Abstract
Atrial fibrillation (AF) is a major cause of cardiovascular morbidity and mortality. To early detect and to avoid AF-related complications, several cardiac imaging modalities and approaches aim to quantify the severity of the underlying atrial cardiomyopathy (i.e., the extent of atrial remodeling). However, most established cardiac imaging modalities just incorporate single components of atrial remodeling and do not reflect the complete multifactorial process, which may contribute to their limited predictive value. Echocardiography-derived PA-TDI duration is a sophisticated echocardiographic parameter to assess total atrial conduction time and directly reflects both electrical and structural changes to the atria. Therefore, PA-TDI duration provides a more comprehensive quantification of the extent of atrial remodeling than other imaging modalities. In this article we review the role of PA-TDI duration as a marker of atrial remodeling and summarize the available data on PA-TDI duration to identify patients at risk for AF, as well as to guide AF management. Moreover, we discuss how to assess PA-TDI duration and provide recommendations on the implementation of PA-TDI duration into routine clinical care.
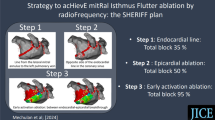
Graphic abstract

Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia in clinical practice and affects more than 6 million people in Europe [1]. AF is often the result of an underlying atrial cardiomyopathy that can be caused by a variety of diseases and concomitant risk factors (e.g., hypertension, obstructive sleep apnea and obesity) that lead to structural (e.g., fibrosis) and electrical changes (e.g., ion channel alterations) to the atria: atrial remodeling [2, 3]. Subsequent clinical manifestations of atrial remodeling can be morphological, electrical and/or functional (Fig. 1) [4, 5].
Role of PA-TDI duration in the visualization of atrial cardiomyopathy. The PA-TDI duration is associated with several conditions that can cause atrial cardiomyopathy. Moreover, the PA-TDI duration reflects the extent of atrial fibrosis, one of the processes involved in atrial cardiomyopathy. Finally, the PA-TDI duration allows direct assessment of both electrical and anatomical manifestations of atrial cardiomyopathy by estimating the total atrial conduction time and is strongly associated with the functional manifestations such left atrial (LA) dysfunction. AF atrial fibrillation
Quantification of the extent of atrial remodeling is considered the key to predict the development and progression of AF, the response to AF treatment and the risk for AF related complications. However, most imaging modalities that are used to quantify atrial remodeling fail to capture more than one clinical manifestation of this process, thereby limiting their predictive value.
Echocardiography derived total atrial conduction time is a marker of atrial remodeling that reflects both morphological (atrial size) and electrical (conduction velocity) manifestations [6]. Total atrial conduction time is measured during sinus rhythm as the time interval from the beginning of the P-wave on the surface electrocardiogram (ECG) to the peak A’-wave on the Tissue-Doppler Imaging (TDI) tracing of the lateral left atrial (LA) wall on echocardiography: PA-TDI duration. The PA-TDI duration reflects the time needed for the atrial depolarization to conduct from the sinus node through the atrial tissue to the LA lateral wall and to result in an active contraction as measured with TDI. Measurement of the PA-TDI duration provides a more comprehensive estimation of the extent of atrial remodeling than other parameters [7].
Here, we review the role of the PA-TDI duration as a marker of atrial remodeling and summarize the available data on PA-TDI duration to detect patients at risk for AF, to guide AF treatment and monitor the effect of risk factor modification on the left atrial substrate. Importantly, we discuss how to assess PA-TDI duration and provide recommendations on the implementation of PA-TDI duration into routine clinical care.
Echocardiographic assessment
The PA-TDI duration is measured from ECG-gated pulse-wave TDI recordings of the apical four-chamber view using two-dimensional transthoracic echocardiography. Settings are optimized for the highest framerate as possible (at least > 115 frames/s, corresponding to a temporal resolution of 8.7 ms or smaller). A region of interest marker is placed at the LA lateral wall just above the mitral annulus providing the tracing of the mechanical activation in that area (Fig. 2). The PA-TDI duration is measured during sinus rhythm as the time interval from the onset of the P-wave in lead II of the surface ECG (start of electrical depolarization) to the peak A’-wave on the tissue Doppler tracing of the LA lateral wall (active atrial contraction).
