Abstract
The echocardiographic assessment of mitral valve regurgitation (MR) by characterizing specific morphological features and grading its severity is still challenging. Analysis of MR etiology is necessary to clarify the underlying pathological mechanism of the valvular defect. Severity of mitral regurgitation is often quantified based on semi-quantitative parameters. However, incongruent findings and/or interpretations of regurgitation severity are frequently observed. This proposal seeks to offer practical support to overcome these obstacles by offering a standardized workflow, an easy means to identify non-severe mitral regurgitation, and by focusing on the quantitative approach with calculation of the individual regurgitant fraction. This work also indicates main methodological problems of semi-quantitative parameters when evaluating MR severity and offers appropriateness criteria for their use. It addresses the diagnostic importance of left-ventricular wall thickness, left-ventricular and left atrial volumes in relation to disease progression, and disease-related complaints to improve interpretation of echocardiographic findings. Finally, it highlights the conditions influencing the MR dynamics during echocardiographic examination. These considerations allow a reproducible, verifiable, and transparent in-depth echocardiographic evaluation of MR patients ensuring consistent haemodynamic plausibility of echocardiographic results.
Graphic abstract

Similar content being viewed by others
Introduction
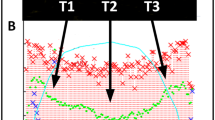
The most frequently used tool for mitral regurgitation (MR) quantification in clinical practice is “eyeballing” of the colour flow jet area to differentiate between mild and severe MR [1]. This practice is primarily explained by its ease of use. However, it seems inadequate to solely use a qualitative diagnostic parameter to distinguish between mild, moderate, and severe MR [2,3,4,5]. As mentioned in recent recommendations, “eyeballing” of the MR jet area is misleading [3, 5, 6]. This is caused by its variations depending on ultrasound settings (Fig. 1), the different display of the jet area in respective sectional planes, and the haemodynamic variations influencing MR dynamics. In consequence, recent papers had eliminated this method in the respective tables [6, 7]. The key point statements—“The colour flow area of regurgitant jet is not recommended to quantify the severity of MR. The colour flow imaging should only be used for diagnosing MR. A more quantitative approach is required when more than a small central MR jet is observed” [3]—emphasize the necessity of a definite quantitative approach for grading MR severity.
The methodological factors influencing color-coded flow phenomena (PISA, VC, jet area)—illustrated by optimal colour Doppler settings with 1.8 MHz Doppler frequency, increased Doppler sample volume, reduced low-velocity reject, increased frame rate, increased Doppler frequency with 3.1 and 3.6 MHz, increased colour pixel smoothing, reduced colour scale, reduced and increased 2D gain, reduced and increased colour gain, reduced and increased 2D priority, and reduced and increased zero line shift
At the same time, semi-quantitative and/or quantitative parameters, such as the 2D-PISA (proximal isovelocity surface area) method, are used by a minority of primary care physicians and cardiologists [1], whereas in clinical trials, it is the most frequently used method for MR quantification [8,9,10,11].
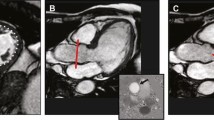
Although recent recommendations describe the numerous limitations of the 2D-PISA method, making its use difficult, one key point message remains, namely “When feasible, the PISA method is highly recommended to quantify the severity of MR” [3]. However, the exact way of measuring of the 2D-PISA radius is unclear, as illustrated in Fig. 2. In the recent guidelines [5] “The radius of PISA is measured from the point of color Doppler aliasing to the VC (vena contracta)”. However, the 2D-PISA radius is illustrated in this recommendation [5], in the first description of the method [12], and in several other references [13] from the proximal convergence area to the ostium of the regurgitant orifice. This discrepancy is not clearly analysed in the literature [5, 13,14,15]—especially using modern colour Doppler technologies. Also, the impact of MR jet orientation is being debated controversially when using the 2D-PISA method. While some recommendations advise the use of the 2D-PISA in both central and eccentric jets [3, 16], others advise caution [15].
Limitations of the 2D-PISA method (PISA radius = r)—scheme of the proximal convergence areas and the proximal regurgitant flow phenomenon through the regurgitant orifice illustrating the importance of the accurate definition of the 2D-PISA radius. Example of regurgitant volume (MVRegVol) assessment using different 2D-PISA radii with equal velocity time integrals of regurgitant velocities (r = 8 mm, MVRegVol = 19 ml; r = 11 mm, MVRegVol = 39 ml; r = 15 mm, MVRegVol = 67 ml)
These two mainly used diagnostic features—the colour flow jet area and the 2D-PISA method—are complemented by additional semi-quantitative parameters, which eventuate in the “integrated approach” of MR quantification [3, 5, 6, 16]. However, all these semi-quantitative parameters have their limitations and can only be used in certain circumstances [13, 17,18,19]. A summary of the strengths and limitations of semi-quantitative parameters for grading of MR severity and the conditions when to apply or not to apply the respective parameters is particularized in Table 1. Considering the methodological challenges of the integrated approach, several concerns of semi-quantitative grading of MR severity should be considered to reduce the inter-observer variability to characterize more precisely and objectively MR severity. The dynamic nature of MR—especially with respect to loading conditions—cause a variability of MR quantification in clinical practice [20,21,22]. Thus, especially in secondary MR (SMR) recommendations favour the approach of MR assessment at compensated stage [16].
The assessment of MR and the grading of its severity remain challenging today. It is the objective of this work to present tools for an in-depth analysis of the MR, taking practical, methodological, and pathophysiological aspects into consideration. To improve diagnostic conclusiveness the quantitative approach of MR assessment by determining left ventricular (LV) total and effective stroke volume (LVSVtot, LVSVeff), regurgitant volume at the mitral valve level (MVRegVol) and regurgitant fraction (RF) is highlighted.
A proposal for a standardized workflow of the echocardiographic MR assessment
A standardized workflow during the echocardiographic examination and the patient`s visit is necessary to ensure a reproducible and verifiable MR assessment as well as documentation of treatment effects in MR patients. Patient`s characteristics and clinical parameters must be considered for therapeutic decision-making. Indexing of several echocardiographic parameters is based on body height, body weight, and surface area. Systemic blood pressure enables estimation of LV afterload. Clinical symptoms and their progression as well as alterations of echocardiographic parameters with disease progression are important to decide the necessity of therapeutic interventions. At last, age and comorbidities are not influencing MR severity, but are important to estimate the individual patients’ risk. Multiple factors cause differences in MR severity in the same patient at different time points, e.g., cardioversion of atrial fibrillation (AF) into sinus rhythm, resynchronisation therapy in patients with left bundle branch block (LBBB), optimized medical treatment (OMT) in heart failure, or revascularization in myocardial ischemia. To ensure comparability of echocardiographic investigations MR assessment should be performed according to recent recommendations at compensated stage [16].
The echocardiographic examination should consider and interpret the clinical symptoms, and the individual patient`s factors in relation to the presumed valvular defect (Figs. 3, 4). After qualitative MR detection by Doppler techniques, the next diagnostic steps by echocardiography should be the assessment of mitral valve (MV) morphology, LV wall thickness, left atrial (LA), and LV volume as well as LV shape and remodelling, prior to grading MR severity (Figs. 3, 4). Thereafter, a semi-quantitative MR assessment is advised, which should be followed by a quantification of MR severity, if moderate or severe MR is being suspected, or if severity of MR remains unclear (Fig. 4). Every changes of MR severity documented by repetitive standardized echocardiography should be noted to enable reliable conclusions about the respective treatment effects. Figure 5 depicts a recommended timeline for performing echocardiographic examinations in patients with significant MR who are considered for interventional/surgical treatment of MR.
