Abstract
Background
Treatment with extracorporeal life support (ECLS) in acute myocardial infarction (AMI) complicated by cardiogenic shock (CS) fell short of improving myocardial recovery measured by 30 day ejection fraction in the ECLS-SHOCK trial. However, to date, no data regarding impact of ECLS on long-term outcomes exist.
Methods
In this randomized, controlled, prospective, open-label trial, 42 patients with CS complicating AMI were randomly assigned to ECLS (ECLS group, n = 21) or no ECLS (control group, n = 21). The primary endpoint was left ventricular ejection fraction (LVEF) after 30 days. Secondary endpoints included mortality and neurological outcome after 12 months. Evaluation of neurological outcome used the modified Rankin Scale.
Results
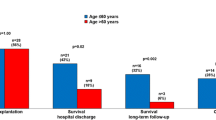
The 12-month all-cause mortality was 19% in the ECLS group versus 38% in the control group (p = 0.31). Only one patient (control group) died after the initial 30 days. Three patients underwent elective percutaneous coronary intervention (PCI) during follow-up (one in the control and two in the ECLS group). Favorable neurological outcome (modified Rankin Score ≤ 2) was seen in 61.9% of patients in the ECLS group versus 57.1% in the control group (p = 1).
Conclusion
This pilot study showed that randomized studies with ECLS in CS patients are feasible and safe. Small numbers of included patients impede meaningful conclusions about mortality and neurological outcome. Our findings of numerical differences in mortality and survival with severe neurological impairment give an urgent call for larger multi-centric randomized trials assessing the endpoint of all-cause mortality but also considering the effects on neurological outcome measures.
Graphic abstract



Similar content being viewed by others
Availability of data and material
The R Code of our analysis was submitted to the journal and is available on request.
Abbreviations
- AMI:
-
Acute myocardial infarction
- CABG:
-
Coronary artery bypass graft
- CAD:
-
Coronary artery disease
- CS:
-
Cardiogenic shock
- ECLS:
-
Extracorporeal life support
- IABP:
-
Intra-aortic balloon pumping
- IQR:
-
Interquartile range
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiac event
- PCI:
-
Percutaneous coronary intervention
- PCAS:
-
Post-cardiac arrest syndrome
- PRMD:
-
Post resuscitation myocardial dysfunction
References
van Diepen S, Katz JN, Albert NM, Henry TD, Jacobs AK, Kapur NK, Kilic A, Menon V, Ohman EM, Sweitzer NK, Thiele H, Washam JB, Cohen MG, American Heart Association Council on Clinical C, Council on C, Stroke N, Council on Quality of C, Outcomes R, