, Sato T, Allali A, Holy EW, Becker B, Landt M, Kebernik J, Schwarz B, Richardt G, Abdel-Wahab M (2017) Clinical bioprosthetic heart valve thrombosis after transcatheter aortic valve replacement: incidence, characteristics, and treatment outcomes. J Am Coll Cardiol Intv 10:686–697
Rheude T, Pellegrini C, Stortecky S, Marwan M, Xhepa E, Ammon F, Pilgrim T, Mayr NP, Husser O, Achenbach S, Windecker S, Cassese S, Joner M (2021) Meta-analysis of bioprosthetic valve thrombosis after transcatheter aortic valve implantation. Am J Cardiol 138:92–99
D’Ascenzo F, Salizzoni S, Saglietto A, Cortese M, Latib A, Franzone A, Barbanti M, Nietlispach F, Holy EW, Burriesci G, De Paoli A, Fonio P, Atzeni F, Moretti C, Perl L, D’Amico M, Rinaldi M, Conrotto F (2019) Incidence, predictors and cerebrovascular consequences of leaflet thrombosis after transcatheter aortic valve implantation: a systematic review and meta-analysis. Eur J Cardiothorac Surg 56:488–494
Funding
This study did not receive external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AHF is a proctor and medical consultant for Edwards Lifesciences. AMK is a proctor and medical consultant for and receives research support from Edwards Lifesciences. BES receives research support from Boston Scientific and Edwards Lifesciences.
Ethics approval
Prospective database approval provided by local ethics board (Technical University Munich).
Consent to participate
Patients provided consent for the procedure.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Michel, J.M., Frangieh, A.H., Giacoppo, D. et al. Safety and efficacy of minimalist transcatheter aortic valve implantation using a new-generation balloon-expandable transcatheter heart valve in bicuspid and tricuspid aortic valves. Clin Res Cardiol 110, 1993–2006 (2021). https://doi.org/10.1007/s00392-021-01935-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01935-7