Abstract
Aims
Epicardial adipose tissue (EAT) has been linked to impaired reperfusion success after percutaneous coronary intervention (PCI). Whether EAT predicts myocardial damage in the early phase after acute myocardial infarction (MI) is unclear. Therefore, we investigated whether EAT in patients with acute MI is associated with more microvascular obstruction (MVO), greater ST-deviation, larger infarct size and reduced myocardial salvage index (MSI).
Methods and results
This retrospective analysis of a prospective observational study including patients with acute MI (n = 54) undergoing PCI and 12 healthy matched controls. EAT, infarct size and MSI were analyzed with cardiac magnetic resonance imaging, conducted 3–5 days and 12 weeks after MI. Patients with acute MI showed higher EAT volume than healthy controls (46 [25.;75. percentile: 37;59] vs. 24 [15;29] ml, p < 0.001). The high EAT group (above median) showed significantly more MVO (2.22 [0.00;5.38] vs. 0.0 [0.00;2.18] %, p = 0.004), greater ST-deviation (0.38 [0.22;0.55] vs. 0.15 [0.03;0.20] mV×10−1, p = 0.008), larger infarct size at 12 weeks (23 [17;29] vs. 10 [4;16] %, p < 0.001) and lower MSI (40 [37;54] vs. 66 [49;88] %, p < 0.001) after PCI than the low EAT group. After accounting for demographic characteristics, body-mass index, heart volume, infarct location, TIMI-flow grade as well as apnea–hypopnea index, EAT was associated with infarct size at 12 weeks (B = 0.38 [0.11;0.64], p = 0.006), but not with MSI.
Conclusions
Patients with acute MI showed higher volume of EAT than healthy individuals. High EAT was linked to more MVO and greater ST-deviation. EAT was associated with infarct size, but not with MSI.
Graphic abstract

Similar content being viewed by others
Introduction
Besides traditional cardiovascular risk factors, body fat is an important factor for determining cardiometabolic risk [1]. The distribution rather than the absolute quantity of excess body fat plays a key role in the pathophysiology of cardiovascular disease [2]. Growing evidence suggests that epicardial adipose tissue (EAT) has been linked to impaired reperfusion success after percutaneous coronary intervention (PCI) [3]. Increased EAT is associated with incident myocardial infarction (MI) [4] and with angiographic severity of an acute coronary syndrome [5]. From previous studies it is known that infarct size [6, 7] is an important predictor of major cardiovascular endpoints in patients after ST-elevation myocardial infarction (STEMI) [7,8,9]. Cardiac magnetic resonance imaging (CMR) is the gold standard for assessing infarct size [10] and EAT can be assessed as well. Furthermore, EAT-induced elevation of paracrine mediator levels may activate platelet aggregation, thereby increase microvascular obstruction (MVO) [11, 12] and thus may result in larger infarct size and myocardial salvage index (MSI). On the other hand, Bière [13] and Gohbara [14], reported a protective effect of EAT on infarct size and MSI.
Therefore, the aim of this observational study was to investigate whether EAT in patients with acute MI is associated with more MVO, greater ST-deviation, larger infarct size and reduced MSI.
Methods
Patients and participants
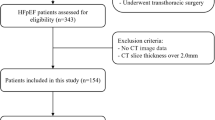
This is a retrospective analysis of a prospective observational study published previously [15]. Two hundred twenty consecutive patients aged between 18 and 80 years with a first acute MI who were treated by PCI within 24 h after symptom onset at the University Medical Center Regensburg were tested for eligibility (Fig. 1) [15]. Acute MI was defined as new ST elevation on the electrocardiogram or as native coronary artery occlusion. Key exclusion criteria were previous MI or previous myocardial revascularization, indication for surgical myocardial revascularization, cardiogenic shock, and contraindications for CMR (e.g. previous cardiac device implantation), including in the final sub-analysis 54 patients with acute MI (Fig. 1). As a control group, 12 healthy matched (age, sex, BMI) volunteers without any history of heart disease (potential living kidney donors) [16] underwent CMR (Fig. 1).
The local Ethics Committee approved the study protocol based on the regulations stated in the Helsinki Declaration of Good Clinical Practice. Prior to enrolment, written informed consent was obtained from each participant.
Percutaneous coronary intervention
Each patient received medication according to current guidelines. PCI was conducted according to standard clinical practice [15]. In addition, administration of glycoprotein IIb/IIIa inhibitors and thrombectomy were at the discretion of the interventionalist.
