Abstract
Background: Optimal deployment of coronary stents in a bifurcation lesion remains a matter of debate.
Aims: We sought to capture the daily practice of bifurcation stenting by means of a worldwide registry and to investigate how post-implantation deployment techniques influence clinical outcomes.
Methods: Data from the e-ULTIMASTER registry were used to perform an analysis of 4,395 patients undergoing percutaneous coronary intervention for bifurcation lesions. Inverse probability of treatment weights (IPTW) propensity score methodology was used to adjust for any baseline differences. The primary outcome of interest was target lesion failure (TLF) at one year (follow-up rate 96.2%).
Results: The global one-year TLF rate was low (5.1%). The proximal optimisation technique (POT) was used in 33.9% of cases and was associated with a reduction in the adjusted TLF rate (4.0% [95% confidence interval: 3.0-5.1%] vs 6.0% [5.1-6.9%], p<0.01) due to a reduction of all components of this composite endpoint, except for cardiac death. Stent thrombosis was also positively impacted (0.4% [0.04-0.7%] vs 1.3% [0.8-1.7%], p<0.01). POT benefit was uniform across subgroups. Conversely, the use of the kissing balloon technique (36.5%) did not influence the adjusted TLF rate.
Conclusions: Despite a low one-year failure rate in this large bifurcation stenting cohort, POT was associated with a further reduction in the event rate and a uniform benefit across subgroups, suggesting systematic use of this deployment technique regardless of the bifurcation anatomy and stenting technique.
Introduction
Bifurcation lesions remain a challenge in terms of both procedural success and long-term cardiovascular outcomes1. Many stenting techniques have been proposed to overcome these limitations from the early days of the bare metal stent era until the advent of new-generation drug-eluting stents (DES)2. Most of them aim at restoring the natural bifurcation anatomy whilst conforming to a wide range of configurations in terms of diameters and angulation. Early results of the two-stent approach prompted the European Bifurcation Club to strongly promote the provisional strategy as a one-stent strategy when acceptable, which was associated with a better or neutral outcome in several randomised clinical trials and most meta-analyses3.
The one-stent technique and two-stent techniques were developed in combination with two major post-dilatation methods to adjust a regular stent to the dedicated anatomy of a bifurcation - the kissing balloon technique (KBT)4 and the proximal optimisation technique (POT)5. Expert consensus has progressively established their respective roles, emphasising the need to respect the fractal geometry of the coronary vasculature6. Although the KBT was evaluated in randomised trials7, recommendations regarding POT have been based mainly on bench testing and small size cohort clinical studies by means of intravascular imaging8,9,10,11,12.
On the basis of the e-ULTIMASTER study13, we sought to evaluate post-stent implantation deployment techniques, with specific focus on POT and KBT, and their impact on the one-year clinical outcome of a large pre-specified bifurcation subgroup of this worldwide prospective mega-registry.
Methods
STUDY DESIGN
e-ULTIMASTER (NCT02188355) is an all-comer, single-arm, prospective, multicentre registry with clinical follow-up at three months and one year. The study was conducted worldwide and enrolled patients between October 2014 and June 2018 from 378 hospitals (Supplementary Appendix 1) in 50 countries across Europe, Asia, Africa, South America and Mexico13. The primary objective of the registry was to evaluate further the safety and performance of the Ultimaster® DES system (Terumo Corporation, Tokyo, Japan) in daily practice.
STUDY POPULATION
Inclusion criteria were broad and involved all patients ≥18 years old, with coronary artery disease eligible for percutaneous coronary intervention (PCI) using DES according to local hospital practice and intended to be treated with the Ultimaster DES (with reference vessel diameter matching available Ultimaster DES sizes). Dual antiplatelet regimen was left to the operators’ discretion. The registry was conducted in accordance with the Declaration of Helsinki and country-specific regulatory requirements. All patients signed the informed consent form reviewed and approved by the Institutional Review Board/Ethics Committee of each participating centre. A bifurcation lesion is defined as a significant stenosis in a coronary artery adjacent to and/or involving the origin of a side branch (SB) that is clinically significant. Selection of patients in the bifurcation cohort was at the operator’s discretion.
The study population used to analyse clinical outcomes during follow-up comprised all patients who received an Ultimaster DES upon enrolment in the e-ULTIMASTER study and (i) completed one-year follow-up, or (ii) who reached the primary endpoint target lesion failure (TLF: cardiac death, target vessel myocardial infarction [TVMI] or clinically driven target lesion revascularisation [TLR]), or (iii) who died during follow-up (Figure 1).
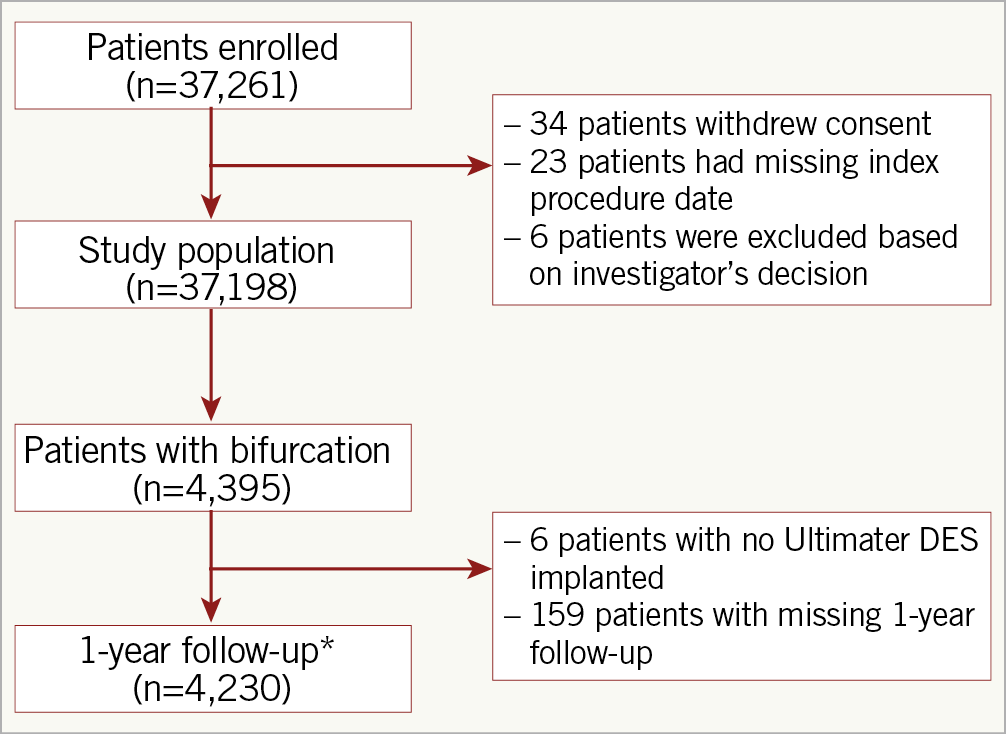
Figure 1. Flow chart of the study population. *The one-year follow-up population includes patients who had an event that contributed to the primary endpoint, died during follow-up or completed one-year follow-up.
STUDY DEVICE
The Ultimaster coronary stent system is a new-generation open-cell cobalt-chromium thin-strut (80 µm) sirolimus-eluting stent with an abluminal biodegradable polymer coating (poly-D,L-lactic acid polycaprolactone)14. Sirolimus is released over a 3- to 4-month period after which the polymer coating is fully degraded.
FOLLOW-UP
Follow-up was performed either via direct phone contact with the patient or during a visit of the patient to the outpatient clinic of the hospital. Measures to ensure data quality included remote and on-site monitoring with a risk-based approach as well as close communication with the sites to reinforce the importance of complete and accurate data entry. All events composing the primary endpoint were independently adjudicated by a clinical events committee.
OUTCOMES AND DEFINITIONS
The primary outcome was TLF, defined as a composite of cardiac death, myocardial infarction that could not be clearly attributed to a vessel other than the target vessel (TVMI) and clinically driven target lesion revascularisation (CD-TLR). Secondary outcomes included any death, cardiac death, MI, TLR, target vessel revascularisation (TVR), target vessel failure (TVF, a composite of cardiac death, TVMI and TVR), stent thrombosis (ST) and major vascular and bleeding complications.
STATISTICAL ANALYSIS
Baseline patient, lesion and procedural characteristics are summarised using mean±standard deviation (SD) for continuous variables and frequencies and percentages for categorical variables. Continuous variables were compared using the Wilcoxon test and categorical variables with the chi-square test. To account for differences in baseline demographics, the POT versus no POT and KBT versus no KBT comparisons were adjusted by weighting the subject by inverse propensity weights. These propensity scores were calculated using a logistic regression model, predicting the probability of belonging to the POT or KBT group, with the baseline demographic variables as independent variables (age, gender, smoking status, renal impairment, previous MI, previous PCI, previous coronary artery bypass grafting [CABG], acute coronary syndrome, ST-elevation myocardial infarction [STEMI], multivessel disease, number of lesions identified and treated, treated vessel location, small vessels, long lesions, lesion type B2 or C, ostial lesions, chronic total occlusion [CTO], calcification, Medina classification, one- versus two-stent technique, number of stents implanted, total stent length, radial access, balloon predilatation, balloon post-dilatation, imaging). Propensity scores for POT versus no POT additionally included KBT, while propensity scores for KBT versus no KBT additionally included POT. The inverse weights were investigated for extreme values (Supplementary Figure 1). Due to the large overlap in populations and the large sample sizes, neither the POT nor the KBT propensity score matching resulted in extreme weights (maximum weights <4).