Validation and determinants of PA-TDI duration
The use of PA-TDI duration to estimate total atrial conduction time has been validated by Merckx et al. using P-wave duration (PWD) on the signal-averaged ECG as the ‘gold standard’ (R = 0.911, p < 0.001) [6]. PWD in this study was measured as the time-interval between the onset and the offset of the P-wave (defined as the junction between the isoelectric line and the beginning of the P-wave deflection and the junction between the end of the P-wave deflection and the isoelectric line, respectively). Importantly, the authors found that assessment of PA-TDI duration was less time-consuming compared to measurement of PWD using signal-averaged ECG (1.0 ± 0.5 min vs 20 ± 5.0 min, respectively, p < 0.01).
Histological validation of PA-TDI duration to assess atrial remodeling was provided by Müller et al. who demonstrated the correlation between PA-TDI duration and the degree of atrial fibrosis inside the right atrial appendage, one of the hallmark processes involved in atrial remodeling [8]. In addition, various studies have demonstrated the prognostic impact of PA-TDI duration on the occurrence of new-onset AF, postoperative AF and AF recurrence after cardioversion or ablation, thereby implicitly strengthening its validity [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25].
The PA-TDI duration is strongly influenced by factors that play a role in atrial remodeling (Fig. 1). In a group of 386 patients without structural heart disease, Abou et al. demonstrated that PA-TDI duration increases across all age categories, reflecting an age-related component of atrial remodeling [26]. These results are in agreement with work from Weijs et al. and Leung et al. who found a similar age-related impact on PA-TDI duration [27, 28]. Furthermore, Weijs et al. demonstrated that PA-TDI duration increases in the presence of hypertension, a history of AF, a higher body mass index and valvular disease [27]. Similarly, Chao et al. demonstrated that the PA-TDI duration significantly increases across the different stages of diastolic dysfunction [29]. The impact of obstructive sleep apnea on PA-TDI duration has been demonstrated by Müller et al. [30]. In this study the PA-TDI duration was higher in patients with obstructive sleep apnea compared to controls (131.4 ± 16.0 ms vs 120.0 ± 6.4 ms, p < 0.001). Furthermore, after effective treatment with continuous positive airway pressure therapy, which is one of the mainstay treatment options for obstructive sleep apnea patients [31], the PA-TDI duration decreased with a mean delta of 6.4 ± 5.7 ms [30]. This observation demonstrates the dynamic character of atrial remodeling as well as the potential positive impact of preventive measures. Moreover, it underlines the value of PA-TDI duration to capture these changes.
The PA-TDI duration shows a close correlation to conventional echocardiographic indices of atrial remodeling. Weijs et al. demonstrated that PA-TDI duration is associated with left atrial dilatation (i.e., larger LA diameter is associated with a longer PA-TDI duration) [27]. However, the same authors also demonstrated that in a group of patients with idiopathic AF a similar LA volume index was found compared to a group of healthy controls, whereas PA-TDI duration was prolonged, reflecting a preclinical underlying disease [32]. In addition, Abou et al. found that PA-TDI duration was inversely related to LA reservoir strain, reflecting a reduced LA compliance [26]. These observations were confirmed in a large study by Leung et al. comprising of 602 patients with AF and 342 controls, that demonstrated that a longer PA-TDI duration was associated with a larger LA volume index (higher extent of left atrial dilatation) and a reduced LA reservoir strain (reduced LA compliance or increased stiffness) [28].
Clinical applications
Prediction of new-onset AF
AF is associated with a higher cardiovascular morbidity and mortality, and timely identification of AF may help to avoid complications and improve outcome [33,34,35]. There is a considerable amount of data demonstrating the value of PA-TDI duration to predict the development of new-onset AF (Table 1A). Different studies have demonstrated that PA-TDI duration consistently and accurately predicts new-onset AF (1) in a general cardiology population; (2) in patients with heart failure; (3) after myocardial infarction; (4) in congenital heart disease; (5) in end-stage renal disease; (6) in patients with cryptogenic stroke; and (7) in patients with hypertrophic cardiomyopathy [11,12,13, 20, 21, 24, 25].