Assessment of outcomes
Patients with acute MI underwent CMR and polysomnography 3–5 days and 12 weeks after PCI [15, 17, 18]. In a subset of STEMI patients with analyzable [19] and available routine electrocardiograms (ECG) before PCI and > 24 h after PCI (n = 27), a non-prespecified sub-analysis of ST-deviations was performed as described previously [20].
Cardiac magnetic resonance image analysis
The CMR study protocol has been published previously [15]. Additional details of the image analysis and the acquisition protocol are described in the online supplement.
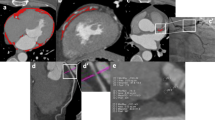
Cardiac adipose tissue was analyzed by means of the highly accurate and reproducible methods of CMR and the 3-dimensional slice summation technique [21] using short-axis slices in consecutive end-diastolic images [21]. A specific protocol was applied starting with the image on which the mitral valve annulus was first visible down to the apex [21]. Cardiac adipose tissue was divided into EAT and paracardial adipose tissue (Fig. 2). EAT was defined as adipose tissue in-between the pericardium, whereas, paracardial adipose tissue was specified as adipose tissue outside the pericardium but directly adherent to the heart. The sum of epicardial and paracardial adipose tissue was referred to as pericardial adipose tissue [22]. EAT and paracardial adipose tissue were manually segmented with the free software ITK Snap (published under General Public License) [23]. Heart volume without cardiac adipose tissue was quantified by manually tracing the area in-between the visceral layer of the pericardium. MI was assumed, if the signal intensity of hyperenhanced myocardium on delayed enhancement imaging was > 5 standard deviations above the mean signal intensity of the remote region and MVO was defined as a hypoenhanced region within the infarcted myocardium [24, 25]. Infarct size and MVO were expressed as a percentage of the total left ventricular myocardial volume [20], when not stated otherwise. The MSI represents the difference between the area at risk and the final MI size highlighting the amount of myocardium which can be saved [15].
Statistical analysis
Categorical data are presented as frequency with percentages, and comparisons between categorical variables were made with the Chi-squared test. Normally distributed quantitative data are expressed as mean ± standard deviation, non-normal as median and interquartile range (IQR). Comparisons between quantitative variables were done with either unpaired Student’s t test or Mann–Whitney U test as necessary. Consecutive measurements were analyzed with the paired t-test.
MVO was classified as present, if > 0% of left ventricular volume were affected. Associations between EAT, ST-deviation and infarct size or MSI were described using linear regression analysis. EAT was included as continuous variable. Multivariate linear regression analyses were conducted to identify predictors of infarct size at baseline and after 12 weeks as well as MSI, including known possible predictors such as infarct location, TIMI flow grade before and after percutaneous coronary intervention and sleep-disordered breathing as previously published [15, 26]. All models were corrected for baseline characteristics such as age, sex, body-mass index and heart volume. A two-sided p-value of < 0.05 was considered statistically significant. Data entry and calculations were made with the software package SPSS 25.0 (Chicago, EUA) and R (version 2.14.2).
Results
Study population
54 patients fulfilled the inclusion criteria and were enrolled in the study (Fig. 1). The baseline characteristics such as age, sex, body weight, blood pressure were similarly distributed between patients with acute MI (MI group) and the control group, except for heart rate that was lower in the latter group (Table 1).
Cardiac adipose tissue
Patients with acute MI had a significantly higher EAT volume (46 [25./75. percentile: 37; 59] vs. 24 [15; 29] ml, p < 0.001; Fig. 3) and total cardiac adipose tissue (163 [132; 201] vs. 117 [84; 159] ml, p < 0.001) than the control group. The amount of paracardial adipose tissue did not significantly differ between the MI and the control group (113 [90; 146] vs. 99 [69; 124] ml, p = 0.126). Same results were seen for EAT, total cardiac adipose tissue and paracardial adipose tissue divided by body-mass index (1.6 [1.3; 2.1] vs. 0.9 [0.6; 1.1] ml/kg/m2, p < 0.001; 5.7 [5.0; 6.7] vs. 4.5 [3.4; 5.9] ml/kg/m2, p = 0.029; 4.0 [3.3; 4.7] vs. 3.7 [2.7; 4.7] ml/kg/m2, p = 0.435, respectively).