Scheme to illustrate the diagnostic steps to assess MR by TTE: The first step includes the interpretation of clinical symptoms and the chronicity of the underlying disease in the context of MR with different severity. The second step is the qualitative detection of MR. The third step is the analysis of MV morphology and the differentiation between PMR and SMR. The fourth step is the assessment of LV wall, LA- and LV volumes as well as LV size and LV remodelling to get insights into MR etiology, MR chronicity, and LV geometry. The last step is the grading of MR severity. HOCM hypertrophic cardiomyopathy, LA left atrial, LV left ventricular, LVEDP LV end-diastolic pressure, LVRI LV remodelling index, MR mitral regurgitation, MV mitral valve, PMR primary MR, RWT relative wall thickness, SMR secondary MR, sPAP systolic pulmonary arterial pressure
Scheme to illustrate the echocardiographic workflow to assess MR severity: After interpretation of symptomatology with respect to the causal relationship to the MR qualitative MR detection results in MR classification due to the MV morphology. Echocardiographic parameters of LA and LV size and LV wall thickness characterize loading conditions and enable to distinguish between pressure or volume overload and between compensated or decompensated conditions. The assessment of MR severity starts with the integrated approach and the analysis of semi-quantitative parameters. The final experts’ task of analysis of MR severity is the quantitative assessment of LVSVtot, LVSVeff, MVRegVol, and RF as a plausibility check. At every level of the assessment of MR severity expert consultation as well as the quantitative analysis of MR severity should be considered with respect to severe symptoms, signs of volume overload and heart failure as well as incongruent results by the grading of MR severity by the semi-quantitative approach. 2D two-dimensional, EROA effective regurgitant orifice area, LA left atrial, LV left ventricular, LVOT LV outflow tract, LVRI LV remodelling index, LVSVeff effective LV stroke volume, LVSVtot total LV stroke volume, MR mitral regurgitation, MV mitral valve, MVRegVol regurgitant MV volume, PISA proximal isovelocity surface area, PMR primary MR, RF regurgitant fraction, RWT relative wall thickness, SMR secondary MR, VTI velocity time integral
Proposal for standards of echocardiographic timing in MR patients. The scheme illustrates a potential timeline of echocardiographic investigations during MR treatment. The upper red box presents the therapeutic aspects and strategies, the mid blue box presents the proposed time points of echocardiographic investigations—especially focusing on secondary mitral regurgitation (SMR)-, the bottom green box illustrates the diagnostic targets of the respective echocardiographic investigations. LV left ventricular, MR mitral regurgitation, OMT optimized medical treatment, TOE transoesopageal echocardiography, TTE transthoracic echocardiography
The rationale for the stepwise workflow to assess MR severity to implement the causal relationships between clinical complaints, disease progression, and echocardiographic characteristics into the “integrated approach”
Identifying a causal relationship between clinical symptoms and MR might facilitate the interpretation of echocardiographic results in MR patients. However, symptoms as well as echocardiographic findings depend on chronicity of the disease progress. Acute MR is normally linked to severe symptoms, smaller LA and LV cavities, and severe PH, whereas chronic MR is linked to mild symptoms, larger LA and LV cavities, and different secondary PH severity. Due to this pathophysiological complexity, all possible morphologic variations of LA and LV size can be observed in clinically relevant MR.
If MR is qualitatively detected by Doppler techniques—e.g., colour flow Doppler—MV morphology should help differentiating between primary MR (PMR) and secondary MR (SMR) [29]. This classification focusses on morphological defects of the MV apparatus (PMR) and on secondary MV alterations induced by underlying LV diseases. Thus, structural involvement of the MV apparatus characterizes PMR and LV dilatation and/or LV dysfunction SMR. Pathologies of the leaflets or alterations of the intricate anatomy of the MV apparatus are causes of PMR, failure of MV leaflet coaptation due to MV annulus dilatation, increased leaflet tethering, and/or papillary muscle (PM) restriction are causes of SMR [3,4,5,6, 30, 31]. Furthermore, Carpentier’s classification scheme according to leaflets mobility [32] considers functional aspects of the MV leaflets.
The pathophysiological understanding of cardiac alterations in MR requires a morphological characterization of the cardiac cavities [3,4,5,6, 16]. Both, PMR and SMR, impose a volume load on the left ventricle and the left atrium. LV dilatation increases MV tethering forces, while LV dysfunction reduces MV closing forces, both driving factors of SMR [33]. SMR resulting from predominant mitral annular dilatation is increasingly being recognized as SMR induced by atrial remodelling [34]. The volume load in chronic PMR and SMR further aggravates LV dilatation to accommodate for the MVRegVol and to maintain LVSVeff. LV function is preserved in the compensated state in PMR, but declines in a decompensated condition. In the decompensated state, MVRegVol itself is a pathophysiological driver that contributes to the disease progress with concomitant increase of LV end-diastolic pressure (LVEDP) and secondary pulmonary hypertension (PH) [35, 36]. LV ejection fraction (LVEF) overestimates LV function in MR. Forward LVEF = LVSVeff/LV end-diastolic volume (LVEDV) seems to represent more reliably LV function than global LVEF in MR [37, 38]. Hence, MR severity relative to LV remodeling has been proposed [16, 39, 40]. In consequence, LV function, LV remodelling, and global haemodynamics often differ between PMR and SMR. Thus, LV wall thickness, LV mass, LV mass index, LV diameter, LV volume, LVEF, as well as LA volume and LA volume should be measured by echocardiography to characterize LV geometry, e.g., concentric remodelling, and concentric and eccentric LV hypertrophy [41]. Relative wall thickness (RWT) and LV mass should be measured using the posterior wall. Considering clinical symptoms and chronicity of the underlying diseases in relation to the specific echocardiographic findings, an extended MR classification is proposed for PMR and SMR patients. Five subtypes can be differentiated in PMR (Table 2). Furthermore, seven subtypes can be differentiated in SMR (Table 3) with respect to symmetric LV remodelling, asynchrony of LV contraction, regional myocardial injury, asymmetric LV hypertrophy, LV stiffening, and LA remodelling [3, 5].
Thus, one target of paramount importance is to characterize cardiac remodelling due to MR effects, which implies the specific assessment of LV [43,44,45] and LA geometry by echocardiography [46]—especially in SMR patients [3, 5, 6]. Despite recent technical improvements in echocardiography and automated features to analyze LA and LV volumes and function, conventional 2D echocardiography remains the current standard and enables the assessment of relevant cardiac parameters as illustrated in Table 4. Linear internal 2D measurements of LV diameters and LV wall thickness as well as LV volume measurements by 2D planimetry are still used in clinical practice [5, 41, 47]—especially for calculation of LV mass [41]. 3D approaches for LV mass determination are preferably recommended [48]. The sphericity ratio and sphericity index, interpapillary muscle distance, the anterior–posterior and medial–lateral PM displacement, and the length between the PM bulges and the respective contralateral MV annulus should be considered for characterization of LV remodelling [3, 49,50,51]. Furthermore, LV remodelling with disease progression or reverse LV remodeling during treatment can be assessed by monitoring LV geometry [3, 51]. LA volume measurement by 2D planimetry of the maximum LA area in the 2- and 4-chamber view (2-ChV, 4-ChV) or using 3D echocardiography is preferred [48]. The progression of LA and LV volumes and reduction of LVEF during follow-up examinations are helpful to determine haemodynamically significant deterioration even in MR patients classified as clinically not severe.
The second target is the analysis of MV morphology by echocardiography. Due to the complexity of the MV apparatus, 3D image acquisition has become an indispensable tool of echocardiographic MV assessment [48, 52,53,54,55]. However, conventional 2D echocardiography enables the measurement of specific parameters characterizing pathologies of MV morphology. MV degeneration can be identified by the presence of intensified echo-densities due to thickening and calcification of the MV annulus [42]. MV prolapse is characterized by systolic displacement of a leaflet by ≥ 2 mm overriding the annular plane into the LA [3, 52]. Rupture of the primary chordae, or ultimately of a PM, causes flail of the leaflet into the LA and is usually associated with severe MR. Analysis of MV involvement in endocarditis should include size of vegetations, presence of abscesses, aneurysms, or perforations [56]. Congenital MV defects, e.g., clefts, can be uncovered in the 3D TOE, favouring definitively this modern technology [55]. MV deformation due to LV remodelling in SMR should be assessed by measurement of MV annulus, coaptation distance/gap, coaptation length/height, as well as coaptation depth and tenting height (Table 5) [3, 5, 57]. The tenting area (area between the MA and the leaflets during systole) of ≥ 2.1 cm2 is a pathologic finding due to tethering in SMR [3,4,5]. MV analysis in SMR should be completed by the assessment of the anterior/medial and posterior/posterolateral tethering angle (Table 5) [3, 5]. As pathophysiology of MR is a constant and complex interplay between initial pathology and further propagation of the disease by volume overload, coexistence between PMR and SMR can be observed and should be labeled as mixed origin.
The rationale to implement a quantitative MR assessment to characterize MR severity
The echocardiographic workflow of grading MR severity (Figs. 3, 4) starts with a semi-quantitative MR assessment and serves two goals. First, all non-severe MR should be detected, preventing unnecessary and time-consuming further evaluation. For example, when sinus rhythm is present, an a-wave dominant inflow pattern into the LV using Doppler interrogation above the MV excludes severe MR. Also, a dominant inflow during systole from the pulmonary veins into the LA cannot be observed in severe MR. Finally, a normal LA volume is not found in chronic severe MR. These and other semi-quantitative parameters, along with their strengths, limitations, and appropriateness are listed in Table 1. In-depth quantitative evaluation should be initiated in cases if MR classification remains unclear.
The quantitative approach is based on the determination of the individual RF. This parameter is included in all current recommendations [3, 5, 6]. RF relies on the determination of LVSVtot and LVSVeff. The absolute value of MVRegVol should always be interpreted with respect to LVEDV. It is obvious that the amount of MVRegVol is much more important in small hearts than in larger hearts, which can be impressively illustrated by interspecies comparisons (Fig. 6). In consequence, haemodynamic conditions can be characterized by plausible LVEDV, LVEF, and LV forward stroke volume (= LVSVeff). Determination of MVRegVol by the 2D-PISA method alone was associated with significant overestimation of MRRegVol as documented in recent transcatheter MV repair (TMVR) trials [10, 58, 59] and further MR outcome trials [60].
Illustration of the interspecies differences of regurgitant volume in relation to total stroke volume (LVSVtot). The normal LVSVtot of a rat heart is about 0.5 ml [61] resulting in a regurgitant fraction (RF) of 50% if regurgitant volume at the mitral valve (MVRegVol) is about 0.25 ml. The normal LVSVtot of an elephant heart is about 20 l [62] resulting in a RF of about zero, if MVRegVol is about 0.25 ml. An RF of about 50% needs an MVRegVol of about 5 l
Calculation of RF is based on the measurement of LVEDV and LV endsystolic volume (LVESV) as well as LVSVeff and MVRegVol to estimate cardiac output (CO) and cardiac index (CI) by echocardiography. Practical tips to avoid pitfalls when determining cardiac volumes—especially LVSVtot, LVSVeff, and right-ventricular (RV) stroke volume (RVSVeff), are listed in Table 6. The practical approach to check Doppler measurements of RVSVeff by a plausibility cross-check is illustrated in Fig. 7. However, this concept is still not validated by prognostic data [2, 3, 5]. Compared to cardiac magnetic resonance (CMR) tomography, a significant underestimation of LV volumes by echocardiography has been reported [63]. Furthermore, over- and underestimation of LV volumes in humans [64] and phantoms [65, 66] have been described comparing different imaging methods, e.g., native 2D- and 3D echocardiography, contrast echocardiography, CMR, and computed tomography. Recently, conclusive LV volume assessment by 2D echocardiography was illustrated if image quality is adequate [67,68,69,70]. The differences in LV volumes between 2D echocardiography and CMR can be minimized by triplane, 3D-, and contrast echocardiography [71, 72]. A Doppler echocardiographic approach to calculate LVSVtot by the LV filling volume has been proposed in recent recommendations using MV diameter in the 4-chamber view and the transmitral velocity time integral (VTI) at the level of the mitral annulus [2, 3, 5]. However, this approach seems to be error-prone due to the non-circular shape of the MV annulus.
Illustration of practical aspects of LVSVeff or RVSVeff determination. Labeling of the DLVOT and correct positioning of the pw-sample volume documented by the cusp artefact in the pw-Doppler spectrum with the respective results (a); three-point labeling of diameters at the level of the pulmonic valve (1) documented by the origin of the pulmonary regurgitation, at the level of the proximal pulmonic trunk (2) and at the level of the distal RVOT (3) for the respective position of the pw-Doppler sample volume (b); labeling of the DRVOT and the corresponding pw-Doppler spectrum at the RVOT (c), at the pulmonic valve (d), and at the proximal pulmonic trunk (e) with the respective results. All determined forward stroke volumes are within similar ranges, hence documenting plausible results
LVSVeff in “pure” MR can be determined by Doppler calculations using cross-sectional area (CSA) or diameters of the LV outflow tract (LVOT) and the corresponding pulsed wave (pw) Doppler velocity time integral (VTI) [2, 3, 5]. In patients with combined aortic valve disease, LVSVeff assessment is more complex, because Doppler calculations of LVSVeff should be performed using the CSA or diameter of the RV outflow tract (RVOT) and the respective pw-Doppler VTI to assess RVSVeff, which corresponds to LVSVeff, if no or only mild pulmonary regurgitation is present. However, RVSVeff measurement is challenging due to the variable anatomy of the RVOT and the additional time needed for precise measurements.
The problem of incongruent haemodynamic measurements in MR patients is highlighted by the recently introduced terms “proportionate” and “disproportionate” MR [40, 73,74,75]. The concept of proportionality between blood flow and orifice areas can be illustrated by the continuity equation determining effective orifice area in patients with aortic valve stenosis (AS) [36, 76]. The same principle of proportionality can only theoretically be applied to the calculation of the MVRegVol (Fig. 8), because MVRegVol cannot be practically measured by pw-Doppler techniques due to methodological limitations. However, a plausibility cross-check of LVSVtot, LVSVeff, MVRegVol,CO, and CI can be performed independently of the method used for determination of these parameters, because proportionality is a prerequisite between EROA and MVRegVol. The usage of the continuity equation for MVRegVol determination is impossible due to the high transmitral velocities of regurgitant flow at the level of the mitral annulus, the EROA changes of the valve during the systolic time interval, and the deceleration of flow velocities between EROA and the mitral annulus level. Because of the rheological need of proportionality between EROA and retrograde volume flow or flow velocities, the term “disproportionateness” [40, 73,74,75] can only be interpreted as a characterization of SMR severity in relation to the impaired LV function. However, the potential therapeutical benefit of MR treatment in relation to heart failure cannot be described by the disproportionality between LVEDV and EROA, because these parameters are proportionally interrelated at a defined LVEF (Fig. 9).
Illustration of the proportionality of forward blood flow volume or effective left-ventricular stroke volume (LVSVeff) and of transmitral regurgitant volume (MVRegVol) between the respective cross-section areas (CSAs) and blood flow velocities in a system of communicating tubes. Considering the volume flow during one heart cycle total left-ventricular stroke volume (LVSVtot) is the summation of LVSVeff and MVRegVol. LVSVeff at the level of the left-ventricular outflow tract (LVOT) is equal to the level of the aortic valve (AV) orifice according to the continuity equation. By analogy MVRegVol at the level of the effective regurgitant orifice area (EROA) is equal to MVRegVol at the level of mitral valve (MV) annulus. Thus, both LVSVeff and MVRegVol exhibit proportionality between respective cross-section areas (CSA) and velocity time integrals (VTI). CSAAV CSA of the AV orifice, CSAEROA CSA of the MV regurgitant orifice, CSALVOT CSA of the LVOT, CSAMV CSA at the level of the MV annulus, DAV diameter of the AV orifice, DEROA diameter of the MV regurgitant orifice, DLVOT diameter of the LVOT, DMV diameter at the level of the MV annulus, VTIAV VTI of the systolic forward blood flow through the AV orifice, VTIEROA VTI of the diastolic backward blood flow through the MV regurgitant orifice, VTILVOT VTI of the systolic forward blood flow through the LVOT, VTIMV VTI of the diastolic forward mitral flow at the level of the MV annulus, VTI-MVRegVol VTI of the systolic regurgitant transmitral blood flow at the level of the MV annulus
The relation between LVSVtot, which is equal to LVSVeff in the absence of mitral regurgitation (MR) and aortic regurgitation (AR), and left-ventricular end-diastolic volume (LVEDV) with respect to left ejection fraction (LVEF) If LVEDV of 200 ml in the presence of LVEF of 30% is assumed at stable haemodynamic conditions labeled by the blue area ( LVSVtot = LVSVeff, = 60 ml indicating a cardiac index > 2.2 l/min m2 at a normal heart rate of 65/min), LVSVtot must be equal to LVSVeff, indicating the absence of MR and AR to provide the necessary cardiac output or cardiac index. The red arrows display the necessary increase of LVEDV or LVEF assuming severe MR with a regurgitant fraction of 50%. Thus, to provide LVSVeff of 60 ml and MVRegVol of 60 ml, LVSVtot of 120 ml is necessary. Consequently, LVEDV must be 400 ml if LVEF is 30%, and LVEF must be 60% if LVEDV is 200 ml
MR severity can be assessed as mild or moderate in heart failure patients at rest during compensated stage with OMT. However, this MR characterization at rest might not describe the individual risk of re-decompensation. Thus, in these cases, haemodynamic impairment should predominantly be documented by increase in SMR severity during mild-to-moderate dynamic stress testing to support this hypothesis [77, 78]. Early treatment of SMR is comprehensible during these conditions because of the potential for reverse LV remodeling and prevention of further deterioration of LV function, which should be documented by prospective trials.
Summary and conclusion
The analysis of MR severity has become more and more important with respect to therapeutic options for MR treatment. The grading of MR severity by “eyeballing” and the 2D-PISA method is common in clinical practice, but it often leads to incongruent results with a high inter-observer variability. In addition, the dynamics of MR due to volume conditions, heart rhythm, and respective medical treatment require a high level of standardization in echocardiography. However, echocardiography allows for reliable assessment of LVSVtot, LVSVeff, MVRegVol, and RF in MR patients. Prerequisites are verifiable documentations, respective technical skill, and plausible measurements. The present proposal provides a “new” haemodynamically oriented workflow, which integrates a detailed MR classification scheme, considering the clinical complaints, the chronicity of the disease process, the MV morphology, and the echocardiographic parameters characterizing LA and LV remodelling. The essential point to note is the integration of a quantitative assessment of MR severity into the recent “integrated approach” to provide haemodynamic plausibility and to avoid inconsistencies of echocardiographic measurements.
References
Wang A, Grayburn P, Foster JA, McCulloch ML, Badhwar V, Gammie JS, Costa SP, Benitez RM, Rinaldi MJ, Thourani VH, Martin RP (2016) Practice gaps in the care of mitral valve regurgitation: insights from the American College of Cardiology mitral regurgitation gap analysis and advisory panel. Am Heart J 172(2):70–79. https://doi.org/10.1016/j.ahj.2015.11.003
Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, Hagendorff A, Monin JL, Badano L, Zamorano JL, European Association of Echocardiography (2010) European Association of Echocardiography recommendations for the assessment of valvular regurgitation Part 1 aortic and pulmonary regurgitation (native valve disease). Eur J Echocardiogr 11(3):223–244. https://doi.org/10.1093/ejechocard/jeq030
Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA, Badano L, Zamorano JL, Scientific Document Committee of the European Association of Cardiovascular Imaging (2013) Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 14(7):611–644. https://doi.org/10.1093/ehjci/jet105
Nickenig G, Mohr FM, Kelm M, Kuck KH, Boekstegers HJ, Schillinger W, Brachmann J, Lange R, Reichenspurner H (2013) Konsensus der Deutschen Gesellschaft für Kardiologie—Herz- und Kreislaufforschung und der Deutschen Gesellschaft für Thorax-Herz- und Gefäßchirurgie zur Behandlung der Mitralklappeninsuffizienz. Kardiologe 7:76–90. https://doi.org/10.1007/s12181-013-0488-1
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, Hahn RT, Han Y, Hung J, Lang RM, Little SH, Shah DJ, Shernan S, Thavendiranathan P, Thomas JD, Weissman NJ (2017) Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J Am Soc Echocardiogr 30(4):303–371. https://doi.org/10.1016/j.echo.2017.01.007
Bonow RO, O’Gara PT, Adams DH, Badhwar V, Bavaria JE, Elmariah S, Hung JW, Lindenfeld J, Morris AA, Satpathy R, Whisenant B, Woo YJ (2020) 2020 focused update of the 2017 ACC expert consensus decision pathway on the management of mitral regurgitation: a report of the American College of Cardiology solution set oversight committee. J Am Coll Cardiol 75(17):2236–2270. https://doi.org/10.1016/j.jacc.2020.02.005
Hagendorff A, Fehske W, Flachskampf FA, Helfen A, Kreidel F, Kruck S, La Rosée K, Tiemann K, Voigt JU, von Bardeleben RS, Ralf Zahn R, Fabian Knebel F (2020) Manual zur Indikation und Durchführung der Echokardiographie—update 2020 der Deutschen Gesellschaft für Kardiologie. Kardiologe 14:396–431. https://doi.org/10.1007/s12181-020-00402-3
Stone GW, Vahanian AS, Adams DH, Abraham WT, Borer JS, Bax JJ, Schofer J, Cutlip DE, Krucoff MW, Blackstone EH, Généreux P, Mack MJ, Siegel RJ, Grayburn PA, Enriquez-Sarano M, Lancellotti P, Filippatos G, Kappetein AP (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 1: clinical trial design principles: a consensus document from the mitral valve academic research consortium. J Am Coll Cardiol 66(3):278–307. https://doi.org/10.1016/j.jacc.2015.05.046
Stone GW, Adams DH, Abraham WT, Kappetein AP, Généreux P, Vranckx P, Mehran R, Kuck KH, Leon MB, Piazza N, Head SJ, Filippatos G, Vahanian AS (2015) Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: Part 2: endpoint definitions: a consensus document from the mitral valve academic research consortium. J Am Coll Cardiol 66(3):308–321. https://doi.org/10.1016/j.jacc.2015.05.049
Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, Whisenant B, Grayburn PA, Rinaldi M, Kapadia SR, Rajagopal V, Sarembock IJ, Brieke A, Marx SO, Cohen DJ, Weissman NJ, Mack MJ, Investigators COAPT (2018) Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med 379(24):2307–2318. https://doi.org/10.1056/NEJMoa1806640
Asch AF, Grayburn PA, Siegel RJ, Kar S, Lim DS, Zaroff JG, Mishell JM, Whisenant B, Mack MJ, JoAnn Lindenfeld JA, Abraham WT, Stone GW, Weissman NJ (2019) Echocardiographic outcomes after transcatheter leaflet approximation in patients with secondary mitral regurgitation: the COAPT trial. J Am Coll Cardiol. 74(24):2969–2979. https://doi.org/10.1016/j.jacc.2019.09.017
Recusani F, Bargiggia GS, Yoganathan AP, Raisaro A, Valdes-Cruz LM, Sung HW, Bertucci C, Gallati M, Moises VA, Simpson IA, Tronconi L, Sahn DJ (1991) A new method for quantification of regurgitant flow rate using color Doppler flow imaging of the flow convergence region proximal to a discrete orifice. An in vitro study. Circulation 83(2):594–604. https://doi.org/10.1161/01.cir.83.2.594
Grayburn PA, Weissman NJ, Zamorano JL (2012) Quantitation of mitral regurgitation. Circulation 126(16):2005–2017. https://doi.org/10.1161/CIRCULATIONAHA.112.121590
Simpson IA, Shiota T, Gharib M, Sahn DJ (1996) Current status of flow convergence for clinical applications: is it a leaning tower of “PISA”? J Am Coll Cardiol 27(2):504–509. https://doi.org/10.1016/0735-1097(95)00486-6
Yosefy C, Levine RA, Solis J, Vaturi M, Handschumacher MD, Hung J (2007) Proximal flow convergence region as assessed by real-time 3-dimensional echocardiography: challenging the hemispheric assumption. J Am Soc Echocardiogr 20(4):389–396. https://doi.org/10.1016/j.echo.2006.09.006
Grayburn PA, Carabello B, Hung J, Gillam LD, Liang D, Mack MJ, McCarthy PM, Miller DC, Trento A, Siegel RJ (2014) Defining “severe” secondary mitral regurgitation: emphasizing an integrated approach. J Am Coll Cardiol 64(25):2792–2801. https://doi.org/10.1016/j.jacc.2014.10.016
Quéré JP, Tribouilloy C, Enriquez-Sarano M (2003) Vena contract measurement: theoretic basis and usefulness in the assessment of valvular regurgitation severity. Curr Cardiol Rep 5(2):110–115. https://doi.org/10.1007/s11886-003-0077-1
Biner S, Rafique A, Rafii F, Tolstrup K, Noorani O, Shiota T, Gurudevan S, Siegel RJ (2010) Reproducibility of proximal isovelocity surface area, vena contracta, and regurgitant jet area for assessment of mitral regurgitation severity. JACC Cardiovasc Imaging 3(3):235–243. https://doi.org/10.1016/j.jcmg.2009.09.029
Uretsky S, Aldaia L, Marcoff L, Koulogiannis K, Argulian E, Lasam G, Gillam L (2020) Concordance and discordance of echocardiographic parameters recommended for assessing the severity of mitral regurgitation. Circ Cardiovasc Imaging 13(5):e010278. https://doi.org/10.1161/CIRCIMAGING.119.010278 (Epub 2020)
Schwammenthal E, Chen C, Benning F, Block M, Breithardt G, Levine RA (1994) Dynamics of mitral regurgitant flow and orifice area. Physiologic application of the proximal flow convergence method: clinical data and experimental testing. Circulation 90(1):307–322. https://doi.org/10.1161/01.cir.90.1.307
Hung J, Otsuji Y, Handschumacher MD, Schwammenthal E, Levine RA (1999) Mechanism of dynamic regurgitant orifice area variation in functional mitral regurgitation: physiologic insights from the proximal flow convergence technique. J Am Coll Cardiol 33(2):538–545. https://doi.org/10.1016/s0735-1097(98)00570-1
Buck T, Plicht B, Kahlert P, Schenk IM, Hunold P, Erbel R (2008) Effect of dynamic flow rate and orifice area on mitral regurgitant stroke volume quantification using the proximal isovelocity surface area method. J Am Coll Cardiol 52(9):767–778. https://doi.org/10.1016/j.jacc.2008.05.028
Watanabe N (2019) Acute mitral regurgitation. Heart 105(9):671–677. https://doi.org/10.1136/heartjnl-2018-313373
Altiok E, Hamada S, van Hall S, Hanenberg M, Dohmen G, Almalla M, Grabskaya E, Becker M, Marx N, Hoffmann R (2011) Comparison of direct planimetry of mitral valve regurgitation orifice area by three-dimensional transesophageal echocardiography to effective regurgitant orifice area obtained by proximal flow convergence method and vena contracta area determined by color Doppler echocardiography. Am J Cardiol 107(3):452–458. https://doi.org/10.1016/j.amjcard.2010.09.043
Chandra S, Salgo IS, Sugeng L, Weinert L, Settlemier SH, Mor-Avi V, Lang RM (2011) A three-dimensional insight into the complexity of flow convergence in mitral regurgitation: adjunctive benefit of anatomic regurgitant orifice area. Am J Physiol Heart Circ Physiol 301(3):H1015–H1024. https://doi.org/10.1152/ajpheart.00275.2011
Zeng X, Levine RA, Hua L, Morris EL, Kang Y, Flaherty M, Morgan NV, Hung J (2011) Diagnostic value of vena contracta area in the quantification of mitral regurgitation severity by color Doppler 3D echocardiography. Circ Cardiovasc Imaging 4(5):506–513. https://doi.org/10.1161/CIRCIMAGING.110.961649
Enriquez-Sarano M, Dujardin KS, Tribouilloy CM, Seward JB, Yoganathan AP, Bailey KR, Tajik AJ (1999) Determinants of pulmonary venous flow reversal in mitral regurgitation and its usefulness in determining the severity of regurgitation. Am J Cardiol 83(4):535–541. https://doi.org/10.1016/s0002-9149(98)00909-6
Tribouilloy C, Shen WF, Rey JL, Adam MC, Lesbre JP (1994) Mitral to aortic velocity-time integral ratio. A non-geometric pulsed-Doppler regurgitant index in isolated pure mitral regurgitation. Eur Heart J 15(10):1335–1339. https://doi.org/10.1093/oxfordjournals.eurheartj.a060390
Carabello BA (2008) The current therapy for mitral regurgitation. J Am Coll Cardiol 52(5):319–326. https://doi.org/10.1016/j.jacc.2008.02.084
Bennett S, Thamman R, Griffiths T, Oxley C, Khan JN, Phan T, Patwala A, Heatlie G, Kwok CS (2019) Mitral annular disjunction: a systematic review of the literature. Echocardiography 36(8):1549–1558. https://doi.org/10.1111/echo.14437
Dziadzko V, Dziadzko M, Medina-Inojosa JR, Benfari G, Michelena HI, Crestanello JA, Maalouf J, Thapa P, Enriquez-Sarano M (2019) Causes and mechanisms of isolated mitral regurgitation in the community: clinical context and outcome. Eur Heart J 40(27):2194–2202. https://doi.org/10.1093/eurheartj/ehz314
Carpentier A (1983) Cardiac valve surgery—the “French correction.” J Thorac Cardiovasc Surg 86(3):323–337
Enriquez-Sarano M, Akins CW, Vahanian A (2009) Mitral regurgitation. Lancet 373:1382–1394. https://doi.org/10.1016/S0140-6736(09)60692-9
Deferm S, Bertrand PB, Verbrugge FH et al (2019) Atrial functional mitral regurgitation: JACC review topic of the week. J Am Coll Cardiol 73:2465–2476. https://doi.org/10.1016/j.jacc.2019.02.061
Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA (2006) Controversies in ventricular remodelling. Lancet 367:356–367. https://doi.org/10.1016/S0140-6736(06)68074-4
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Munoz DR, Rosenhek R, Sjogren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL (2017) 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 38(36):2739–2791. https://doi.org/10.1093/eurheartj/ehx391
Lavall D, Reil JC, Segura Schmitz L et al (2016) Early hemodynamic improvement after percutaneous mitral valve repair evaluated by noninvasive pressure-volume analysis. J Am Soc Echocardiogr 29:888–898. https://doi.org/10.1016/j.echo.2016.05.012
Kamperidis V, Marsan NA, Delgado V, Bax JJ (2016) Left ventricular systolic function assessment in secondary mitral regurgitation: Left ventricular ejection fraction vs. speckle tracking global longitudinal strain. Eur Heart J 37:811–816. https://doi.org/10.1093/eurheartj/ehv680
Gaasch WH, Aurigemma GP, Meyer TE (2020) An appraisal of the association of clinical outcomes with the severity of regurgitant volume relative to end-diastolic volume in patients with secondary mitral regurgitation. JAMA Cardiol 5:476–481. https://doi.org/10.1001/jamacardio.2019.5980
Packer M, Grayburn PA (2020) New evidence supporting a novel conceptual framework for distinguishing proportionate and disproportionate functional mitral regurgitation. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2019.5971
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270. https://doi.org/10.1093/ehjci/jev014
Abramowitz Y, Jilaihawi H, Chakravarty T, Mack MJ, Makkar RR (2015) Mitral annulus calcification. J Am Coll Cardiol 66(17):1934–1941. https://doi.org/10.1016/j.jacc.2015.08.872
De Castro S, Caselli S, Maron M, Pelliccia A, Cavarretta E, Maddukuri P, Cartoni D, Di Angelantonio E, Kuvin JT, Patel AR, Pandian NG (2007) Left ventricular remodelling index (LVRI) in various pathophysiological conditions: a real-time three-dimensional echocardiographic study. Heart 93(2):205–209. https://doi.org/10.1136/hrt.2006.093997
Kono T, Sabbah HN, Stein PD, Brymer JF, Khaja F (1991) Left ventricular shape as a determinant of functional mitral regurgitation in patients with severe heart failure secondary to either coronary artery disease or idiopathic dilated cardiomyopathy. Am J Cardiol 68(4):355–359. https://doi.org/10.1016/0002-9149(91)90831-5
Yiu SF, Enriquez-Sarano M, Tribouilloy C, Seward JB, Tajik AJ (2000) Determinants of the degree of functional mitral regurgitation in patients with systolic left ventricular dysfunction: a quantitative clinical study. Circulation 102(12):1400–1406. https://doi.org/10.1161/01.cir.102.12.1400
Balachandran P, Schaff HV, Lahr BD, Nguyen A, Daly RC, Maltais S, Pislaru SV, Dearani JA (2020) Preoperative left atrial volume index is associated with postoperative outcomes in mitral valve repair for chronic mitral regurgitation. J Thorac Cardiovasc Surg 160(3):661-672.e5. https://doi.org/10.1016/j.jtcvs.2019.08.040
Kou S, Caballero L, Dulgheru R, Voilliot D, De Sousa C, Kacharava G, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Gomez De Diego JJ, Hagendorff A, Henri C, Hristova K, Lopez T, Magne J, De La Morena G, Popescu BA, Penicka M, Ozyigit T, Rodrigo Carbonero JD, Salustri A, Van De Veire N, Von Bardeleben RS, Vinereanu D, Voigt JU, Zamorano JL, Donal E, Lang RM, Badano LP, Lancellotti P (2014) Echocardiographic reference ranges for normal cardiac chamber size: results from the NORRE study. Eur Heart J Cardiovasc Imaging 15(6):680–690. https://doi.org/10.1093/ehjci/jet284
Lang RM, Badano LP, Tsang W, Adams DH, Agricola E, Buck T, Faletra FF, Franke A, Hung J, de Isla LP, Kamp O, Kasprzak JD, Lancellotti P, Marwick TH, McCulloch ML, Monaghan MJ, Nihoyannopoulos P, Pandian NG, Pellikka PA, Pepi M, Roberson DA, Shernan SK, Shirali GS, Sugeng L, Ten Cate FJ, Vannan MA, Zamorano JL, Zoghbi WA (2012) EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. Eur Heart J Cardiovasc Imaging 13(1):1–46. https://doi.org/10.1093/ehjci/jer316
Magne J, Pibarot P, Dagenais F, Hachicha Z, Dumesnil JG, Senechal M (2007) Preoperative posterior leaflet angle accurately predicts outcome after restrictive mitral valve annuloplasty for ischemic mitral regurgitation. Circulation 115(6):782–791. https://doi.org/10.1161/CIRCULATIONAHA.106.649236
Gelsomino S, van Garsse L, Lucà F, Lorusso R, Cheriex E, Rao CM, Caciolli S, Vizzardi E, Crudeli E, Stefàno P, Gensini GF, Maessen J (2011) Impact of preoperative anterior leaflet tethering on the recurrence of ischemic mitral regurgitation and the lack of left ventricular reverse remodeling after restrictive annuloplasty. J Am Soc Echocardiogr 24(12):1365–1375. https://doi.org/10.1016/j.echo.2011.09.015
Shakil O, Jainandunsing JS, Ilic R, Matyal R, Mahmood F (2013) Ischemic mitral regurgitation: an intraoperative echocardiographic perspective. J Cardiothorac Vasc Anesth 27(3):573–585. https://doi.org/10.1053/j.jvca.2012.06.003
Pepi M, Tamborini G, Maltagliati A, Galli CA, Sisillo E, Salvi L, Naliato M, Porqueddu M, Parolari A, Zanobini M, Alamanni F (2006) Head-to-head comparison of two- and three-dimensional transthoracic and transesophageal echocardiography in the localization of mitral valve prolapse. J Am Coll Cardiol 48(12):2524–2530. https://doi.org/10.1016/j.jacc.2006.02.079
Thompson KA, Shiota T, Tolstrup K, Gurudevan SV, Siegel RJ (2011) Utility of three-dimensional transesophageal echocardiography in the diagnosis of valvular perforations. Am J Cardiol 107(1):100–102. https://doi.org/10.1016/j.amjcard.2010.08.051
Lee AP, Hsiung MC, Salgo IS, Fang F, Xie JM, Zhang YC, Lin QS, Looi JL, Wan S, Wong RH, Underwood MJ, Sun JP, Yin WH, Wei J, Tsai SK, Yu CM (2013) Quantitative analysis of mitral valve morphology in mitral valve prolapse with real-time 3-dimensional echocardiography: importance of annular saddle shape in the pathogenesis of mitral regurgitation. Circulation 127(7):832–841. https://doi.org/10.1161/CIRCULATIONAHA.112.118083
Narang A, Addetia K, Weinert L, Yamat M, Shah AP, Blair JE, Mor-Avi V, Lang RM (2018) Diagnosis of isolated cleft mitral valve using three-dimensional echocardioraphy. J Am Soc Echocardiogr 31(11):1161–1167. https://doi.org/10.1016/j.echo.2018.06.008
De Castro S, Cartoni D, d’Amati G, Beni S, Yao J, Fiorell M, Gallo P, Fedele F, Pandian NG (2000) Diagnostic accuracy of transthoracic and multiplane transesophageal echocardiography for valvular perforation in acute infective endocarditis: correlation with anatomic findings. Clin Infect Dis 30(5):825–826. https://doi.org/10.1086/313762
Dwivedi G, Mahadevan G, Jimenez D, Frenneaux M, Steeds RP (2014) Reference values for mitral and tricuspid annular dimensions using two-dimensional echocardiography. Echo Res Pract 1(2):43–50. https://doi.org/10.1530/ERP-14-0050
Obadia JF, Messika-Zeitoun D, Leurent G, Iung B, Bonnet G, Piriou N, Lefèvre T, Piot C, Rouleau F, Carrié D, Nejjari M, Ohlmann P, Leclercq F, Saint Etienne C, Teiger E, Leroux L, Karam N, Michel N, Gilard M, Donal E, Trochu JN, Cormier B, Armoiry X, Boutitie F, Maucort-Boulch D, Barnel C, Samson G, Guerin P, Vahanian A, Mewton N, Investigators MITRA-FR (2018) Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med 379(24):2297–2306. https://doi.org/10.1056/NEJMoa1805374
Witte KK, Lipiecki J, Siminiak T, Meredith IT, Malkin CJ, Goldberg SL, Stark MA, von Bardeleben RS, Cremer PC, Jaber WA, Celermajer DS, Kaye DM, Sievert H (2019) REDUCE FMR trial: a randomized sham-controlled study of percutaneous mitral annuloplasty in functional mitral regurgitation. JACC Heart Fail 7:945–955. https://doi.org/10.1016/j.jchf.2019.06.011
Namazi F, van der Bijl P, Fortuni F, Mertens BJA, Kamperidis V, van Wijngaarden SE, Stone GW, Narula J, Ajmone Marsan N, Vahanian A, Delgado V, Bax JJ (2020) Regurgitant volume/left ventricular end-diastolic volume ratio: prognostic value in patients with secondary mitral regurgitation. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2020.06.032
Arias T, Chen J, Fayad ZA, Fuster V, Hajjar RJ, Chemaly ER (2013) Comparison of echocardiographic measurements of left ventricular volumes to full volume magnetic resonance imaging in normal and diseased rats. J Am Soc Echocardiogr 26(8):910–918. https://doi.org/10.1016/j.echo.2013.04.016
Holt JP, Rhode EA, Kines H (1968) Ventricular volumes and body weight in mammals. Am J Physiol 215(3):704–715. https://doi.org/10.1152/ajplegacy.1968.215.3.704
Rigolli M, Anandabaskaran S, Christiansen JP, Whalley GA (2016) Bias associated with left ventricular quantification by multimodality imaging: a systematic review and meta-analysis. Open Heart 3(1):388. https://doi.org/10.1136/openhrt-2015-000388 (eCollection 2016)
Moceri P, Doyen D, Bertora D, Cerboni P, Ferrari E, Gibelin P (2012) Real time three-dimensional echocardiographic assessment of left ventricular function in heart failure patients: underestimation of left ventricular volume increases with the degree of dilatation. Echocardiography 29(8):970–977. https://doi.org/10.1111/j.1540-8175.2012.01707.x
Mårtensson M, Winter R, Cederlund K, Ripsweden J, Mir-Akbari H, Nowak J, Brodin LA (2008) Assessment of left ventricular volumes using simplified 3-D echocardiography and computed tomography—a phantom and clinical study. Cardiovasc Ultrasound. https://doi.org/10.1186/1476-7120-6-26
Aurich M, André F, Keller M, Greiner S, Hess A, Buss SJ, Katus HA, Mereles D (2014) Assessment of left ventricular volumes with echocardiography and cardiac magnetic resonance imaging: real-life evaluation of standard versus new semiautomatic methods. J Am Soc Echocardiogr 27(10):1017–1024. https://doi.org/10.1016/j.echo.2014.07.006
Hagendorff A, Doenst T, Falk V (2019) Echocardiographic assessment of functional mitral regurgitation: opening Pandora’s box? ESC Heart Fail 6(4):678–685. https://doi.org/10.1002/ehf2.12491
Hagendorff A, Knebel F, Helfen A, Stöbe S, Doenst T, Falk V (2020) Disproportionate mitral regurgitation: another myth? A critical appraisal of echocardiographic assessment of functional mitral regurgitation. Int J Cardiovasc Imaging. https://doi.org/10.1007/s10554-020-01975-6
Kamoen V, Calle S, De Buyzere M, Timmermans F (2020) Proportionate or disproportionate secondary mitral regurgitation: how to untangle the Gordian knot? Heart 106(22):1719–1725. https://doi.org/10.1136/heartjnl-2020-317040
Stöbe S, Kreyer K, Jurisch D, Pfeiffer D, Lavall D, Farese G, Laufs U, Hagendorff A (2020) Echocardiographic analysis of acute effects of percutaneous mitral annuloplasty on severity of functional mitral regurgitation. ESC Heart Fail 7(4):1645–1652. https://doi.org/10.1002/ehf2.12719
Malm S, Frigstad S, Sagberg E, Larsson H, Skjaerpe T (2004) Accurate and reproducible measurement of left ventricular volume and ejection fraction by contrast echocardiography: a comparison with magnetic resonance imaging. J Am Coll Cardiol 44(5):1030–1035. https://doi.org/10.1016/j.jacc.2004.05.068
Jenkins C, Moir S, Chan J, Rakhit D, Haluska B, Marwick TH (2009) Left ventricular volume measurement with echocardiography: a comparison of left ventricular opacification, three-dimensional echocardiography, or both wit magnetic resonance imaging. Eur Heart J 30(1):98–106. https://doi.org/10.1093/eurheartj/ehn484
Grayburn PA, Sannino A, Packer M (2019) Proportionate and disproportionate functional mitral regurgitation: a new conceptual framework that reconciles the results of the MITRA-FR and COAPT trials. JACC Cardiovasc Imaging 12(2):353–362. https://doi.org/10.1016/j.jcmg.2018.11.006
Hahn RT (2020) Disproportionate emphasis on proportionate mitral regurgitation-are there better measures of regurgitant severity? JAMA Cardiol. https://doi.org/10.1001/jamacardio.2019.6235
Packer M (2020) Disproportionate functional mitral regurgitation: a new therapeutic target in patients with heart failure and a reduced ejection fraction. Eur J Heart Fail 22(1):23–25. https://doi.org/10.1002/ejhf.1469
Hagendorff A, Knebel F, Helfen A, Knierim J, Sinning C, Stöbe S, Fehske W, Ewen S (2020) Expert consensus document on the assessment of the severity of aortic valve stenosis by echocardiography to provide diagnostic conclusiveness by standardized verifiable documentation. Clin Res Cardiol 109(3):271–288. https://doi.org/10.1007/s00392-019-01539-2
Izumo M, Lancellotti P, Suzuki K, Kou S, Shimozato T, Hayashi A, Akashi YJ, Osada N, Omiya K, Nobuoka S, Ohtaki E, Miyake F (2009) Three-dimensional echocardiographic assessments of exercise-induced changes in left ventricular shape and dyssynchrony in patients with dynamic functional mitral regurgitation. Eur J Echocardiogr 10(8):961–967. https://doi.org/10.1093/ejechocard/jep114
Bertrand PB, Schwammenthal E, Levine RA, Vandervoort PM (2017) Exercise dynamics in secondary mitral regurgitation: pathophysiology and therapeutic implications. Circulation 135(3):297–314. https://doi.org/10.1161/CIRCULATIONAHA.116.025260
Acknowledgements
The pencil drawings of Fig. 6 are performed by Louise Hagendorff. Louise Hagendorff has given consent to publish the drawings.
Funding
Open Access funding enabled and organized by Projekt DEAL.. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Appendix: Conference discussion
Appendix: Conference discussion
Prof. Dr. Andreas Hagendorff (Leipzig) The “2. Mitteldeutscher Echokardiographie Kongress” in Leipzig had the thematic priority about echocardiography in MR patients at the debate “echocardiography-guided clinical trials: TMVR trials and their consequences” and the session “quantification of MR severity: a problem—which cannot or can be solved”. Due to the corona crisis, we had to communicate mostly in T-conferences during the year 2020. Thus, this year, the discussion about the topic of our expert proposal was also web-based like the congress itself in October 2020. To introduce into the following conference discussion: Please, tell us the most frequent errors assessing MR severity using the “integrative approach”?
Prof. Dr. Fabian Knebel (Berlin) The most frequent error in the assessment of MR severity is the misuse of the MR jet area and its relation to the LA size. This approach is in principle inappropriate, because misinterpretation is inevitable. Further frequent errors are the use of improper images for MR assessment anyway, and the overuse of the 2D-PISA method for all MR types irrespectively to the eccentricity of the jet formation. Several simple questions can help to scrutinize the results and to uncover misinterpretations, e.g., is a relevant chronic MR possible, if the patient has no complaints?—Is a relevant MR possible in a patient with a normal LV function, if E-wave velocity is low or A-wave velocity is high?—Is a relevant MR possible if E/E` and sPAP are normal?
Prof. Dr. Andreas Hagendorff (Leipzig) The 2D-PISA method is highly prone to errors. However, do you think the 2D-PISA method can be accepted as a reasonable approach under certain conditions? Will 3D-PISA measurements will improve the assessment of MR severity?
Dr. Jan Knierim (Berlin) Notably, only the elliptical shape of the orifice area is often mentioned as a reason for underestimation of EROA and MRRegVol by the 2D-PISA-method. The multiple other factors for overestimating EROA and MRRegVol, e.g., improper labeling of the PISA radius, PISA elongation by constrained flow field and eccentric jets, dynamic nature of the MR, etc. are rarely mentioned. However, the 2D-PISA method is quite reasonable in cases of circular EROA shape and flat PISA hemispheres like in SMR Carpentier type I patients with reduced LV function and central regurgitant jet formation. 3D-PISA is a very promising tool and will obviously solve several problems of the 2D-PISA-method. Unfortunately, it is still too time-consuming at present in daily routine.
Prof. Dr. Andreas Hagendorff (Leipzig) Focusing on methodological problems by echocardiography to assess MR severity, should we provide the machine settings—especially for color Doppler images—in routine practice and/or in scientific papers due to better transparency of a verifiable documentation?
Dr. Andreas Helfen (Lünen) Considering the methodical aspects of spectral and color Doppler data acquisition, it is desirable that even in clinical practice, ultrasound settings are provided to allow insights into the quality of Doppler measurements when therapeutic options for MR patients are discussed in the heart team. Furthermore, disease progression or improvement, e.g., due to reverse LV remodeling, can be better detected comparing images with the same settings during follow-up visits. In scientific papers, the information about the machine settings should be recommended as mandatory. A second important methodological problem is linked to the measurement of the 2D-PISA radius. Although it is stated that the radius of the proximal flow convergence has to be measured “from the point of the color aliasing to the VC” [5], all studies cited in this recommendation measured the radius from the point of color aliasing to the level of the regurgitant orifice.
Prof. Dr. Andreas Hagendorff (Leipzig) Do you want to propose some ideas to provide better transparency of the echocardiographic documentation of MR by color Doppler?
