Abstract
Background
Ethnic disparities have been reported in cardiovascular disease. However, ethnic disparities in takotsubo syndrome (TTS) remain elusive. This study assessed differences in clinical characteristics between Japanese and European TTS patients and determined the impact of ethnicity on in-hospital outcomes.
Methods
TTS patients in Japan were enrolled from 10 hospitals and TTS patients in Europe were enrolled from 32 hospitals participating in the International Takotsubo Registry. Clinical characteristics and in-hospital outcomes were compared between Japanese and European patients.
Results
A total of 503 Japanese and 1670 European patients were included. Japanese patients were older (72.6 ± 11.4 years vs. 68.0 ± 12.0 years; p < 0.001) and more likely to be male (18.5 vs. 8.4%; p < 0.001) than European TTS patients. Physical triggering factors were more common (45.5 vs. 32.0%; p < 0.001), and emotional triggers less common (17.5 vs. 31.5%; p < 0.001), in Japanese patients than in European patients. Japanese patients were more likely to experience cardiogenic shock during the acute phase (15.5 vs. 9.0%; p < 0.001) and had a higher in-hospital mortality (8.2 vs. 3.2%; p < 0.001). However, ethnicity itself did not appear to have an impact on in-hospital mortality. Machine learning approach revealed that the presence of physical stressors was the most important prognostic factor in both Japanese and European TTS patients.
Conclusion
Differences in clinical characteristics and in-hospital outcomes between Japanese and European TTS patients exist. Ethnicity does not impact the outcome in TTS patients. The worse in-hospital outcome in Japanese patients, is mainly driven by the higher prevalence of physical triggers.
Trial Registration
URL: https://www.clinicaltrials.gov; Unique Identifier: NCT01947621.
Similar content being viewed by others
Introduction
Takotsubo syndrome (TTS) is characterized by acute left ventricular (LV) systolic dysfunction, which is often triggered by emotional or physical stressors [1]. The condition was first reported from Japan in 1990 and the terminology derived from a Japanese octopus trap known as takotsubo because the LV in TTS mimics the shape of it [2, 3]. TTS was largely unknown outside Japan until the first reports from Europe and the US were published in the late 90 s [4, 5]. Since then, TTS has been reported from all continents, in both sexes and in different ethnic groups [6,7,8,9,10,11]. Although TTS was initially considered to be harmless, it is now known that it has a wide range of presentations and outcomes, depending on the triggering factor [12]. It may even be associated with life-threatening complications, with outcomes comparable to those of acute coronary syndromes [12,13,14].
Ethnic and geographic disparities are known to exist in many cardiovascular diseases [15, 16]. These differences may be related to socioeconomic factors, healthcare systems, or genetic background, but there is no clear evidence in support of such speculation. To date, no large head-to-head comparison between different ethnic and geographic groups has been conducted in the field of TTS research. Little is known about ethnic differences in outcomes in TTS, especially between Asian and European patients [17].
The present study aimed to investigate differences in clinical characteristics and in-hospital outcomes between Japanese and European TTS patients and to evaluate the impact of ethnic background on outcomes.
Methods
Patients and inclusion criteria
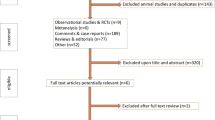
The Japanese TTS patients were enrolled from 10 different hospitals, while the European TTS patients were enrolled from the University Hospital Zurich and 31 other collaborating hospitals in 9 countries (Austria, Czech Republic, Finland, France, Germany, Italy, Poland, Switzerland, and the UK) (Fig. 1). Data were collected from January 1, 2011, through October 31, 2017, and patients with unknown ethnicity were excluded from the present analysis. All patients were diagnosed according to the InterTAK Diagnostic Criteria [18]:.
-
1)
Transient LV wall motion abnormality presenting as apical ballooning or midventricular, basal, or focal wall motion abnormalities. The wall motion abnormality usually extends beyond a single epicardial coronary artery distribution; however, in rare cases, especially in focal TTS, wall motion abnormality may be limited to a single coronary artery distribution. TTS patients who died during the acute phase, before complete recovery of LV wall motion, were also eligible for inclusion.
-
2)
TTS event is typically triggered by emotional or physical, or combined stress. However, this is not obligatory. Neurologic disorders or pheochromocytoma may also serve as triggers.