Patients with acute myocardial infarction
The baseline characteristics of the two groups of patients stratified according to the median EAT volume at baseline are depicted in Table 2. The two groups did not differ with respect to age, height, heart rate, systolic or diastolic blood pressure and total sleep time. The high EAT group showed significantly higher body mass index, AHI, heart volume, maximum creatine-kinase and proportion of men than the low EAT group. The two groups did not differ with regard to cardiovascular risk factors, such as cholesterol, low density lipoprotein (LDL), high density lipoprotein (HDL), triglycerides, CRP levels, smoking status, or the prevalence of diabetes mellitus. Both groups were similar with respect to infarct type, infarct location, or in TIMI flow rate before and after PCI.
Microvascular obstruction and ST-deviation
12 weeks after PCI, the high EAT group showed significantly more MVO than the low EAT group (2.22 [0.00; 5.38] vs. 0.0 [0.00; 2.18] %, p = 0.004; Fig. 4a). The best predictive EAT volume for MVO was 40.8 ml (sensitivity 77.4%, specificity 60.9%). MVO > 0% was present in 31 of 54 patients (57%) and the extent of MVO was significantly associated with the extent of EAT (B = 0.324 [0.024; 0.234], p = 0.017) in univariate analysis, but not after accounting for potential confounders.
Box plots of microvascular obstruction a, mean ST-deviation > 24 h after percutaneous coronary intervention (PCI) b, infarct size after 12 weeks c and myocardial salvage index d according to the low and high epicardial adipose tissue (EAT) volume group. Data are expressed as median, minimum, maximum, 25. percentile, and 75. percentile
In a subset of STEMI patients with analyzable routine ECG (n = 27), the high and the low EAT groups had similar ST-deviations before PCI (1.13 [0.73; 1.87] vs. 1.00 [0.39; 1.19] mVx10−1, p = 0.294). However, > 24 h after PCI, patients from the high EAT group had significantly greater ST-deviations compared to the low EAT group (0.38 [0.22; 0.55] vs. 0.15 [0.03; 0.20] mVx10−1, p = 0.008; Fig. 4b). ST-deviation > 24 h after PCI was significantly associated with infarct size 12 weeks after PCI (B = 29.26 [17.86; 40.66] p < 0.001, Fig. S1).
Predictors of infarct size and myocardial salvage index
The relative infarct size in relation to the left ventricular volume at baseline and after 12 weeks was significantly higher in the high EAT group than in the low EAT group (24 [16; 34] vs. 15 [7; 22] %, p = 0.003; 23 [17; 29] vs. 10 [4; 16] %, p < 0.001; Fig. 4c, respectively). EAT and infarct size were significantly correlated at baseline and at 12 weeks (R2 linear = 0.220, p < 0.001, R2 linear = 0.302, p < 0.001; Fig. S2a, b). EAT was an independent predictor of infarct size at baseline and at 12 weeks size after accounting for potential confounders such as infarct location, TIMI flow grade before and after PCI and sleep-disordered breathing, respectively (B = 0.49 [0.0; 0.90], p = 0.017; B = 0.38 [0.11; 0.64] p = 0.006; Table 3, respectively). When including only those with high EAT and low PAT (n = 8) and those with low EAT combined with high PAT (n = 7), univariate analysis revealed no association with baseline and 12 weeks follow-up infarct size.
The MSI was significantly lower in the high EAT group compared to the low EAT group (40 [37; 54] vs. 66 [49; 88] %, p < 0.001; Fig. 4d). In univariate linear regression analysis EAT was significantly associated with MSI (B = – 0.005 [ – 0.007; – 0.002], p = 0.002), however, this association was no longer significant either after adjustment for AHI only (B = – 0.001 [ – 0.004; 0.001], p = 0.262) or in the fully adjusted model (Table 3).
Discussion
The current retrospective analysis of a prospective observational study on the association between EAT and MI size yielded several novel findings. First, patients with acute MI had significantly more EAT than healthy individuals.
Second, patients with acute MI and high EAT had more MVO than patients with low EAT. Before PCI, ST-deviation was similar between groups. However, after PCI, the high EAT group had more residual ST-deviation compared to the low EAT group. ST-deviation after PCI was associated with infarct size.
Third, patients with acute MI and high EAT had larger infarct size at baseline and 12 weeks after MI than those with low EAT. EAT was significantly associated with infarct size at baseline and 12 weeks after MI, independently of demographic characteristics, infarct location, efficacy of PCI as well as sleep-disordered breathing. The high EAT group had a significantly lower MSI.
EAT in patients with acute myocardial infarction and healthy controls
Patients with acute MI had 50% more EAT in comparison to healthy controls. Similarly, Mahabadi et al. [4] (Table S1) observed in a cohort study of 4093 participants, that patients with incident coronary events had 21% more EAT compared to patients without coronary events. In addition, hypertensive men without MI had less EAT in comparison to those with MI [27]. Conflicting data from Bière et al. [13] (Table S1) showed no differences in epicardial adipose tissue volumes between STEMI patients (primary PCI and rescue PCI within 12 h) and healthy controls with a very broad spectrum of EAT values (0–105 ml), resulting in 16% patients with MI and less than 10 ml EAT. According to previous results [4], the results from the present analysis and pathophysiology, these findings seem to be disputable. It is uncertain whether such conflicting results are a consequence of differences in the studied patient population or differences in methodology of assessment of EAT (e.g. technique of MRI or interval between MI and MRI) [13]. The effect of EAT on cardiovascular events is thought to result from the endocrine, pro-inflammatory activity of EAT [22].
EAT, MVO and ST-deviation in patients with myocardial infarction
MVO, assessed by CMR, is regarded as a better predictor for mortality than ejection fraction and different clinical scores [25, 28, 29] and the extent of MVO is associated with short-term and long-term mortality [29, 30]. MVO occurred in 57.4% in the MI cohort reflecting the largest pooled data analysis with 1688 patients on MVO and STEMI with 56.9% [29]. Alam et al. [31] reported an association of EAT and impaired myocardial flow reserve as surrogate parameter for microvascular dysfunction in patients with non-obstructive coronary artery disease. Classifying patients with acute MI in a high and low EAT volume group, we could show that within 12 weeks after PCI high EAT volume was associated with more MVO. But this association was not robust in multivariate analysis. Contrary, Gohbara et al. [14] (Table S1) reported very low amounts of MVO (1%) in patients with low (16 ml) and high (48 ml) EAT volumes. However, in the study of Gohbara et al. [14] BMI was 25 kg/m2 and 22% patients had TIMI flow > 1 reflecting a healthier population than in the current cohort. Another study [13] with similar subepicardial adipose tissue volumes in STEMI and healthy controls, reported MVO less frequent in STEMI patients with high EAT (> 34 ml) compared to low EAT (< 34 ml). The current analysis showed that ST deviation was similar before PCI and deviation was greater after PCI in the high EAT group than in the low EAT group. Findings are in line with Zencirci et al. [3] (Table S1), who showed that patients with acute MI with resolution of ST segment deviation ≥ 70% had a lower thickness of EAT compared to those with a poor resolution of ST segment deviation (< 70%).
EAT, infarct size and MSI in patients with acute myocardial infarction
Keeping in mind that infarct size, measured by CMR, is a strong predictor for all-cause mortality after MI [7], our study shows that EAT is an independent predictor of infarct size, both at baseline as well as after 12 weeks. EAT remained an independent predictor of infarct size even after adjustment for traditional risk factors. EAT was associated with greater infarct size assessed with CMR and with higher creatine kinase as a surrogate for greater infarct size. These findings are supported by the association of EAT with MVO and ST-deviation. Both parameters mirroring disturbed microcirculation [32], correlate with infarct size [30, 33].
In contrast to our analyses, others [13, 14] (Table S1) reported conflictive results in STEMI patients with less infarct size in the high EAT group. These findings were stated to be associated with obesity paradox [13, 14]. Bière et al. [13] could not reproduce the established finding that patients with MI have higher EAT volume compared to healthy controls (Table S1) [4, 27].
While EAT was significantly associated with infarct size in this analysis, independently of several other risk factors for infarct size, this was not the case for the association with MSI. Sleep-disordered breathing was one of the strongest confounders for the association between EAT and MSI, confirming previous findings identifying sleep-disordered breathing as a strong predictor for MSI with a high pathophysiologic plausibility to contribute to cardiac damage [15]. Therefore, the pathophysiological effect of sleep-disordered breathing [34] might be stronger than the endocrine effects of EAT. Similar to the results with respect to infarct size, Gohbara et al. [14] reported an opposite association of EAT and MSI than the current analysis.
However, further evidence for the potentially harmful impact of EAT derive from animal studies, showing that resection of EAT decreases progression of cardiovascular disease in coronary arteries [35, 36]. Therefore, future studies in humans with acute MI are necessary to confirm and clarify the potentially protective effect of decreasing EAT volume on cardiovascular disease.
