Abstract
Background
For patients with heart failure (HF), iron deficiency (ID) is a common therapeutic target. However, little is known about the utility of transferrin saturation (TSAT) or serum ferritin for risk stratification in decompensated HF (DHF) or the European Society of Cardiology's (ESC) current definition of ID (ferritin < 100 μg/L or TSAT < 20% if ferritin is 100–299 μg/L). We evaluated the association between these potential markers of ID and the risk of 30-day readmission for HF or death in patients with DHF.
Methods
We retrospectively included 1701 patients from a multicenter registry of DHF. Serum ferritin and TSAT were evaluated 24–72 h after hospital admission, and multivariable Cox regression was used to assess their association with the composite endpoint.
Results
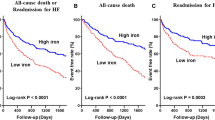
Participants' median (quartiles) age was 76 (68–82) years, 43.8% were women, and 51.7% had a left ventricular ejection fraction > 50%. Medians for NT-proBNP, TSAT, and ferritin were 4067 pg/mL (1900–8764), 14.1% (9.0–20.3), and 103 ug/L (54–202), respectively. According to the current ESC definition, 1,246 (73.3%) patients had ID. By day 30, there were 177 (10.4%) events (95 deaths and 85 HF readmission). After multivariable adjustment, lower TSAT was associated with outcome (p = 0.009) but serum ferritin was not (HR 1.00; 95% confidence interval 0.99–1.00, p = 0.347).
Conclusions
Lower TSAT, but not ferritin, was associated with a higher risk of short-term events in patients with DHF. Further research is needed to confirm these findings and the utility of serum ferritin as a marker of ID in DHF.
Graphic abstract



Similar content being viewed by others
References
Okonko, D. O., Mandal, A. K., Missouris, C. G., & Poole-Wilson, P. A. (2011). Disordered iron homeostasis in chronic heart failure: prevalence, predictors, and relation to anemia, exercise capacity, and survival. Journal of the American College of Cardiology, 58, 1241–1251.
Cleland, J. G., Zhang, J., Pellicori, P., et al. (2016). Prevalence and outcomes of anemia and hematinic deficiencies in patients with chronic heart failure. JAMA Cardiol, 1, 539–547.
Ambrosy, A. P., Gurwitz, J. H., Tabada, G. H., et al. (2019). Incident anaemia in older adults with heart failure: rate, aetiology, and association with outcomes. Eur Heart J Qual Care Clin Outcomes, 5, 361–369.
Moliner, P., Jankowska, E. A., van Veldhuisen, D. J., et al. (2017). Clinical correlates and prognostic impact of impaired iron storage versus impaired iron transport in an international cohort of 1821 patients with chronic heart failure. International Journal of Cardiology, 243, 360–366.
Grote Beverborg, N., Klip, I. T., Meijers, W. C., et al. (2018). Definition of iron deficiency based on the gold standard of bone marrow iron staining in heart failure patients. Circulation. Heart Failure, 11, e004519.
Gentil, J. R. S., Fabricio, C. G., Tanaka, D. M., et al. (2020). Should we use ferritin in the diagnostic criteria of iron deficiency in heart failure patients? Clin Nutr ESPEN, 39, 119–123.
Anker, S. D., Comin Colet, J., Filippatos, G., et al. (2009). Ferric carboxymaltose in patients with heart failure and iron deficiency. New England Journal of Medicine, 361, 2436–2448.
Ponikowski, P., van Veldhuisen, D. J., Comin-Colet, J., et al. (2015). Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. European Heart Journal, 36, 657–668.
Anker, S. D., Kirwan, B. A., van Veldhuisen, D. J., et al. (2018). Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: an individual patient data meta-analysis. European Journal of Heart Failure, 20, 125–133.
Mistry, R., Hosoya, H., Kohut, A., & Ford, P. (2019). Iron deficiency in heart failure, an underdiagnosed and undertreated condition during hospitalization. Annals of Hematology, 98, 2293–2297.
Cohen-Solal, A., Damy, T., Terbah, M., et al. (2014). High prevalence of iron deficiency in patients with acute decompensated heart failure. European Journal of Heart Failure, 16, 984–991.
Ponikowski, P., Kirwan, B. A., Anker, S. D., et al. (2020). Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicenter, double-blind, randomized, controlled trial. Lancet, 396, 1895–1904.
Farmakis, D., Parissis, J., Lekakis, J., & Filippatos, G. (2015). Acute heart failure: epidemiology, risk factors, and prevention. Revista Espanola de Cardiologia, 68, 245–248.
Ponikowski, P., Voors, A. A., Anker, S. D., et al. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Journal of Heart Failure, 18, 891–975.
Nutritional anaemias. Report of a WHO scientific group. (1968). World Health Organ. Tech Rep Ser, 405, 5–37.
Rocha, B. M. L., Cunha, G. J. L., & MenezesFalcão, L. F. (2018). The burden of iron deficiency in heart failure: therapeutic approach. Journal of the American College of Cardiology, 71, 782–793.
Nunez, J., Comin-Colet, J., Miñana, G., et al. (2016). Iron deficiency and risk of early readmission following a hospitalization for acute heart failure. European Journal of Heart Failure, 18, 798–802.
Pasricha, S. R., Tye-Din, J., Muckenthaler, M. U., & Swinkels, D. W. (2020). Iron deficiency. Lancet. https://doi.org/10.1016/S0140-6736(20)32594-0
WHO. (2011). Serum Ferritin Concentrations for The Assessment of Iron Status and Iron Deficiency in Populations. World Health Organization, Geneva: Vitamin and Min-eral Nutrition Information System.
Silvestre, O. M., Gonçalves, A., Nadruz, W., Jr., et al. (2017). Ferritin levels and risk of heart failure-the atherosclerosis risk in communities study. European Journal of Heart Failure, 19, 340–347.
Cacoub, P., Vandewalle, C., & Peoc’h, K. (2019). Using transferrin saturation as a diagnostic criterion for iron deficiency: a systematic review. Critical Reviews in Clinical Laboratory Sciences, 56, 526–532.
Jankowska, E. A., Kasztura, M., Sokolski, M., et al. (2014). Iron deficiency defined as depleted iron stores accompanied by unmet cellular iron requirements identifies patients at the highest risk of death after an episode of acute heart failure. European Heart Journal, 35, 2468–2476.
Hirsch, V. G., Tongers, J., Bode, J., et al. (2020). Cardiac iron concentration in relation to systemic iron status and disease severity in non-ischaemic heart failure with reduced ejection fraction. European Journal of Heart Failure, 22, 2038–2046.
Núñez, J., Miñana, G., Cardells, I., et al. (2020). Noninvasive imaging estimation of myocardial iron repletion following administration of intravenous iron: the myocardial-IRON trial. J Am Heart Assoc. https://doi.org/10.1161/JAHA.119.014254
Santas, E., Miñana, G., Cardells, I., et al. (2020). Myocardial-IRON investigators. Short-term changes in left and right systolic function following ferric carboxymaltose: a substudy of the Myocardial-IRON trial. ESC Heart Fail, 7, 4222–4230.
Funding
This work was supported in part by an unrestricted grant from Vifor Pharma, CIBER Cardiovascular (Grant Numbers 16/11/00420 and 16/11/00403).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest concerning the research, authorship, and publication of this article.
Ethics standards
This work complies with ethical standards.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Palau, P., Llàcer, P., Domínguez, E. et al. Iron deficiency and short-term adverse events in patients with decompensated heart failure. Clin Res Cardiol 110, 1292–1298 (2021). https://doi.org/10.1007/s00392-021-01832-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01832-z