Abstract
Background
The bleeding risk profile of patients with atrial fibrillation (AF) may change over time, and the increment of HAS-BLED score is perceived to result in discontinuations of oral anticoagulants (OACs).
Objectives
To investigate the changes of HAS-BLED scores of AF patients initially with a low bleeding risk. The associations between continuation or discontinuation of OACs and clinical outcomes after patients’ bleeding risk profile worsened (ie HAS-BLED increased) were studied.
Methods
The present study used Taiwan nationwide health insurance research database. From year 2000 to 2015, a total of 24,990 AF patients aged ≥ 20 years with a CHA2DS2-VASc score ≥ 1 (males) or ≥ 2 (females) having an HAS-BLED score of 0–2 who were treated with OACs were identified and followed up for changes of the HAS-BLED scores. Patients who did not refill OACs within 90 days after their HAS-BLED scores increased to ≥ 3 were defined as discontinuations of OACs. The risks of clinical outcomes were compared between patients who continued or stopped OACs once their HAS-BLED scores increased to ≥ 3.
Results
Mean HAS-BLED score of study population increased from 1.54 to 3.33. At end of 1 year, 5,229 (20.9%) patients had an increment of their HAS-BLED scores to ≥ 3, mainly due to newly diagnosed hypertension, stroke, bleeding, and concomitant drug therapies. Among 4777 patients who consistently had an HAS-BLED score ≥ 3, 1,062 (22.2%) stopped their use of OACs. Patients who kept on OACs (n = 3715; 77.8%) even after their HAS-BLED scores increased to ≥ 3 were associated with a lower risk of ischemic stroke (aHR 0.60, 95%CI 0.53–0.69), major bleeding (aHR 0.78, 95%CI 0.67–0.91), all-cause mortality (aHR 0.88, 95%CI 0.79–0.97), and any adverse events (aHR 0.75, 95%CI 0.68–0.82) adjusted for age, sex, heart failure, and HAS-BLED score. These results were consistent among the cohorts after propensity matching.
Conclusions
For patients whose HAS-BLED scores increased to ≥ 3, the continuation of OACs was associated with better clinical outcomes. An increased HAS-BLED score in anticoagulated AF patients may not be the only reason to withhold OACs, but reminds physicians to correct modifiable bleeding risk factors and follow up patients more closely.
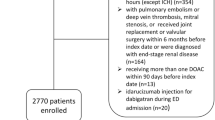
Graphical abstract
Associations between Continuation or Discontinuation of Oral Anticoagulants and Risks of Clinical Outcomes after HAS-BLED Scores Increased

AF atrial fibrillation; aHR adjusted hazard ratio; ICH intra-cranial hemorrhage; OACs oral anticoagulants






Similar content being viewed by others
References
Lip GY, Freedman B, De Caterina R, Potpara TS (2017) Stroke prevention in atrial fibrillation: past, present and future. Thromb Haemost 117(07):1230–1239
Hart RG, Pearce LA, Aguilar MI (2007) Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med 146:857–867
Lip GYH, Banerjee A, Boriani G, Chiang CE, Fargo R, Freedman B, Lane DA, Ruff CT, Turakhia M, Werring D, Patel S, Moores L (2018) Antithrombotic therapy for atrial fibrillation: chest guideline and expert panel report. Chest 154:1121–1201
Borre ED, Goode A, Raitz G, Shah B, Lowenstern A, Chatterjee R, Sharan L, Allen LaPointe NM, Yapa R, Davis JK, Lallinger K, Schmidt R, Kosinski A, Al-Khatib SM, Sanders GD (2018) Predicting thromboembolic and bleeding event risk in patients with non-valvular atrial fibrillation: a systematic review. Thromb Haemost 118:2171–2187
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138:1093–1100
Lip GY, Lane DA (2016) Bleeding risk assessment in atrial fibrillation: observations on the use and misuse of bleeding risk scores. J Thromb Haemost 14:1711–1714
Olesen JB, Lip GY, Lindhardsen J, Lane DA, Ahlehoff O, Hansen ML, Raunso J, Tolstrup JS, Hansen PR, Gislason GH, Torp-Pedersen C (2011) Risks of thromboembolism and bleeding with thromboprophylaxis in patients with atrial fibrillation: a net clinical benefit analysis using a “real world” nationwide cohort study. Thromb Haemost 106:739–749
Roldan V, Marin F, Manzano-Fernandez S, Gallego P, Vilchez JA, Valdes M, Vicente V, Lip GY (2013) The HAS-BLED score has better prediction accuracy for major bleeding than CHADS2 or CHA2DS2-VASc scores in anticoagulated patients with atrial fibrillation. J Am Coll Cardiol 62:2199–2204
Apostolakis S, Lane DA, Buller H, Lip GY (2013) Comparison of the CHADS2, CHA2DS2-VASc and HAS-BLED scores for the prediction of clinically relevant bleeding in anticoagulated patients with atrial fibrillation: the AMADEUS trial. Thromb Haemost 110:1074–1079
Domek M, Gumprecht J, Mazurek M, Chao TF, Lip GYH (2019) Should we judge stroke risk by static or dynamic risk scores? a focus on the dynamic nature of stroke and bleeding risks in patients with atrial fibrillation. J Cardiovasc Pharmacol 74:491–498