Pathophysiological considerations
Evidence indicates that the effect of EAT on cardiovascular disease may mainly result from its release of endocrine proinflammatory mediators such as interleukin-6 (IL-6) and TNF-α [37]. EAT produced pro-inflammatory markers could lead to platelet aggregation and increased leucocyte activation followed by intravascular plugging resulting in MVO [38, 39] and impaired coronary flow reserve [40].
A further explanation could be the more pronounced arteriosclerosis and the higher rates of coronary events due to the inherent pro-inflammatory activity of EAT [4, 41, 42]. On the one side high EAT volume has been shown to be associated with the vulnerability of coronary artery plaques [43] and on the other side severe coronary artery disease may stimulate the expression of pro-inflammatory parameters in the EAT [37].
Taken together, these pathomechanisms may result in a vicious circle of high EAT volume, inflammation and arteriosclerosis which may lead to a more pronounced myocardial damage as seen in the current analysis.
Limitations
This study is limited by its sample size and its design that does not allow to build causal relations. Therefore, further experimental studies and randomized clinical trials are required. The control group was a small group of healthy volunteers [16]. Therefore, a potential selection bias cannot be excluded in total. However, controls and patients were matched for age, sex and BMI. Despite correcting for BMI and AHI [44], we cannot exclude whether the effect of EAT is independent of body fat distribution. Waist-to-hip ratio and visceral obesity were not assessed. Lesion geometry and location of lesion (proximal vs. distal) was not taken into account in the multivariate analysis.
Conclusion
Patients with acute MI showed higher volume of EAT than healthy individuals. High EAT was linked to more MVO and less ST-deviation. EAT was significantly associated with infarct size, independently of demographic characteristics, BMI, heart volume, infarct location, efficacy of PCI as well as sleep-disordered breathing. EAT was not independently associated with MSI. Further clinical and mechanistic studies are needed to evaluate whether EAT may contribute to myocardial damage in the early phase after myocardial infarction.
Change history
14 June 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00392-021-01889-w
References
Hubert HB, Feinleib M, McNamara PM, Castelli WP (1983) Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study. Circulation 67:968–977. https://doi.org/10.1161/01.cir.67.5.968
Janssen I, Katzmarzyk PT, Ross R (2004) Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr 79:379–384. https://doi.org/10.1093/ajcn/79.3.379
Zencirci E, Zencirci AE, Değirmencioğlu A, Karakuş G, Uğurlucan M, Özden K, Erdem A, Güllü AÜ, Ekmekçi A, Velibey Y, Erer HB, Çelik S, Akyol A (2015) The relationship between epicardial adipose tissue and ST-segment resolution in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Heart Vessels 30:147–153. https://doi.org/10.1007/s00380-013-0459-2
Mahabadi AA, Berg MH, Lehmann N, Kälsch H, Bauer M, Kara K, Dragano N, Moebus S, Jöckel K-H, Erbel R, Möhlenkamp S (2013) Association of epicardial fat with cardiovascular risk factors and incident myocardial infarction in the general population: The Heinz Nixdorf Recall Study. J Am Coll Cardiol 61:1388–1395. https://doi.org/10.1016/j.jacc.2012.11.062
Ozcan F, Turak O, Canpolat U, Kanat S, Kadife I, Avcı S, Işleyen A, Cebeci M, Tok D, Başar FN, Aras D, Topaloğlu S, Aydoğdu S (2014) Association of epicardial fat thickness with TIMI risk score in NSTEMI/USAP patients. Herz 39:755–760. https://doi.org/10.1007/s00059-013-3914-z
Selker HP, Udelson JE, Ruthazer R, D’Agostino RB, Nichols M, Ben-Yehuda O, Eitel I, Granger CB, Jenkins P, Maehara A, Patel MR, Ohman EM, Thiele H, Stone GW (2017) Relationship between therapeutic effects on infarct size in acute myocardial infarction and therapeutic effects on 1-year outcomes: A patient-level analysis of randomized clinical trials. Am Heart J 188:18–25. https://doi.org/10.1016/j.ahj.2017.02.028