Post-operative AF
Post-operative AF (POAF) is the most common sustained arrhythmia after cardiac surgery and is associated with an increased morbidity and mortality as well as prolonged in-hospital stay [36]. Pre-operative identification of patients at a high risk of POAF may help to guide pharmacological prophylaxis and reduce complications. Five studies have consistently shown that PA-TDI duration can be used to identify patients at high risk of POAF (Table 1B) [8, 18, 19, 22, 23]. Of note, PA-TDI duration was longer in patients after aortic valve replacement or mitral-valve surgery than in patients after bypass surgery only possibly reflecting valvulopathy related atrial remodeling.
AF recurrence after rhythm control interventions
Antiarrhythmic drugs, electrical cardioversion and catheter ablation are the cornerstones of rhythm control therapy of AF. Despite significant advancement of these therapies, AF recurrence rates are high [37]. Age, co-morbidities and AF duration before restoration of sinus rhythm predispose an atrial remodeling process and leads to both the progression of AF and recurrence of AF after interventions for rhythm control strategies [4, 5, 38]. Overall, eight studies have looked at PA-TDI duration as a predictor of AF recurrence (Table 1C, D) [7, 9, 10, 14,15,16,17]. To summarize, four studies with 262 patients and four studies with 550 patients analyzed the predictive value of PA-TDI duration for AF recurrence after successful electrical cardioversion and catheter ablation, respectively. Of note, all these studies demonstrated the ability of PA-TDI duration to predict AF recurrence.
Assessment of thromboembolic risk
AF predisposes patients to a fivefold increased risk of ischemic stroke [35]. Thus, individual thromboembolic risk stratification is desirable to identify candidates which most benefit of oral anticoagulation therapy. Recently, Leung and colleagues investigated the association between PA-TDI duration and ischemic stroke in 1361 patients with first diagnosis of AF [39]. Assessment of LA reservoir strain and PA-TDI duration on echocardiography after initial CHA2DS2-VASc scoring provides improved risk stratification for stroke over a mean of 7.9 years, especially for the low-to-intermediate risk groups. Importantly, PA-TDI duration was the strongest echocardiographic predictor of stroke in this study.
Comparison to conventional echocardiography
Echocardiography is commonly used to quantify atrial remodeling by measurement of LA size and function. LA size and function have proven to be an important predictor of AF related outcome [38,39,40]. However, measurement of LA size using standard two-dimensional echocardiography is less accurate than with three-dimensional imaging modalities, such as MRI or CT: The shape of the LA is often asymmetrical, making it more difficult for two-dimensional imaging echocardiography to accurately assess true LA volume [41]. This limits the clinical applicability of echocardiography derived volumetric measurement, such as LA size and function, to predict AF related outcome. This is illustrated by the fact that PA-TDI duration has consistently demonstrated to be a stronger predictor of AF related outcome than LA size and function [7,8,9,10,11,12, 14,15,16,17,18,19,20,21,22,23].
A more sophisticated echocardiographic parameter that does not rely on volumetric measurements to quantify atrial remodeling is LA strain. LA strain uses Speckle tracking tissue deformation analysis to assess global LA function and has proven to be an independent predictor of AF related outcome [42]. However, LA strain analyses require time-consuming offline post-processing by manual adjustment of tracing of the LA borders [43]. This limits the routine use of LA strain in clinical practice and its reproducibility. Importantly, Leung et al. demonstrated that although LA reservoir strain was a predictor of stroke in patients with AF, PA-TDI duration was a stronger predictor than LA strain [39].
Measurement of PA-TDI duration is angle-independent and the TDI-tracings have a high temporal resolution (i.e., a high framerate compared to 2D echocardiography and strain analyses). Moreover, the PA-TDI duration can be measured directly on the echo machine and does not require time-consuming offline post-processing and has a low intra- and interobserver variability.