-
3)
Appearance of new electrocardiographic (ECG) abnormalities. Occasionally, there may not be any electrocardiographic changes.
-
4)
Occurrence of moderate elevations of cardiac biomarkers (troponin and/or creatine kinase). Elevation of brain natriuretic peptide is common.
-
5)
Coexisting significant coronary artery disease, which is not related to the wall motion abnormality, does not rule out TTS.
-
6)
No evidence of infectious myocarditis.
The study protocol was approved by the respective local ethics committees or institutional review boards at each collaboration site. Due to the, in part, retrospective nature of the study, the ethics committees of most study centers waived the need for informed consent. At centers where the ethics committees or institutional review boards required informed consent, formal written consent was obtained from all included patients or their surrogates.
Clinical characteristics and in-hospital outcomes
We compared demographic data, clinical characteristics, triggering factors, taktosubo type, laboratory values, ECG findings, vital signs, hemodynamic findings, cardiovascular risk factors, and medications prescribed (before admission and at discharge) between the Japanese and European TTS cohorts. Acute cardiac care treatment (use of catecholamine and intra-aortic balloon pump [IABP]) and in-hospital complications (cardiogenic shock and death) were also compared between the two groups.
Statistical analysis
Continuous data were summarized as means ± standard deviations or medians and interquartile ranges. Categorical variables were summarized as numbers and percentages. Comparisons of characteristics between different groups were performed using the unpaired t test or the Mann–Whitney U test for continuous variables and the Pearson chi-squared test for categorical variables. Variables that were statistically significant on univariate analysis were included in multivariate models, using in-hospital mortality as an endpoint. Two different models (Model I: without ethnicity as a covariate and Model II with ethnicity as a covariate) were used. The Hosmer–Lemeshow test for goodness of fit was performed for both logistic regression models. To compare these two models, and to clear any doubts about which model is more appropriate, three different statistical approaches were used. First, the Brier score was used to quantify the accuracy of risk predictions of our two logistic regression models by comparing predicted risks with observed outcomes at the individual level. The lower the Brier score is for a set of predictions, the better the predictions are calibrated. Second, classification performance was evaluated by use of receiver operating characteristic (ROC) curves. Third, the predictiveness curve was calculated [19]. The predictiveness curve is a plot of the cumulative percentage of individuals to the predicted risks. The cumulative percentage indicates the percentage of individuals with predicted risk equal to, or lower than, the risk value. The predictiveness curve also displays essential information about risk that is not displayed by the ROC curve [19]. The Delong [20] as well as the Venkatraman test [21] were used to compare the AUCs for equivalence (equivalence bound 5%) and then for equality ((AUCII—AUCI) = 0) (condition = in-hospital death). To evaluate the influence of each factor on in-hospital death, we used a radial basis function network (RBF-net) [22]. RBF networks are artificial neural networks that use radial basis functions as activation functions. They are primarily used for regression or function approximation. The Bayesian Information Criterion (BIC) determines the number of units in the hidden layer. The "best" number of hidden units is the one that yields the smallest BIC in the training data. We used normalized Gaussian radial basis functions as activation functions for the hidden layer. For the output layer, we used the identity function as the activation function; thus, the output units are simply weighted sums of the hidden units. The output of the network (in-hospital death) is, therefore, a linear combination of normalized Gaussian radial basis functions of the inputs and neuron parameters. Decision trees such as Classification And Regression Trees (CART) or exhaustive CHi-squared Automatic Interaction Detector (CHAID), were used in addition as a nonparametric supervised learning method for classification and regression. Decision trees are adaptive in at least three aspects: they (1) adapt to favorable conditions near the Bayes decision boundary; (2) focus on data distributed on lower dimensional manifolds, and (3) reject irrelevant features.
All tests were two sided and statistical significance was defined as p < 0.05. Statistical analyses were performed using IBM SPSS Statistics, version 25.0 (IBM Corp., Armonk, NY, USA) and R, version 3.5 (https://cran.r-project.org/).