Stone GW, Selker HP, Thiele H, Patel MR, Udelson JE, Ohman EM, Maehara A, Eitel I, Granger CB, Jenkins PL, Nichols M, Ben-Yehuda O (2016) Relationship between infarct size and outcomes following primary PCI. J Am Coll Cardiol 67:1674–1683. https://doi.org/10.1016/j.jacc.2016.01.069
Eitel I, Desch S, Fuernau G, Hildebrand L, Gutberlet M, Schuler G, Thiele H (2010) Prognostic significance and determinants of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. J Am Coll Cardiol 55:2470–2479. https://doi.org/10.1016/j.jacc.2010.01.049
Eitel I, Thiele H (2014) Prognostic role of CMR imaging after myocardial infarction. J Am Coll Cardiol 64:2069. https://doi.org/10.1016/j.jacc.2014.05.078
Kim HW, Farzaneh-Far A, Kim RJ (2009) Cardiovascular magnetic resonance in patients with myocardial infarction: Current and emerging applications. J Am Coll Cardiol 55:1–16. https://doi.org/10.1016/j.jacc.2009.06.059
Jaffe R, Charron T, Puley G, Dick A, Strauss BH (2008) Microvascular obstruction and the no-reflow phenomenon after percutaneous coronary intervention. Circulation 117:3152–3156. https://doi.org/10.1161/CIRCULATIONAHA.107.742312
Michaels AD, Gibson CM, Barron HV (2000) Microvascular dysfunction in acute myocardial infarction: Focus on the roles of platelet and inflammatory mediators in the no-reflow phenomenon. Am J Cardiol 85:50B-60B. https://doi.org/10.1016/s0002-9149(00)00811-0
Bière L, Behaghel V, Mateus V, Assunção A, Gräni C, Ouerghi K, Grall S, Willoteaux S, Prunier F, Kwong R, Furber A (2017) Relation of quantity of subepicardial adipose tissue to infarct size in patients with ST-elevation myocardial infarction. Am J Cardiol 119:1972–1978. https://doi.org/10.1016/j.amjcard.2017.03.024
Gohbara M, Iwahashi N, Akiyama E, Maejima N, Tsukahara K, Hibi K, Kosuge M, Ebina T, Umemura S, Kimura K (2016) Association between epicardial adipose tissue volume and myocardial salvage in patients with a first ST-segment elevation myocardial infarction: an epicardial adipose tissue paradox. J Cardiol 68:399–405. https://doi.org/10.1016/j.jjcc.2015.10.018
Buchner S, Satzl A, Debl K, Hetzenecker A, Luchner A, Husser O, Hamer OW, Poschenrieder F, Fellner C, Zeman F, Riegger GA, Pfeifer M, Arzt M (2014) Impact of sleep-disordered breathing on myocardial salvage and infarct size in patients with acute myocardial infarction. Eur Heart J 35:192–199. https://doi.org/10.1093/eurheartj/eht450
Altmann U, Böger CA, Farkas S, Mack M, Luchner A, Hamer OW, Zeman F, Debl K, Fellner C, Jungbauer C, Banas B, Buchner S (2017) Effects of reduced kidney function because of living kidney donation on left ventricular mass. Hypertension 69:297–303. https://doi.org/10.1161/HYPERTENSIONAHA.116.08175
Fisser C, Marcinek A, Hetzenecker A, Debl K, Luchner A, Sterz U, Priefert J, Zeman F, Kohler M, Maier LS, Buchner S, Arzt M (2017) Association of sleep-disordered breathing and disturbed cardiac repolarization in patients with ST-segment elevation myocardial infarction. Sleep Med 33:61–67. https://doi.org/10.1016/j.sleep.2017.01.007
Schmidleitner C, Arzt M, Tafelmeier M, Ripfel S, Fauser M, Weizenegger T, Flörchinger B, Camboni D, Wittmann S, Zeman F, Schmid C, Maier LS, Wagner S, Fisser C (2018) Sleep-disordered breathing is associated with disturbed cardiac repolarization in patients with a coronary artery bypass graft surgery. Sleep Med 42:13–20. https://doi.org/10.1016/j.sleep.2017.12.007
Buller CE, Fu Y, Mahaffey KW, Todaro TG, Adams P, Westerhout CM, White HD, van ’t Hof AW, van de Werf FJ, Wagner GS, Granger CB, Armstrong PW, (2008) ST-segment recovery and outcome after primary percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation 118:1335–1346. https://doi.org/10.1161/CIRCULATIONAHA.108.767772