Fauchier L, Bodin A, Bisson A, Herbert J, Spiesser P, Clementy N, Babuty D, Chao TF, Lip GY (2020) Incident comorbidities, aging and the risk of stroke in 608,108 patients with atrial fibrillation: a nationwide analysis. J Clinic Med 9(4):1234
Chao TF, Lip GYH, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Chen SA (2018) Relationship of aging and incident comorbidities to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol 71:122–132
Yoon M, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, Kim JY, Pak HN, Lee MH, Lip GYH, Joung B (2018) Dynamic changes of cha2ds2-vasc score and the risk of ischaemic stroke in asian patients with atrial fibrillation: a nationwide cohort study. Thromb Haemost 118:1296–1304
Chao TF, Lip GYH, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Chen SA (2018) Incident risk factors and major bleeding in patients with atrial fibrillation treated with oral anticoagulants: a comparison of baseline, follow-up and delta has-bled scores with an approach focused on modifiable bleeding risk factors. Thromb Haemost 118:768–777
Chao TF, Liu CJ, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Lip GYH, Chen SA (2018) Oral anticoagulation in very elderly patients with atrial fibrillation: a nationwide cohort study. Circulation 138:37–47
Chao TF, Lip GYH, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Chen SA (2019) Age threshold for the use of non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with atrial fibrillation: insights into the optimal assessment of age and incident comorbidities. Eur Heart J 40:1504–1514
Chao TF, Chiang CE, Liao JN, Chen TJ, Lip GYH, Chen SA (2020) Comparing the effectiveness and safety of nonvitamin k antagonist oral anticoagulants and warfarin in elderly asian patients with atrial fibrillation: a nationwide cohort study. Chest 157:1266–1277
Chang CH, Lee YC, Tsai CT, Chang SN, Chung YH, Lin MS, Lin JW, Lai MS (2014) Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis 232:224–230
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137:263–272
Friberg L, Rosenqvist M, Lip GY (2012) Net clinical benefit of warfarin in patients with atrial fibrillation: a report from the Swedish atrial fibrillation cohort study. Circulation 125:2298–2307
Chao TF, Liu CJ, Liao JN, Wang KL, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Chung FP, Chen TJ, Lip GY, Chen SA (2016) Use of oral anticoagulants for stroke prevention in patients with atrial fibrillation who have a history of intracranial hemorrhage. Circulation 133:1540–1547
Gallego P, Roldan V, Marin F, Romera M, Valdes M, Vicente V, Lip GY (2013) Cessation of oral anticoagulation in relation to mortality and the risk of thrombotic events in patients with atrial fibrillation. Thromb Haemost 110:1189–1198
Guo Y, Lane DA, Chen Y, Lip GY, mAF-App II Trial investigators, (2020) Regular bleeding risk assessment associated with reduction in bleeding outcomes: the mAFA-II randomized trial. Am J Med 133(10):1195–1202
Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML (2011) Validation of the national health insurance research database with ischemic stroke cases in taiwan. Pharmacoepidemiol Drug Saf 20:236–242
Hsieh CY, Chen CH, Li CY, Lai ML (2015) Validating the diagnosis of acute ischemic stroke in a national health insurance claims database. J Formos Med Assoc 114:254–259
Acknowledgements
1. This work was supported in part by grants from the Ministry of Science and Technology (MOST 107-2314-B-075-062-MY3), Taipei Veterans General Hospital (V108B-015, V108B-027, V108C-090, V109C-042, and V109C-186), Research Foundation of Cardiovascular Medicine, and Szu-Yuan Research Foundation of Internal Medicine, Taipei, Taiwan.
2. This study is based on data from the Health and Welfare Data Science Center (HWDC), Ministry of Health and Welfare (MOHW), Taiwan. The interpretation and conclusions contained herein do not represent those of HWDC, MOHW, Taiwan.
Author information
Authors and Affiliations
Contributions
GYHL: Consultant for Bayer/Janssen, BMS/Pfizer, Medtronic, Boehringer Ingelheim, Novartis, Verseon and Daiichi-Sankyo. Speaker for Bayer, BMS/Pfizer, Medtronic, Boehringer Ingelheim, and Daiichi-Sankyo. No fees are directly received personally.
Corresponding author
Rights and permissions
About this article
Cite this article
Chao, TF., Chan, YH., Chiang, CE. et al. Continuation or discontinuation of oral anticoagulants after HAS-BLED scores increase in patients with atrial fibrillation. Clin Res Cardiol 111, 23–33 (2022). https://doi.org/10.1007/s00392-021-01816-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01816-z