In the propensity score weighted analyses, categorical variables were compared with a weighted chi-square test. For time-to-event analysis, an inverse propensity score weighted Kaplan-Meier method was applied. Logistic regression was used to test the interaction effect for POT or KBT separately versus a list of predictor variables on one-year TLF, by modelling, per predictor variable, the one-year TLF as binary outcome, while using POT or KBT and the predictor variable as independent variables, and the interaction between POT or KBT and the predictor variable as interaction effect. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
At least one bifurcation lesion was treated in 4,395 patients, 11.8% of the 37,198 patients enrolled in the e-ULTIMASTER registry, among whom 4,230 patients (96.2%) were followed up to one year. Baseline and procedural characteristics of this bifurcation cohort are shown in Table 1. More than half of the patients were treated on a true bifurcation lesion (Medina x,x,1: 52.2%), mainly in the left anterior descending coronary artery (LAD) (68.4%) via radial access in 80.2% of cases. A double (main and side branches) vessel treatment was carried out in 51.8% and a double stenting was performed in 22.8%, reflecting a high incidence of adoption of a provisional strategy. Details of techniques are presented in Supplementary Figure 2. At the one-year endpoint, the TLF rate was 5.1%; each component of the composite endpoint is described in Figure 2.
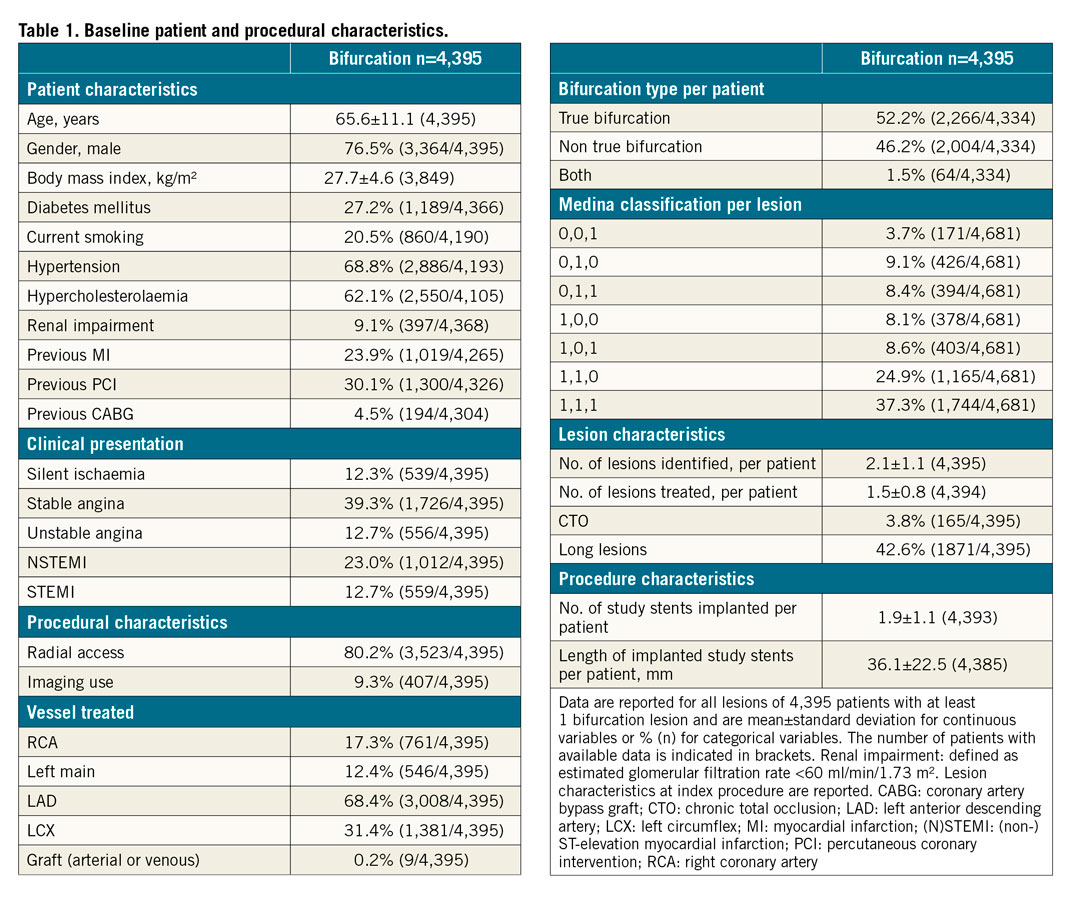
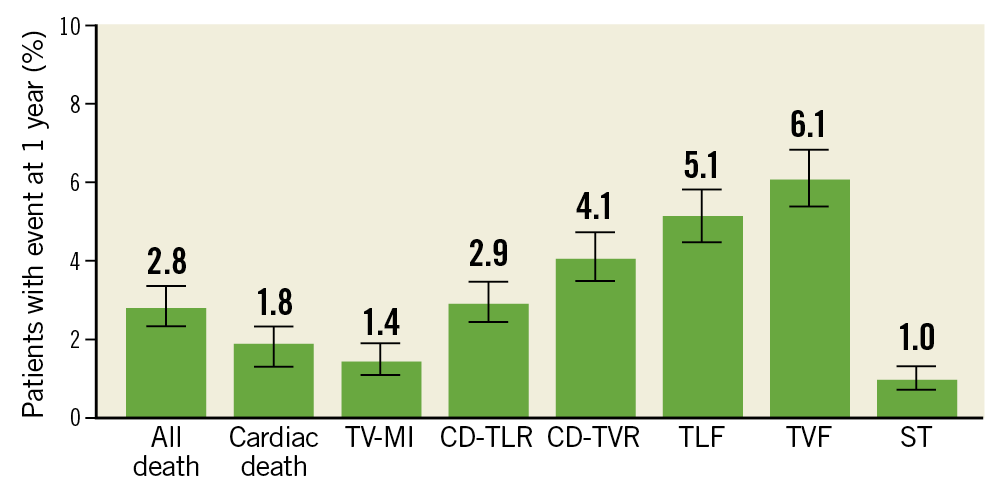
Figure 2. Unadjusted one-year clinical outcomes of all bifurcation patients (N=4,230). CD-TLR clinically driven target lesion revascularisation; CD-TVR clinically driven target vessel revascularisation; ST: stent thrombosis; TLF: target lesion failure; TVF: target vessel failure; TV-MI target vessel myocardial infarction
POT was performed in 33.9% of cases. Its use was more prevalent in left main (LM) and LAD lesions as well as in long lesions, true bifurcations, and when a two-stent technique was used (Table 2). KBT was performed in 36.5% of cases; its use was heterogeneous regarding the main baseline characteristics (Supplementary Table 1). Unadjusted and adjusted (inverse propensity score weighted) outcomes according to POT and KBT use are presented in Table 3 and Supplementary Table 2.
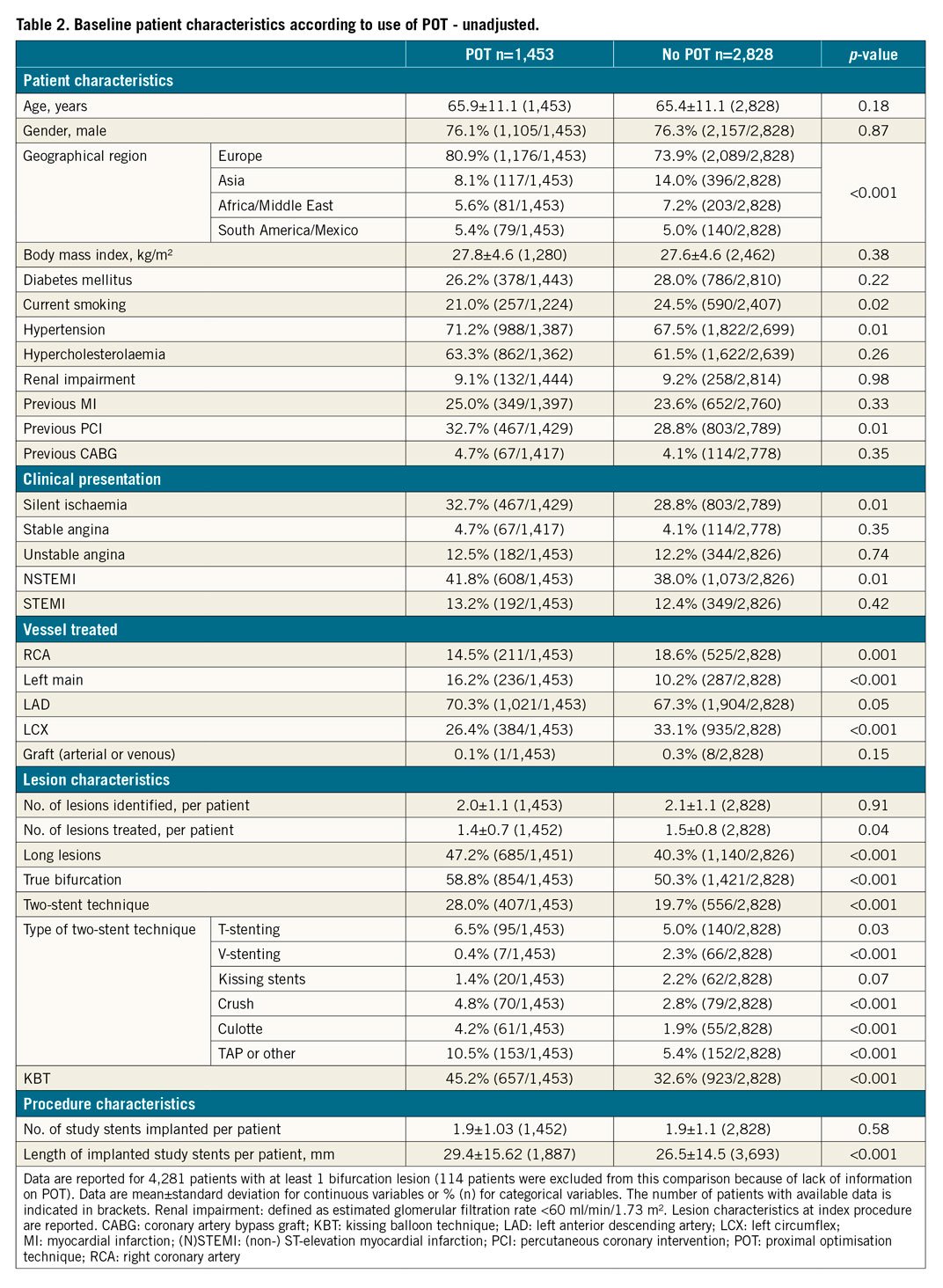
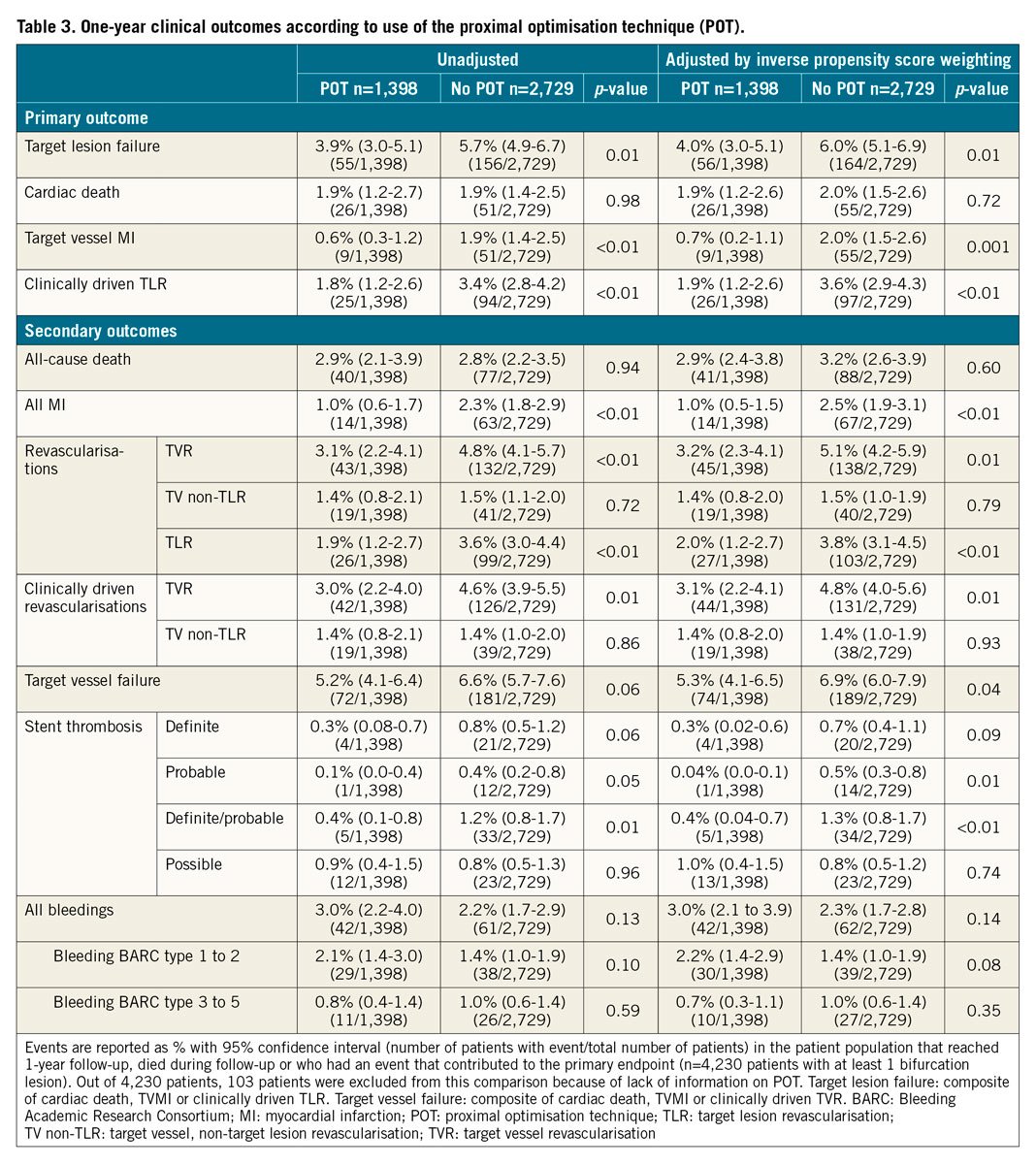
The baseline characteristics of the study population after propensity weighting are shown in Supplementary Table 3 (POT vs no POT) and Supplementary Table 4 (KBT vs no KBT). After propensity weighting, POT was associated with a reduction of TVMI (0.7% [0.2-1.1%] vs 2.0% [1.5-2.6%], p=0.001), CD-TLR (1.9% [1.2-2.6%] vs 3.6% [2.9-4.3%], p<0.01), ST (0.4% vs 1.3%, p<0.01) with a strong impact on TLF (4.0% [3.0-5.1%] vs 6.0% [5.1-6.9%], p<0.01). POT benefit was consistent across the subgroups (p for interaction=NS) with regard to major angiographic and procedural features (Figure 3). The difference was established early, during the first month, and maintained during the first year (Central illustration).
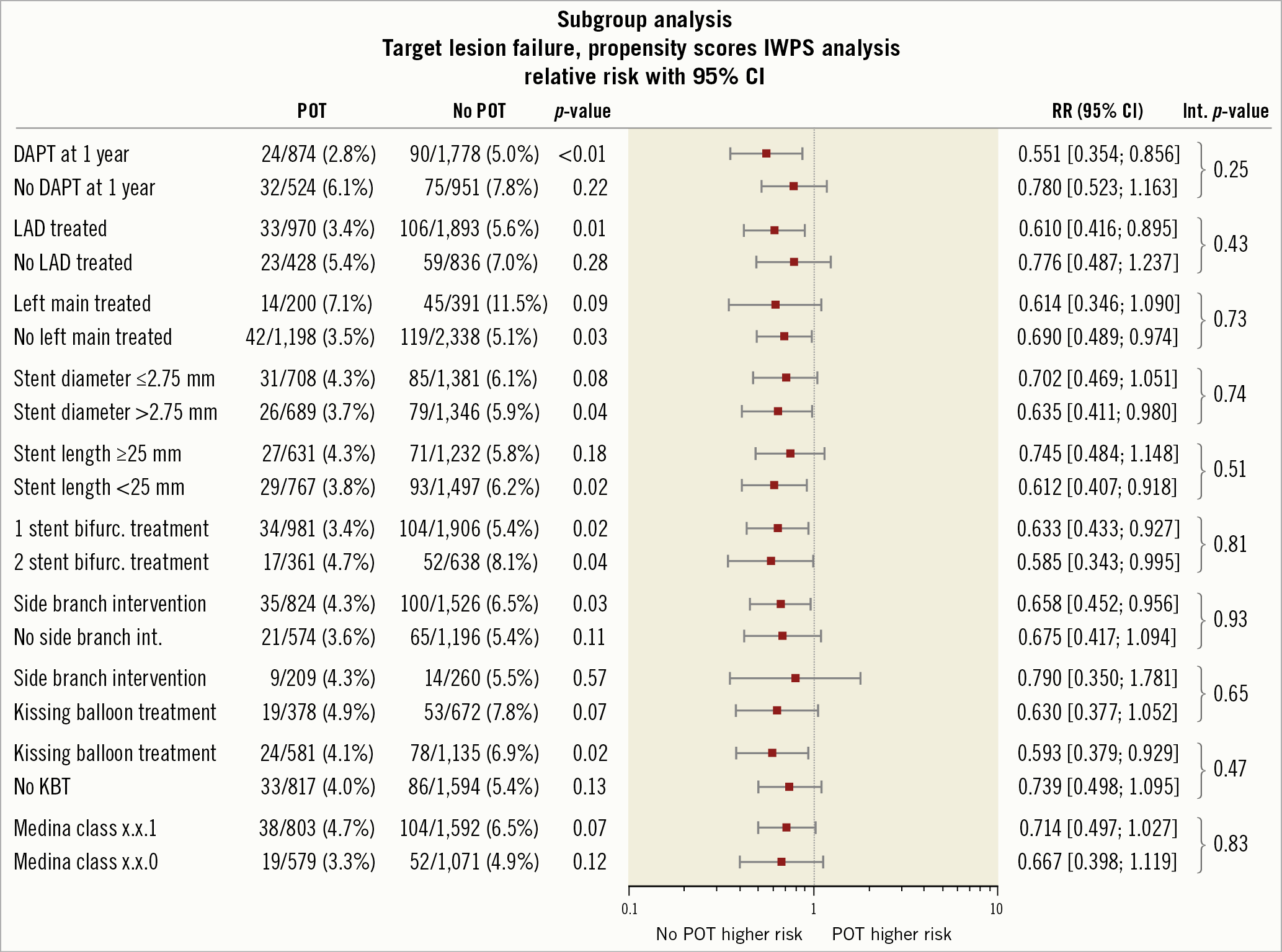
Figure 3. Impact of POT in major angiographic and procedural subgroups - inverse propensity score weighted analysis. DAPT: duel anti platelet therapy; KBT: kissing balloon technique; LAD: left anterior descending coronary artery; POT: proximal optimisation technique
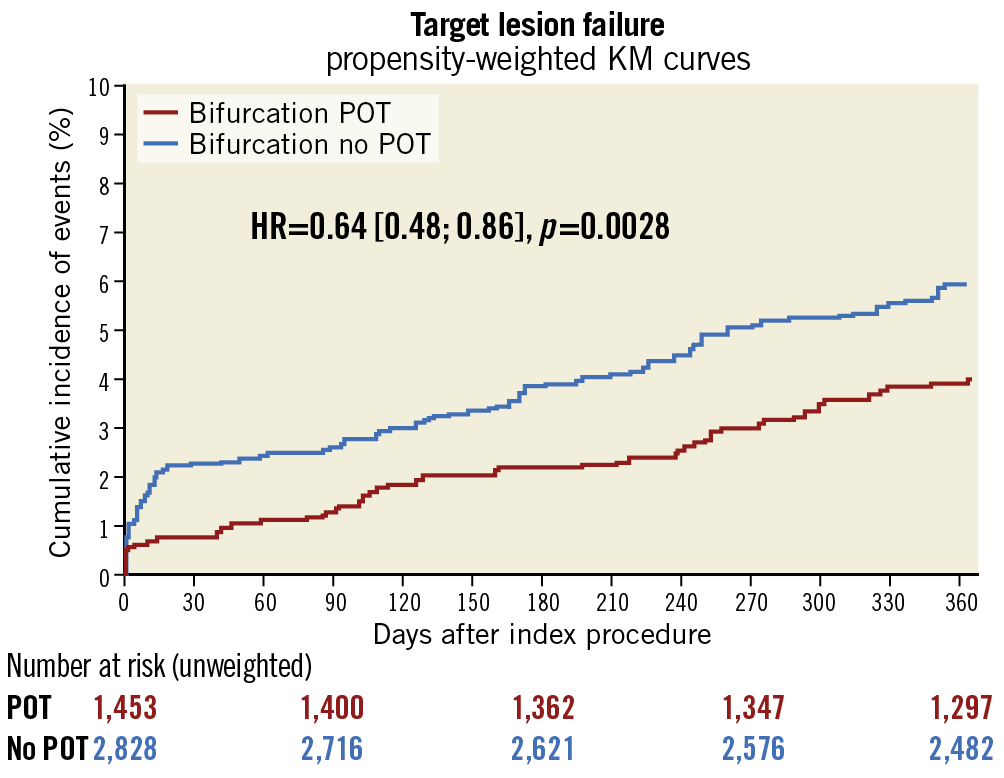
Central illustration. POT versus no POT: inverse propensity score weighted Kaplan-Meier curve of target lesion failure. KM: Kaplan Meier; POT: proximal optimisation technique
KBT had a limited clinical impact on clinical outcomes with a reduction in TVMI after propensity weighting (1.0% [0.5-1.5%] vs 1.9% [1.4-2.4%], p=0.02) with no effect on the one-year composite endpoint TLF (4.5% [3.5-5.6%] vs 4.7% [3.9-5.5%], p=0.77) or on ST rates (0.9% [0.4-1.4%] vs 0.8% [0.5-1.2%], p=0.76). There was an interaction between KBT effect and some procedural characteristics: LM location, Medina type, stent size and persistent dual antiplatelet therapy (DAPT) at one year (Supplementary Figure 3). Details of this analysis are presented in Supplementary Table 2.
Discussion
To the best of our knowledge, this is the largest bifurcation study aiming at assessing the respective impact of post-stent implantation deployment techniques, namely POT and KBT. Our study shows, first, a low one-year event rate in this large registry capturing the real-world practice in bifurcation stenting when using a latest-generation DES despite a surprisingly low rate of POT, second, a strong impact of POT on one-year clinical outcomes which is consistent across subgroups, and third, a minimal effect of KBT on outcomes.
FROM FRACTAL GEOMETRY TO POT