Sterz U, Buchner S, Hetzenecker A, Satzl A, Debl K, Luchner A, Husser O, Hamer OW, Fellner C, Zeman F, Maier LS, Arzt M (2018) Erratum to: Resolution of ST deviation after myocardial infarction in patients with and without sleep-disordered breathing. Somnologie 22:130. https://doi.org/10.1007/s11818-018-0165-5
Nelson AJ, Worthley MI, Psaltis PJ, Carbone A, Dundon BK, Duncan RF, Piantadosi C, Lau DH, Sanders P, Wittert GA, Worthley SG (2009) Validation of cardiovascular magnetic resonance assessment of pericardial adipose tissue volume. J Cardiovasc Magn Reson 11:15. https://doi.org/10.1186/1532-429X-11-15
Iacobellis G, Malavazos AE, Corsi MM (2011) Epicardial fat: from the biomolecular aspects to the clinical practice. Int J Biochem Cell Biol 43:1651–1654. https://doi.org/10.1016/j.biocel.2011.09.006
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G (2006) User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 31:1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015
Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, Kim RJ, von Knobelsdorff-Brenkenhoff F, Kramer CM, Pennell DJ, Plein S, Nagel E (2013) Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) Board of Trustees Task Force on Standardized Post Processing. J Cardiovasc Magn Reson 15:76. https://doi.org/10.1186/1532-429X-15-35
Eitel I, de Waha S, Wöhrle J, Fuernau G, Lurz P, Pauschinger M, Desch S, Schuler G, Thiele H (2014) Comprehensive prognosis assessment by CMR imaging after ST-segment elevation myocardial infarction. J Am Coll Cardiol 64:1217–1226. https://doi.org/10.1016/j.jacc.2014.06.1194
Fisser C, Götz K, Hetzenecker A, Debl K, Zeman F, Hamer OW, Poschenrieder F, Fellner C, Stadler S, Maier LS, Pfeifer M, Buchner S, Arzt M (2020) Obstructive sleep apnoea but not central sleep apnoea is associated with left ventricular remodelling after acute myocardial infarction. Clin Res Cardiol 39:119. https://doi.org/10.1007/s00392-020-01684-z
Homsi R, Sprinkart A, Gieseke J, Yuecel S, Dabir D, Luetkens JA, Marx C, Kuetting D, Schild HH, Thomas DK (2016) 3D-Dixon cardiac magnetic resonance detects an increased epicardial fat volume in hypertensive men with myocardial infarction. J Cardiovasc Magn Reson 18:O4. https://doi.org/10.1186/1532-429X-18-S1-O4
Hadamitzky M, Langhans B, Hausleiter J, Sonne C, Byrne RA, Mehilli J, Kastrati A, Schomig A, Martinoff S, Ibrahim T (2014) Prognostic value of late gadolinium enhancement in cardiovascular magnetic resonance imaging after acute ST-elevation myocardial infarction in comparison with single-photon emission tomography using Tc99m-Sestamibi. Eur Heart J Cardiovasc Imaging 15:216–225. https://doi.org/10.1093/ehjci/jet176
de Waha S, Patel MR, Granger CB, Ohman EM, Maehara A, Eitel I, Ben-Yehuda O, Jenkins P, Thiele H, Stone GW (2017) Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: an individual patient data pooled analysis from seven randomized trials. Eur Heart J 38:3502–3510. https://doi.org/10.1093/eurheartj/ehx414
van Kranenburg M, Magro M, Thiele H, de Waha S, Eitel I, Cochet A, Cottin Y, Atar D, Buser P, Wu E, Lee D, Bodi V, Klug G, Metzler B, Delewi R, Bernhardt P, Rottbauer W, Boersma E, Zijlstra F, van Geuns R-J (2014) Prognostic value of microvascular obstruction and infarct size, as measured by CMR in STEMI patients. JACC Cardiovasc Imaging 7:930–939. https://doi.org/10.1016/j.jcmg.2014.05.010
Alam MS, Green R, de Kemp R, Beanlands RS, Chow BJW (2013) Epicardial adipose tissue thickness as a predictor of impaired microvascular function in patients with non-obstructive coronary artery disease. J Nucl Cardiol 20:804–812. https://doi.org/10.1007/s12350-013-9739-6
Stiermaier T, Thiele H, Eitel I (2017) Coronary microvascular obstruction. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.117.006568
Dizon JM, Brener SJ, Maehara A, Witzenbichler B, Biviano A, Godlewski J, Parise H, Dambrink J-H, Mehran R, Gibson CM, Stone GW (2014) Relationship between ST-segment resolution and anterior infarct size after primary percutaneous coronary intervention: Analysis from the INFUSE-AMI trial. Eur Heart J Acute Cardiovasc Care 3:78–83. https://doi.org/10.1177/2048872613508658