Clinical implementation
The PA-TDI duration can be assessed on each echocardiographic machine with the ability to record TDI with ECG-gating. Therefore, this technique is widely available and easy to introduce into clinical practice. However, there are some challenges that need to be overcome. Currently, no normal values for PA-TDI duration have been established. There seems to be a large variation in values for PA-TDI duration across the different studies (Table 1A–D). Although no head-to-head comparisons were made, there is a significant difference in mean PA-TDI duration in studies using a Philips system compared to a GE system (145.1 ± 21.7 ms vs 126.4 ± 26.3 ms, respectively, p < 0.0001). Most likely, this could be explained by a different time delay between the ECG-signal and the echo-signal across the two systems [44]. In addition, the variation in the values for PA-TDI duration can be partly attributed to the different patient populations that were studied. Importantly, despite these variations, studies consistently demonstrated a very low intra-observer variability (range 1.6–1.8 ms) and inter-observer variability (range 1.7–2.6 ms) in PA-TDI duration measurement, underlining the high degree of reproducibility [7, 11, 12, 28]. Altogether, it seems reasonable that for clinical implementation of PA-TDI duration, each echocardiography laboratory must establish its own normal values and cutoff values, specific for their population and ultrasound system. In addition, P-wave duration on signal-averaged ECG can be used to calibrate and validate laboratory specific measurements.
Discussion
Quantification of atrial remodeling is considered the key to predict the development of AF, the response to rhythm control therapies and the occurrence of AF related complications. The PA-TDI duration is an echocardiography-derived parameter that can be used to quantify the severity of atrial remodeling [6]. The advantage of PA-TDI duration over other parameters is that it combines electrical as well as morphological manifestations of atrial remodeling and, therefore, provides a more comprehensive assessment of atrial remodeling. However, PA-TDI duration does not capture all manifestations of atrial remodeling. For example, PA-TDI duration holds no information about atrial refractoriness, action potential duration or heterogeneity of conduction [2].
PA-TDI duration is very closely related to PWD, as both parameters are indices of the total atrial conduction time. However, whereas PWD reflects the time interval between the earliest and latest atrial electrical activation, PA-TDI duration reflects the time interval between earliest atrial electrical activation and the latest atrial mechanical contraction. Theoretically, PA-TDI duration, therefore, provides a more comprehensive assessment of atrial remodeling than PWD. Practically, measurement of PA-TDI duration is less time-consuming than PWD derived from signal-averaged ECG [6], and has a superior prognostic value over PWD derived from a 12-lead ECG [18,19,20,21].
Heart rate can have an important impact on cardiac physiology, for example on the QT-time. The impact of heart rate on PA-TDI duration has not been investigated extensively. Chao et al. found a weak correlation of − 0.270 between PA-TDI duration and heart rate, meaning that roughly 7% of variation in PA-TDI duration can be related to the heart rate [29]. However, recently, the impact of heart rate on PWD has been studied thoroughly: Toman et al. demonstrated that within a normal range of 60–75 bpm, the impact of heart rate on PWD was neglectable [45]. Nevertheless, future studies should be directed to investigate the association between of heart rate and PA-TDI duration.
Future directions
Assessment of PA-TDI duration as a routine echo-lab parameter may substantially improve risk stratification and management of AF. The simple, quick and inexpensive measurement of PA-TDI duration enables its integration into everyday clinical practice. As PA-TDI duration reflects different aspects and dynamics of atrial cardiomyopathy, this parameter may be useful: (1) to identify patients at risk for AF; (2) to guide and monitor individualized rhythm-control therapy; and (3) to identify which patients with low CHA2DS2-VASc score may benefit from anticoagulation therapy. Carefully designed clinical trials are needed to evaluate these potential applications of PA-TDI duration.
Conclusions
The PA-TDI duration is an easy and fast-to-measure echocardiographic parameter that combines information about parts of the structural, electrical and functional changes to the atria to reflect the different and dynamic facets of atrial remodeling. Assessment of PA-TDI duration, as part of an integrated diagnostic work-up, has a potential role to improve risk stratification and management of AF in clinical practice.