Dr. Stephan Stöbe (Leipzig) This is almost an unfair question, because it gives the impression to impose requirements on routine echocardiography. However, especially in the scientific arena, we should aim for a higher standard. Thus, it would be desirable to illustrate—e.g., if a 2D-PISA-measurement is performed—the correlation of color-coded images to the cardiac cycle by a proper ECG documentation, to present an anatomical colored M-Mode to verify the optimal alignment of central jet formation within the cardiac cycle, to perform an adjustment of color-coded Doppler settings by comparison of the color delineation at the LVOT during systole in comparison to LV wall, and to prove the sample volume position and the cursor alignment of PW and CW Doppler spectra using duplex mode. All these documentations could be transparently displayed by image libraries in scientific papers as supplementals.
Prof. Dr. Andreas Hagendorff (Leipzig) Comparable to the previous question, how to improve the MR analysis with respect to the time-dependency within the cardiac cycle?
Prof. Dr. Dariusch Haghi (Ludwigshafen) As mentioned in the paper, dynamic MR time-dependency can conventionally be documented by colour-coded anatomical M-Mode showing alterations in PISA radii during systole. Perhaps 3D-colour-coded echocardiography will improve MR analysis with respect to its time-dependency within the cardiac cycle.
Prof. Dr. Andreas Hagendorff (Leipzig) Beside the time-dependency of MR within the cardiac cycle, the dynamic nature of MR during various conditions—especially in SMR—should be considered in our therapeutic decision-making. Can you recommend a strategy to clarify the importance of SMR in patients, in whom the grading of MR severity at baseline cannot explain the severity of complaints?
Dr. Nicolas Merke (Berlin) It is important to prove that the clinical symptoms are originated from the MR. Especially in SMR, which is characterized by the diseased left ventricle, mild-to-moderate dynamic stress will increase the MR degree. Thus, dynamic stress echocardiography seems to be the adequate method to document the risk of LV failure due to SMR.
Prof. Dr. Andreas Hagendorff (Leipzig) The assessment of MR severity should be performed at compensated conditions during optimized treatment (revascularization, resynchronization, and OMT). How to document this prerequisite—especially in clinical trials?
Dr. Nicolas Merke (Berlin) The information about medication and dosages like circulatory parameters may be added to the report to ensure comparability of echocardiographic findings during OMT.
Prof. Dr. Andreas Hagendorff (Leipzig) The grading of MR severity during OMT arises the question about the volume state during echocardiography. What is the “physiological” volume load?
Dr. Roland Brandt (Bad Nauheim) The “physiological” volume load is definitively not the condition in the theatre, because normally the patient is in an almost hypovolemic state prior to invasive diagnostics or intervention. In addition, general anesthesia and positive-pressure ventilation cause a reduction in sympathetic tone and have an unloading effect on the left ventricle. Therefore, TOE under general anesthesia may underestimate the degree of MR compared to the baseline evaluation in the ambulatory setting. The so-called “physiological” volume should reflect real-life conditions. Thus, we propose the echocardiographic analysis 1 day prior to intervention or surgery and at hospital discharge at comparable cardiovascular conditions for objective documentation of treatment effects.
Prof. Dr. Andreas Hagendorff (Leipzig) With respect to possible dehydration, is it allowed to assess MR severity by inducing volume overload?
Dr. Nicolas Merke (Berlin) It is certainly allowed to test intraoperatively MR severity by increasing volume load. On the other hand, the volume amount to adjust a “normal” state in the catheter laboratory is not known. Thus, provoking increased MR severity by volume load or drug-induced increase of LV afterload is crucial. The better way to test the dynamics of MR severity—as mentioned before—is a dynamic stress test. Even if the semi-quantitative and quantitative parameters are difficult to assess during dynamic stress echocardiography, the pathological increase of E/E´ and sPAP can often be determined during stress and will be helpful for decision-making.
Prof. Dr. Andreas Hagendorff (Leipzig) The characterization of MR pathology is based on the Carpentier classification and the differentiation between PMR and SMR. Are there further aspects to classify MR with respect to potential MR treatment?
Dr. Daniel Lavall (Leipzig) The Carpentier classification and the differentiation between PMR and SMR are crucial for medical, surgical, and interventional therapy as well as for prognostic considerations. However, multiple aspects—the MR etiology, the MR chronicity, concomitant diseases, clinical complaints, and special echocardiographic findings—may also be considered in a classification to specify more in detail the underlying MR mechanisms. We assume that the proposed classification aligned to echocardiographic and clinical characteristics might be helpful to guide therapeutic approaches.
Prof. Dr. Andreas Hagendorff (Leipzig) How to define the morphological differences between fibroelastic deficiency, Barlow`s disease and MV annulus disjunction?
Dr. Tobias Ruf (Mainz) Fibroelastic deficiency is characterized by thin MV leaflet, MV prolapse—frequently in a single scallop—and frequent chordae rupture, whereas Barlow`s disease shows bulky billowing leaflets with excess of tissue, thick MV leaflets and multi-segmental prolapse. However, the echocardiographic characterization is challenging. In contrast the MV annulus disjunction is a sole echocardiographic diagnosis showing insertion of the MV leaflets at the LA level and a curling motion of the LV wall during systole predominantly in the posterolateral LV segments.
Prof. Dr. Andreas Hagendorff (Leipzig) Again, focusing on MV morphology do you think that 3D echocardiography is mandatory for better diagnosis of leaflet perforation or clefts?
PD Dr. Ertunc Altiok (Aachen) The answer is easy—“yes”. 3D TTE and 3D TOE allow improved en-face visualizing of MV leaflets permitting more precise localization of pathologies and the origin of regurgitation jets compared to 2D echocardiography. However, it should be noted that 3D TOE imaging can be limited particularly by dropout artefacts giving the appearance of not existing valve perforation or cleft. This limitation may be overcome by visualization of the defect in more than one view and by demonstration of color Doppler flow through the valve at the site of the suspected perforation or cleft.
Prof. Dr. Andreas Hagendorff (Leipzig) Looking at the individual RF as an objective individual parameter of MR severity—is this quantitative approach a solution to provide conclusive echocardiographic results?
PD Dr. Sebastian Ewen The accurate quantification of MR severity by the individual RF would be the desirable “gold standard” of MR assessment. However, this approach is the most difficult one and requires maximum accurateness of echocardiographic image acquisition and high expertise of measurement procedures. Thus, the quantitative RF determination is comparably error-prone as the “integrated approach” of the current recommendations [3, 5] in untrained echocardiography. The verification of cardiac volumes determined by Doppler techniques or planimetry/volumetry—especially the comparison of LVSVtot, LVSVeff, and MRRegVol in MR patients—is necessary to provide haemodynamic plausibility and to avoid miscalculation of MR severity.
Prof. Dr. Andreas Hagendorff (Leipzig) The quantitative approach of MR assessment is still a maximum challenge. Do you think this approach can be implemented into the so-called clinical routine?
Prof. Dr. Fabian Knebel (Berlin) My answer will disappoint you. The determination of the individual RF is nothing for routine scanning procedures. In addition, we need a complete rethinking in echocardiography regarding the possibilities and options of accurate LV and RV volume assessment by all possible echocardiographic techniques to accept this quantitative approach. However, if AS patients are classified according to flow conditions determined by Doppler echocardiography. Perhaps, it is possible to determine LVSVeff in MR patients, and thus, the estimation of CO and CI might be the first step to characterize the cardiovascular conditions in MR patients. Currently, the quantitative approach of RF determination is only feasible for experts.
However, to finalize our discussion, what is the most important challenge to improve the quality of echocardiography for assessment of MR severity?
Prof. Dr. Andreas Hagendorff (Leipzig) The answer is simple. We need to improve echocardiographic teaching as concerns basic knowledge of physics, anatomy and pathophysiology, technical skill of the scanning, image optimization, standardization and completeness of documentation, clinical experience, interpretation of the findings, and knowledge about possible treatment options. I think, we have still to cover these educational challenges—even in the near era of artificial intelligence.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hagendorff, A., Knebel, F., Helfen, A. et al. Echocardiographic assessment of mitral regurgitation: discussion of practical and methodologic aspects of severity quantification to improve diagnostic conclusiveness. Clin Res Cardiol 110, 1704–1733 (2021). https://doi.org/10.1007/s00392-021-01841-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01841-y