Results
A total of 503 Japanese TTS patients and 1670 European TTS patients were included in this study. Table 1 presents a comparison of clinical characteristics between Japanese and European patients. The proportion of male patients was significantly higher in the Japanese cohort (18.5 vs. 8.4%; p < 0.001). Japanese patients were older (72.6 ± 11.4 vs. 68.0 ± 12.0 years; p < 0.001) and had lower body mass index (21.0 ± 3.6 vs. 24.8 ± 4.6 kg/m2; p < 0.001) than European patients. Japanese patients had lower prevalence of hypertension (52.7 vs. 66.3%; p < 0.001), current smoking (15.2 vs. 18.7%; p < 0.001), and higher prevalence of diabetes mellitus (18.1 vs. 13.5%, p = 0.011) than European patients. Troponin (median factor increase of the upper limit of normal, 16.78 vs. 7.67; p < 0.001) and brain natriuretic peptide plasma levels (median factor increase of the upper limit of normal, 13.14 vs. 5.72; p < 0.001) at hospital admission were significantly higher in Japanese patients. ST-segment elevation on admission was more common in Japanese patients than in European patients (70.3 vs. 45.0%; p < 0.001). Left ventricular ejection fraction (LVEF) on admission was significantly higher in Japanese than in European patients (44.5 ± 13.3 vs. 41.8% ± 11.2%; p < 0.001). Japanese patients were more likely to have physical triggers (45.5 vs. 32.0%; p < 0.001), and less likely to have emotional triggers (17.5 vs. 31.5%; p < 0.001) than European patients. Details on triggering factors are shown in Supplementary Fig. 1. Before admission, Japanese patients were more likely to be using calcium-channel antagonists (25.5 vs. 7.2%; p < 0.001), while European patients were more likely to be using angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers (39.4 vs. 30.8%; p = 0.001) and beta-blockers (30.9 vs. 7.9%; p < 0.001). The same trend in medications prescribed was seen at discharge (Table 1).
While in-hospital Japanese patients were more likely to experience cardiogenic shock (15.5 vs. 9.0%; p < 0.001) and more likely to receive treatment with catecholamines (14.1 vs. 10.3%; p = 0.016) or IABP (5.6 vs. 2.1%; p < 0.001) to maintain hemodynamic stability. In-hospital mortality was significantly higher in Japanese patients than in European patients (8.2 vs. 3.2%; p < 0.001).
To evaluate the influence of ethnicity on in-hospital death, we first used the two different multiple logistic regression models (Table 2). The Hosmer–Lemeshow test for goodness of fit demonstrated no evidence of poor fit for Models I and II (p = 0.26 and = 0.39, respectively). The Brier score was 0.038 for Model I and 0.037 for Model II, demonstrating that these two models were nearly identical with respect to risk predictions. On ROC analysis, the area under the curve (AUC) (95% confidence interval) was 0.81 (0.78–0.86) for Model I and 0.83 (0.78–0.88) for Model II. The comparisons of ROC curves to test for statistically significant differences between the areas under the ROC curves AUCII and AUCI using Venkatraman and DeLong tests, demonstrate again that these two models had an identical classification performance ((AUCII—AUCI) = 0 for condition = in-hospital death; Venkatraman p = 0.15; Delong p = 0.052). The predictiveness curves of both models were also almost identical (Fig. 2). Both predictiveness curves calculated the risk of in-hospital death as ≤ 10% for around 90% of the study population.
Radial Basis Function Networks and CART were applied to analyze the effect of various variables on in-hospital death in the Japanese and European cohorts. The normalized importance of the respective variables for the Japanese and European cohorts is summarized in Supplementary Figs. 2 and 3. Physical stress was the most important prognostic factor for in-hospital mortality in both cohorts. The second most important prognostic factor was LVEF by both CART and RBF-nets for Japanese patients, while it was white blood cell count by CART or heart rate by RBF-nets for European patients. The in-hospital mortality rate in TTS patients without physical stress (n = 1410; 64.9%) was 1.7%, with no significant difference between the Japanese (n = 274) and European (n = 1136) cohorts (2.6 vs. 1.5%, p = 0.22) (Fig. 3).
Decision trees. Decision trees for Japanese patients (a) and European patients (b). Presence of physical stressors was the most important prognostic factor for in-hospital mortality in the Japanese and European cohorts. The second most important prognostic factor was LVEF for Japanese patients, and the white blood cell count for European patients. LVEF left ventricular ejection fraction, SBP systolic blood pressure, WBC white blood cell count
Discussion
This study aimed to investigate differences in clinical and demographic characteristics and in-hospital outcomes between Japanese and European TTS patients and to determine whether ethnicity affects outcomes. The main findings were as follows: (2) Japanese patients were more likely to have physical triggers, and less likely to have emotional triggers; (3) Japanese patients required more often catecholamines and/or IABP to maintain hemodynamic stability; and (4) Japanese patients had higher in-hospital mortality, although ethnicity per se did not appear to have an impact on the higher mortality.