References
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ (2014) Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129:837–847
Heijman J, Voigt N, Nattel S, Dobrev D (2014) Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circ Res 114:1483–1499
Goette A, Kalman JM, Aguinaga L, Akar J, Cabrera JA, Chen SA, Chugh SS, Corradi D, D’Avila A, Dobrev D, Fenelon G, Gonzalez M, Hatem SN, Helm R, Hindricks G, Ho SY, Hoit B, Jalife J, Kim YH, Lip GY, Ma CS, Marcus GM, Murray K, Nogami A, Sanders P, Uribe W, Van Wagoner DR, Nattel S (2016) EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Europace 18:1455–1490
Nattel S, Burstein B, Dobrev D (2008) Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ Arrhythm Electrophysiol 1:62–73
Burstein B, Nattel S (2008) Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J Am Coll Cardiol 51:802–809
Merckx KL, De Vos CB, Palmans A, Habets J, Cheriex EC, Crijns HJ, Tieleman RG (2005) Atrial activation time determined by transthoracic Doppler tissue imaging can be used as an estimate of the total duration of atrial electrical activation. J Am Soc Echocardiogr 18:940–944
den Uijl DW, Gawrysiak M, Tops LF, Trines SA, Zeppenfeld K, Schalij MJ, Bax JJ, Delgado V (2011) Prognostic value of total atrial conduction time estimated with tissue Doppler imaging to predict the recurrence of atrial fibrillation after radiofrequency catheter ablation. Europace 13:1533–1540
Müller P, Hars C, Schiedat F, Bösche LI, Gotzmann M, Strauch J, Dietrich JW, Vogt M, Tannapfel A, Deneke T, Mügge A, Ewers A (2013) Correlation between total atrial conduction time estimated via tissue Doppler imaging (PA-TDI Interval), structural atrial remodeling and new-onset of atrial fibrillation after cardiac surgery. J Cardiovasc Electrophysiol 24:626–631
Müller P, Schiedat F, Bialek A, Bösche L, Ewers A, Kara K, Dietrich JW, Mügge A, Deneke T (2014) Total atrial conduction time assessed by tissue doppler imaging (PA-TDI Interval) to predict early recurrence of persistent atrial fibrillation after successful electrical cardioversion. J Cardiovasc Electrophysiol 25:161–167
Müller P, Schiedat F, Dietrich JW, Shin DI, Kara K, Mügge A, Deneke T (2014) Reverse atrial remodeling in patients who maintain sinus rhythm after electrical cardioversion: evidence derived from the measurement of total atrial conduction time assessed by PA-TDI interval. J Echocardiogr 12:142–150
Antoni ML, Bertini M, Atary JZ, Delgado V, ten Brinke EA, Boersma E, Holman ER, van der Wall EE, Schalij MJ, Bax JJ, van de Veire NR (2010) Predictive value of total atrial conduction time estimated with tissue Doppler imaging for the development of new-onset atrial fibrillation after acute myocardial infarction. Am J Cardiol 106:198–203
Bertini M, Borleffs CJ, Delgado V, Ng AC, Piers SR, Shanks M, Antoni ML, Biffi M, Boriani G, Schalij MJ, Bax JJ, Van de Veire NR (2010) Prediction of atrial fibrillation in patients with an implantable cardioverter-defibrillator and heart failure. Eur J Heart Fail 12:1101–1110
van der Hulst AE, Roest AA, Holman ER, Vliegen HW, Hazekamp MG, Bax JJ, Blom NA, Delgado V (2012) Relation of prolonged tissue Doppler imaging-derived atrial conduction time to atrial arrhythmia in adult patients with congenital heart disease. Am J Cardiol 109:1792–1796
Ejima K, Kato K, Arai K, Fukushima K, Fukushima N, Suzuki T, Yoshida K, Nuki T, Uematsu S, Hoshi H, Manaka T, Ashihara K, Shoda M, Hagiwara N (2014) Impact of atrial remodeling on the outcome of radiofrequency catheter ablation of paroxysmal atrial fibrillation. Circ J 78:872–877
Fukushima K, Fukushima N, Ejima K, Kato K, Sato Y, Uematsu S, Arai K, Manaka T, Takagi A, Ashihara K, Shoda M, Hagiwara N (2015) Left atrial appendage flow velocity and time from P-wave onset to tissue Doppler-derived A’ predict atrial fibrillation recurrence after radiofrequency catheter ablation. Echocardiography 32:1101–1108