Arzt M (2020) Update – schlafbezogene Atmungsstörungen. Somnologie 24:28–38. https://doi.org/10.1007/s11818-020-00239-8
Chang H-X, Zhao X-J, Zhu Q-L, Hou Q, Li Y (2018) Entfernung von epikardialem Fettgewebe nach Herzinfarkt verbessert die Herzfunktion. Herz 43:258–264. https://doi.org/10.1007/s00059-017-4555-4
McKenney ML, Schultz KA, Boyd JH, Byrd JP, Alloosh M, Teague SD, Arce-Esquivel AA, Fain JN, Laughlin MH, Sacks HS, Sturek M (2014) Epicardial adipose excision slows the progression of porcine coronary atherosclerosis. J Cardiothorac Surg 9:2. https://doi.org/10.1186/1749-8090-9-2
Sacks HS, Fain JN (2011) Human epicardial fat: What is new and what is missing? Clin Exp Pharmacol Physiol 38:879–887. https://doi.org/10.1111/j.1440-1681.2011.05601.x
Rezkalla SH, Kloner RA (2002) No-reflow phenomenon. Circulation 105:656–662. https://doi.org/10.1161/hc0502.102867
Engler RL, Schmid-Schönbein GW, Pavelec RS (1983) Leukocyte capillary plugging in myocardial ischemia and reperfusion in the dog. Am J Pathol 111:98–111
Sade LE, Eroglu S, Bozbaş H, Ozbiçer S, Hayran M, Haberal A, Müderrisoğlu H (2009) Relation between epicardial fat thickness and coronary flow reserve in women with chest pain and angiographically normal coronary arteries. Atherosclerosis 204:580–585. https://doi.org/10.1016/j.atherosclerosis.2008.09.038
Cheng K-H, Chu C-S, Lee K-T, Lin T-H, Hsieh C-C, Chiu C-C, Voon W-C, Sheu S-H, Lai W-T (2008) Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Int J Obes (Lond) 32:268–274. https://doi.org/10.1038/sj.ijo.0803726
Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, Sarov-Blat L, O’Brien S, Keiper EA, Johnson AG, Martin J, Goldstein BJ, Shi Y (2003) Human epicardial adipose tissue is a source of inflammatory mediators. Circulation 108:2460–2466. https://doi.org/10.1161/01.CIR.0000099542.57313.C5
Ito T, Nasu K, Terashima M, Ehara M, Kinoshita Y, Ito T, Kimura M, Tanaka N, Habara M, Tsuchikane E, Suzuki T (2012) The impact of epicardial fat volume on coronary plaque vulnerability: Insight from optical coherence tomography analysis. Eur Heart J Cardiovasc Imaging 13:408–415. https://doi.org/10.1093/ehjci/jes022
Newman AB (2005) Progression and regression of sleep-disordered breathing with changes in weight. Arch Intern Med 165:2408. https://doi.org/10.1001/archinte.165.20.2408
Acknowledgements
The authors are grateful for the excellent assistance provided by Astrid Brandl-Novak, Astrid Braune, Ruth Luigart, and Katja Ziczinski.
Funding
Open Access funding enabled and organized by Projekt DEAL. The study was funded by Resmed (Martinsried, Germany), Philips Respironics (Murrysville, PA, USA), and the Faculty of Medicine of the University of Regensburg, Germany.
Author information
Authors and Affiliations
Contributions
S.B. and M.A. were responsible for conceiving and designing the study and its hypotheses, acquiring study funding, collecting, analyzing and interpreting the data, and writing and revising the manuscript prior to submission. C.F. and S.C. were involved in the collection, analysis and interpretion of data, and were responsible for drafting and revising the manuscript prior to submission. K.D., A.H., U.S., O.W.H., Cl.F. and L.S.M. were involved in the collection and interpretation of data and critical revision of the manuscript prior to submission.
Corresponding author
Ethics declarations
Conflict of interest
M.A.: grant support from ResMed, the ResMed Foundation, Philips Respironics and lecture and consulting fees from ResMed, Philips Respironics, Boehringer-Ingelheim, NRI, Novartis and Bresotec. C.F., S.C., K.D., A.H., U.S., O.W.H., Cl.F., L.S.M., S.B.: no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fisser, C., Colling, S., Debl, K. et al. The impact of epicardial adipose tissue in patients with acute myocardial infarction. Clin Res Cardiol 110, 1637–1646 (2021). https://doi.org/10.1007/s00392-021-01865-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01865-4