No large-scale study has been conducted so far to compare TTS features between different ethnic groups. In a small study, Maekawa et al. found no significant difference in clinical characteristics between TTS patients in Japan (n = 12) and USA (n = 34) [17]. However, recent reports from Europe and Japan have demonstrated some differences in the demographic characteristics of those affected in these two regions: in Europe 85–90% of patients are women, and the mean age of patients is 65–70 years [13, 23, 24], whereas in Japan, 75–85% are women, and the mean age of patients is 70–75 years [25,26,27]. These findings were confirmed in the present study, the largest head-to-head comparison to date. However, it should be noted that these disparities may reflect potential differences in patient selection and the older age of the general population in Japan [28].
The present study found significant differences between the two cohorts in medications being used by the patients at admission. This difference may have partly affected in-hospital outcomes. Japanese patients were more likely to be on regular calcium-channel antagonists at the TTS index event. These drugs are obviously contraindicated in patients with acute heart failure because of their negative inotropic effect [29] and their activation of the sympathetic nervous system [30]. In contrast, European TTS patients were more likely to receive beta-blockers, however, which have failed to show a beneficial effect on 1-year mortality [13]. Regular treatment with beta-blockers before admission may have protected patients with apical ballooning from left ventricular outflow tract obstruction [25]. These disparities in drug prescription seem to be due to different guidelines for the treatment of hypertension in these two regions [29, 31].
From a clinical perspective, the most important finding of the present study was the unanticipated worse in-hospital outcome in Japanese patients. We demonstrated by machine learning approach that the prognostic factors for in-hospital mortality were almost same in both cohorts; however, the relative importance of the factors varied. Physical stress was the most important prognostic factor for in-hospital mortality in both cohorts. However, the prevalence of physical stressors was higher in Japanese patients and might have been responsible for the higher in-hospital mortality in this cohort. This observation is in line with our previous study demonstrating that physical triggers of TTS are independent predictors of poor in-hospital outcomes [12, 13]. Japanese patients were more likely to have cardiogenic shock than European patients. It is notable that in patients with cardiogenic shock IABP was more often used in Japan compared to Europe (35.9 vs. 23.5%).
Although a role for genetics in TTS has not yet been fully uncovered, we examined whether ethnicity independently influences outcomes. Brinjikji et al., in their nation-wide study in the US, found that ethnicity was not associated with in-hospital mortality in TTS [32]; their study, however, had a very small proportion of Asian patients and included only patients located in the US without taking also geographic differences into account. Notably, we revealed in the present study by use of three different statistical approaches that two different multiple logistic regression models (with and without ethnicity) had almost same accuracies of a risk prediction for in-hospital death. This observation can be interpreted that ethnicity, per se, does not have an additional impact on in-hospital death beyond that caused by differences of other clinical backgrounds. Nevertheless, patients with different ethnicities were enrolled from different regions, and so differences between groups could be due to geographic and socioeconomic factors and regional differences in therapeutic strategies. Therefore, further studies are needed to clarify the impact of genetic factors on in-hospital outcomes of TTS patients.
Conclusions
This large-scale head-to-head comparative study provides important insights into ethnic disparities between Japanese and European TTS patients. Japanese patients are older and more likely to be male than European patients; they also have a significantly higher prevalence of physical triggers. Cardiogenic shock and in-hospital death are more common in Japanese patients. Ethnicity, per se, does not appear to have an additional impact on in-hospital mortality, beyond that caused by differences of other clinical backgrounds. Presence of physical stress is the most important prognostic factor in both Japanese and European patients. Thus, the worse in-hospital outcome in Japanese patients is mainly driven by the higher prevalence of physical triggers in this cohort.
References
Kato K, Lyon AR, Ghadri JR, Templin C (2017) Takotsubo syndrome: aetiology, presentation and treatment. Heart 103:1461–1469
Sato H (1990) Tako-tsubo-like left ventricular dysfunction due to multivessel coronary spasm. In: Kodama K, Haze K, Hori M (eds) Clinical aspect of myocardial injury: from ischemia to heart failure. Kagakuhyoronsha Publishing Co., Tokyo, pp 56–64 (Article in Japanese)
Dote K, Sato H, Tateishi H, Uchida T (1991) Ishihara M [myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases]. J Cardiol 21:203–214
Pavin D, Le Breton H, Daubert C (1997) Human stress cardiomyopathy mimicking acute myocardial syndrome. Heart 78:509–511
Sharkey SW, Shear W, Hodges M, Herzog CA (1998) Reversible myocardial contraction abnormalities in patients with an acute noncardiac illness. Chest 114:98–105
Kato K, Sakai Y, Ishibashi I, Kobayashi Y (2014) Recurrent mid-ventricular takotsubo cardiomyopathy. Int J Cardiovasc Imaging 30:1417–1418
Schlossbauer SA, Ghadri JR, Cammann VL, Maier W, Luscher TF, Templin C (2016) A broken heart in a broken car. Cardiol J 23:352–354
Singh K, Marinelli T, Horowitz JD (2013) Takotsubo cardiomyopathy after anti-influenza vaccination: catecholaminergic effects of immune system. Am J Emerg Med 31(1627):e1621-1624
do Nascimento CU, Bosso CE, Jorge PH, Vanderlei FM, Ebaid HI, Valenti VE, Vanderlei LC (2013) Apical ballooning syndrome (takotsubo syndrome): case report. Int Arch Med 6:12
Srivastava NT, Parent JJ, Hurwitz RA (2016) Recurrent takotsubo cardiomyopathy in a child. Cardiol Young 26:410–412
Rush C, Ntsekhe M (2015) A lady with a broken heart: apical ballooning syndrome. S Afr Med J 105:422
Ghadri JR, Kato K, Cammann VL, Gili S, Jurisic S, Di Vece D, Candreva A, Ding KJ, Micek J, Szawan KA, Bacchi B, Bianchi R, Levinson RA, Wischnewsky M, Seifert B, Schlossbauer SA, Citro R, Bossone E, Munzel T, Knorr M, Heiner S, D’Ascenzo F, Franke J, Sarcon A, Napp LC, Jaguszewski M, Noutsias M, Katus HA, Burgdorf C, Schunkert H, Thiele H, Bauersachs J, Tschope C, Pieske BM, Rajan L, Michels G, Pfister R, Cuneo A, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun-Dullaeus RC, Banning A, Cuculi F, Kobza R, Fischer TA, Vasankari T, Airaksinen KEJ, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Empen K, Felix SB, Delmas C, Lairez O, El-Battrawy I, Akin I, Borggrefe M, Horowitz J, Kozel M, Tousek P, Widimsky P, Gilyarova E, Shilova A, Gilyarov M, Winchester DE, Ukena C, Bax JJ, Prasad A, Bohm M, Luscher TF, Ruschitzka F, Templin C (2018) Long-term prognosis of patients with takotsubo syndrome. J Am Coll Cardiol 72:874–882
Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschope C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfister R, Ukena C, Bohm M, Erbel R, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun-Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T, Airaksinen KE, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Luscher TF (2015) Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 373:929–938
Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, Crea F, Galiuto L, Desmet W, Yoshida T, Manfredini R, Eitel I, Kosuge M, Nef HM, Deshmukh A, Lerman A, Bossone E, Citro R, Ueyama T, Corrado D, Kurisu S, Ruschitzka F, Winchester D, Lyon AR, Omerovic E, Bax JJ, Meimoun P, Tarantini G, Rihal C, Shams YH, Migliore F, Horowitz JD, Shimokawa H, Luscher TF, Templin C (2018) International expert consensus document on takotsubo syndrome (part ii): diagnostic workup, outcome, and management. Eur Heart J. 39:2047–2062
Graham G (2015) Disparities in cardiovascular disease risk in the united states. Curr Cardiol Rev 11:238–245
Balfour PC Jr, Rodriguez CJ, Ferdinand KC (2015) The role of hypertension in race-ethnic disparities in cardiovascular disease. Curr Cardiovasc Risk Rep 9:18
Maekawa Y, Kawamura A, Yuasa S, Nesto RW, Fukuda K (2012) Direct comparison of takotsubo cardiomyopathy between Japan and USA: 3-year follow-up study. Intern Med 51:257–262
Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, Cammann VL, Crea F, Galiuto L, Desmet W, Yoshida T, Manfredini R, Eitel I, Kosuge M, Nef HM, Deshmukh A, Lerman A, Bossone E, Citro R, Ueyama T, Corrado D, Kurisu S, Ruschitzka F, Winchester D, Lyon AR, Omerovic E, Bax JJ, Meimoun P, Tarantini G, Rihal C, Shams YH, Migliore F, Horowitz JD, Shimokawa H, Luscher TF, Templin C (2018) International expert consensus document on takotsubo syndrome (part i): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J. 39:2032–2046
Pepe MS, Feng Z, Huang Y, Longton G, Prentice R, Thompson IM, Zheng Y (2008) Integrating the predictiveness of a marker with its performance as a classifier. Am J Epidemiol 167:362–368
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Venkatraman ES, Begg CB (1996) A distribution-free procedure for comparing receiver operating characteristic curves from a paired experiment. Biometrika 83:835–848
Wu Y, Wang H, Zhang B, Du KL (2012) Using radial basis function networks for function approximation and classification. ISRN Appl Math 2012:324194
Tornvall P, Collste O, Ehrenborg E, Jarnbert-Petterson H (2016) A case-control study of risk markers and mortality in takotsubo stress cardiomyopathy. J Am Coll Cardiol 67:1931–1936
Redfors B, Vedad R, Angeras O, Ramunddal T, Petursson P, Haraldsson I, Ali A, Dworeck C, Odenstedt J, Ioaness D, Libungan B, Shao Y, Albertsson P, Stone GW, Omerovic E (2015) Mortality in takotsubo syndrome is similar to mortality in myocardial infarction—a report from the swedeheart registry. Int J Cardiol 185:282–289
Isogai T, Matsui H, Tanaka H, Fushimi K, Yasunaga H (2016) Early beta-blocker use and in-hospital mortality in patients with takotsubo cardiomyopathy. Heart 102:1029–1035
Murakami T, Yoshikawa T, Maekawa Y, Ueda T, Isogai T, Konishi Y, Sakata K, Nagao K, Yamamoto T, Takayama M, Committee CCUNS (2014) Characterization of predictors of in-hospital cardiac complications of Takotsubo cardiomyopathy: multi-center registry from Tokyo CCU network. J Cardiol. 63:269–273
Kato K, Kitahara H, Saito Y, Fujimoto Y, Sakai Y, Ishibashi I, Himi T, Kobayashi Y (2017) Impact of myocardial bridging on in-hospital outcome in patients with takotsubo syndrome. J Cardiol 70:615–619
Sharkey SW, Maron BJ (2014) Epidemiology and clinical profile of takotsubo cardiomyopathy. Circ J 78:2119–2128
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, Group ESCSD (2018) 2018 esc/esh guidelines for the management of arterial hypertension. Eur Heart J 39:3021–3104
Wenzel RR, Allegranza G, Binggeli C, Shaw S, Weidmann P, Luscher TF, Noll G (1997) Differential activation of cardiac and peripheral sympathetic nervous system by nifedipine: role of pharmacokinetics. J Am Coll Cardiol 29:1607–1614
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S, Japanese Society of Hypertension Committee for Guidelines for the Management of H (2014) The Japanese society of hypertension guidelines for the management of hypertension (jsh 2014). Hypertens Res 37:253–390
Brinjikji W, El-Sayed AM, Salka S (2012) In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the national inpatient sample 2008 to 2009. Am Heart J 164:215–221
Funding
Open Access funding provided by Universität Zürich. CT has been supported by the H.H. Sheikh Khalifa bin Hamad Al-Thani Research Programme and the Swiss Heart Foundation. L.S.M. has been supported by EU HORIZON 2020 (SILICOFCM ID777204). J.R.G has received a grant “Filling the gap” from the University of Zurich. The InterTAK Registry is supported by The Biss Davies Charitable Trust.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Imori, Y., Kato, K., Cammann, V.L. et al. Ethnic comparison in takotsubo syndrome: novel insights from the International Takotsubo Registry. Clin Res Cardiol 111, 186–196 (2022). https://doi.org/10.1007/s00392-021-01857-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01857-4