Park SM, Kim YH, Choi JI, Pak HN, Kim YH, Shim WJ (2010) Left atrial electromechanical conduction time can predict six-month maintenance of sinus rhythm after electrical cardioversion in persistent atrial fibrillation by Doppler tissue echocardiography. J Am Soc Echocardiogr 23:309–314
Maffè S, Paffoni P, Dellavesa P, Cucchi L, Zenone F, Bergamasco L, Paino AM, Franchetti Pardo N, Signorotti F, Baduena L, Parravicini U (2015) Prognostic value of total atrial conduction time measured with tissue Doppler imaging to predict the maintenance of sinus rhythm after external electrical cardioversion of persistent atrial fibrillation. Echocardiography 32:420–427
Takahashi S, Katayama K, Watanabe M, Kodama H, Taguchi T, Kurosaki T, Imai K, Sueda T (2016) Preoperative tissue Doppler imaging-derived atrial conduction time predicts postoperative atrial fibrillation in patients undergoing mitral valve surgery for mitral valve regurgitation. Circ J 80:101–109
Takahashi S, Fujiwara M, Watadani K, Taguchi T, Katayama K, Takasaki T, Kurosaki T, Imai K, Sueda T (2014) Preoperative tissue Doppler imaging-derived atrial conduction time can predict postoperative atrial fibrillation in patients undergoing aortic valve replacement for aortic valve stenosis. Circ J 78:2173–2181
De Vos CB, Weijs B, Crijns HJ, Cheriex EC, Palmans A, Habets J, Prins MH, Pisters R, Nieuwlaat R, Tieleman RG (2009) Atrial tissue Doppler imaging for prediction of new-onset atrial fibrillation. Heart 95:835–840
Müller P, Ivanov V, Kara K, Klein-Wiele O, Forkmann M, Piorkowski C, Blockhaus C, Dimitroulis D, Afzal S, Shin DI, Kelm M, Makimoto H, Mügge A (2017) Total atrial conduction time to predict occult atrial fibrillation after cryptogenic stroke. Clin Res Cardiol 106:113–119
Özlü MF, Erdem K, Kırış G, Parlar A, Demirhan A, Ayhan SS, Erdem A, Öztürk S, Tekelioğlu ÜY, Yazıcı M (2013) Predictive value of total atrial conduction time measured with tissue Doppler imaging for postoperative atrial fibrillation after coronary artery bypass surgery. J Interv Card Electrophysiol 37:27–33
Fujiwara M, Nakano Y, Hidaka T, Oda N, Uchimura Y, Sairaku A, Kajihara K, Tokuyama T, Motoda C, Watanabe Y, Ikenaga H, Imai K, Sueda T, Kihara Y (2014) Prediction of atrial fibrillation after off-pump coronary artery bypass grafting using preoperative total atrial conduction time determined on tissue Doppler imaging. Circ J 78:345–352
Hensen LCR, Delgado V, van Wijngaarden SE, Leung M, de Bie MK, Buiten MS, Schalij MJ, Van de Kerkhof JJ, Rabelink TJ, Rotmans JI, Jukema JW, Bax JJ (2017) Echocardiographic associates of atrial fibrillation in end-stage renal disease. Nephrol Dial Transplant 32:1409–1414
Tjahjadi C, Hiemstra YL, van der Bijl P, Pio SM, Bootsma M, Marsan NA, Delgado V, Bax JJ (2020) Assessment of left atrial electro-mechanical delay to predict atrial fibrillation in hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging 22:589–596
Abou R, Leung M, Tonsbeek AM, Podlesnikar T, Maan AC, Schalij MJ, Marsan NA, Delgado V, Bax JJ (2017) Effect of aging on left atrial compliance and electromechanical properties in subjects without structural heart disease. Am J Cardiol 120:140–147
Weijs B, de Vos CB, Tieleman RG, Pisters R, Cheriex EC, Prins MH, Crijns HJ (2011) Clinical and echocardiographic correlates of intra-atrial conduction delay. Europace 13:1681–1687
Leung M, Abou R, van Rosendael PJ, van der Bijl P, van Wijngaarden SE, Regeer MV, Podlesnikar T, Marsan NA, Leung DY, Delgado V, Bax JJ (2018) Relation of echocardiographic markers of left atrial fibrosis to atrial fibrillation burden. Am J Cardiol 122:584–591
Chao TF, Wang KL, Chuang CF, Chen SA, Yu WC (2012) Atrium electromechanical interval in left ventricular diastolic dysfunction. Eur J Clin Invest 42:117–122