The law of conservation of mass, also known as Murray’s law, established the fractal geometry15 of artery bifurcations. A simplification of this rule, suggested by Finet et al16, was validated by means of quantitative angiography and intravascular ultrasound (IVUS) and allows the quantification of the step-up of proximal main branch reference diameter according to the distal main branch and side branch reference diameters. In order to minimise the risk of carina shift after main branch stent implantation, and the subsequent risk of side branch occlusion inducing a periprocedural MI, a 1:1 stent diameter/distal reference diameter ratio was proposed by Darremont at the 5th European Bifurcation Club meeting5 in combination with a 1:1 balloon post-dilatation just proximal to the carina, sized on the basis of a simplified Murray’s law, to eliminate undersizing, and subsequent malapposition in the proximal segment of the bifurcation and to facilitate access to the side branch by reducing strut obstruction. This concept of two diameters with a single stent allows the transformation of a regular stent in order to comply with the fractal nature of the coronary tree.
POT VALIDATION
Despite this strong rationale and the intuitive benefit, few studies have been performed to validate this strategy. This could be the reason why the POT was used only in one third of our bifurcation registry despite strong recommendations by the various bifurcation clubs. Rigatelli et al17 showed a significant improvement in terms of flow dynamics when POT is used on bench models with some two-stent techniques. Derimay et al emphasised the impact of balloon position to obtain the expected effect on bench testing10 and highlighted differences between balloon brands in terms of marker to shoulder distances.
Some studies used intravascular imaging to evaluate the potential benefit with contradictory results. Hakim et al8 showed that POT increased proximal stent area, as assessed by IVUS, while Murasato et al did not obtain the expected benefit on incomplete stent apposition as assessed by optical coherence tomography (OCT)9. Few clinical studies have been conducted so far. Mylotte et al evaluated the role of POT among other modifications of the provisional strategy to improve clinical outcome18. Takagi et al studied a series of 586 patients treated on LM bifurcation lesions, showing a strong trend towards major adverse cardiac events (MACE) and TLR reductions (hazard ratio [HR] 0.73 and 0.69, p=0.05 and 0.06) when POT was performed19. More recently, Yang et al12, in a series of 1,191 bifurcation lesions with a 21.1% POT rate, showed a benefit in terms of MACE and TLR when no KBT was performed (p for interaction=0.03). Our results in a much larger cohort found an early and sustained benefit in terms of safety - ST and TVMI –and efficacy– TVR with no interaction with major angiographic and procedural characteristics.
ROLE OF THE KISSING BALLOON TECHNIQUE
In our study, KBT was not associated with a TLF benefit after propensity weighting, a result which is consistent with data from NORDIC III7 in which KBT failed to prove an impact on a provisional stenting strategy. However, the KBT subgroup, despite worse baseline characteristics, experienced less TVMI without any difference in terms of ST, a finding which could be related to less side branch periprocedural obstruction with no further effect on the TLR rate. Conversely, registry data have shown a late revascularisation benefit, as shown in COBIS II20 and RAIN21. However, guidelines22 recommend using KBT in two-stent techniques. A significant interaction was present with some baseline angiographic characteristics and DAPT duration but the KBT effect was similar regardless of the number of stents and the deployment technique.
The question as to whether KBT and POT are complementary techniques is still a matter of debate as both techniques are implemented to reduce proximal malapposition and to facilitate further access to the side branch. In our study, POT and KBT practices were more frequently associated than dissociated.
Given the low event rates, it is important to remove as much of the variability induced by the confounding factors as possible. For this purpose, we performed propensity-matched POT and KBT analyses. In order to identify the combined effects of POT and KBT in our study population more clearly, we used logistic regression models where we included both POT and KBT as predictive factors of one-year TLF (Supplementary Table 5), together with their interaction effect and the covariates we used in propensity score weighting. From the multivariate model, it seems that POT only (p=0.046), rather than KBT (p=0.81) or their interaction effect (p=0.76), is the protective factor for TLF in our study. Additionally, we performed 2 by 2 propensity-matched analyses, classifying patients by their POT and KBT status into four groups: (1) using POT and KBT, (2) using POT but no KBT, (3) using KBT but no POT, and (4) neither POT nor KBT used (Supplementary Table 6). These results corroborate the results from the logistic regression models: POT is the protective factor for TLF, while KBT or the POT-KBT interaction does not seem to play a major role. These data suggest that KBT cannot be a substitute for the POT technique.
Limitations
First, due to the registry design, there is a potential for selection bias and under-reporting of events despite the prospective nature of the study and the specific measures undertaken to improve data quality using on- and off-site monitoring. In particular, an underestimation of periprocedural MI cannot be excluded as periprocedural biomarker collection was per hospital practice. Second, vessel and lesion characteristics were assessed by operators, most commonly through visual estimation, and not measured centrally by a core lab. Third, deployment technique details are limited in terms of size selection and inflation technique. Sequence description data with regard to POT and KBT are missing, even though the latter was always performed after stenting; moreover, a small number of patients were treated under intravascular imaging guidance, limiting the extrapolation of these results to intravascular imaging-guided interventions. Fourth, the outcomes reported are based on the use of a single new-generation stent platform for all patients; these may potentially differ with the use of different DES. Fifth, as the antiplatelet regimen nature and duration was left to the operator’s discretion, interaction with deployment techniques is unknown. Finally, although we report a follow-up of one year, coronary stents are lifelong implants; it is possible that further differences between our study groups could be observed at longer follow-up.
Conclusions
In this large prospective single-arm study with an already low one-year failure rate in the bifurcation stenting cohort, the proximal optimisation technique was associated with a further reduction in the event rate and a uniform benefit across subgroups, reinforcing the recommendation for a systematic use of this deployment technique regardless of the bifurcation anatomy and stenting technique.
|
Impact on daily practice This large bifurcation subgroup from a global registry using a latest-generation DES shows a low one-year event rate with significant clinical improvement when the proximal optimisation technique was performed. The kissing balloon technique has a more limited influence on the outcome. The current findings suggest a benefit of the proximal optimisation technique irrespective of the lesion anatomy and the stenting technique, promoting its systematic use. |
Funding
The e-Ultimaster registry was funded and sponsored by Terumo Europe NV (Leuven, Belgium).
Conflict of interest statement
B. Chevalier reports grants from Terumo during the conduct of the study, personal fees from Terumo, outside the submitted work, and being a minor shareholder of CERC (CRO). M. Mamas has the following interests to declare: unrestricted educational grants from Terumo, Abbott, Medtronic and Biosensors, and speaker fees from Terumo, Daiichi Sankyo and Biosensors. M. Pan reports minor lecture fees from Abbott, Terumo and Volcano. F.F. Beygui reports grants from Terumo during the conduct of the study, grants and personal fees from Medtronic and Biosensor, and personal fees from Bristol Myers Squibb, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.