Müller P, Grabowski C, Schiedat F, Shin DI, Dietrich JW, Mügge A, Deneke T, Walther JW, Kara K (2016) Reverse remodelling of the atria after treatment of obstructive sleep apnoea with continuous positive airway pressure: evidence from electro-mechanical and endocrine markers. Heart Lung Circ 25:53–60
Linz D, McEvoy RD, Cowie MR, Somers VK, Nattel S, Lévy P, Kalman JM, Sanders P (2018) Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol 3:532–540
Weijs B, de Vos CB, Limantoro I, Cheriex EC, Tieleman RG, Crijns HJ (2012) The presence of an atrial electromechanical delay in idiopathic atrial fibrillation as determined by tissue Doppler imaging. Int J Cardiol 156:121–122
Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D (1998) Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 98:946–952
Stewart S, Hart CL, Hole DJ, McMurray JJ (2002) A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley Study. Am J Med 113:359–364
Wolf PA, Abbott RD, Kannel WB (1991) Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 22:983–988
Dobrev D, Aguilar M, Heijman J, Guichard JB, Nattel S (2019) Postoperative atrial fibrillation: mechanisms, manifestations and management. Nat Rev Cardiol 16:417–436
Kuck KH, Brugada J, Fürnkranz A, Metzner A, Ouyang F, Chun KR, Elvan A, Arentz T, Bestehorn K, Pocock SJ, Albenque JP, Tondo C (2016) Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med 374:2235–2245
Berruezo A, Tamborero D, Mont L, Benito B, Tolosana JM, Sitges M, Vidal B, Arriagada G, Méndez F, Matiello M, Molina I, Brugada J (2007) Pre-procedural predictors of atrial fibrillation recurrence after circumferential pulmonary vein ablation. Eur Heart J 28:836–841
Leung M, van Rosendael PJ, Abou R, Marsan NA, Leung DY, Delgado V, Bax JJ (2018) Left atrial function to identify patients with atrial fibrillation at high risk of stroke: new insights from a large registry. Eur Heart J 39:1416–1425
den Uijl DW, Cabanelas N, Benito EM, Figueras R, Alarcón F, Borràs R, Prat S, Guasch E, Perea R, Sitges M, Brugada J, Berruezo A, Mont L (2018) Impact of left atrial volume, sphericity, and fibrosis on the outcome of catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol 29:740–746
den Uijl DW, Bax JJ (2009) Left atrial size as a predictor of successful radiofrequency catheter ablation for atrial fibrillation. Europace 11:1255–1256
Koca H, Demirtas AO, Kaypaklı O, Icen YK, Sahin DY, Koca F, Koseoglu Z, Baykan AO, Guler EC, Demirtas D, Koc M (2020) Decreased left atrial global longitudinal strain predicts the risk of atrial fibrillation recurrence after cryoablation in paroxysmal atrial fibrillation. J Interv Card Electrophysiol 58:51–59
Voigt JU, Mălăescu GG, Haugaa K, Badano L (2020) How to do LA strain. Eur Heart J Cardiovasc Imaging 21:715–717
Walker A, Olsson E, Wranne B, Ringqvist I, Ask P (2002) Time delays in ultrasound systems can result in fallacious measurements. Ultrasound Med Biol 28:259–263
Toman O, Hnatkova K, Smetana P, Huster KM, Šišáková M, Barthel P, Novotný T, Schmidt G, Malik M (2020) Physiologic heart rate dependency of the PQ interval and its sex differences. Sci Rep 10:2551
Acknowledgements
We thank Nadine Bemelmans for the excellent central figure for our review.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no financial disclosure and no conflict of interest to this article.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000(5). Informed consent was obtained from all patients for being included in this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Müller, P., Weijs, B., Bemelmans, N.M.A.A. et al. Echocardiography-derived total atrial conduction time (PA-TDI duration): risk stratification and guidance in atrial fibrillation management. Clin Res Cardiol 110, 1734–1742 (2021). https://doi.org/10.1007/s00392-021-01917-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01917-9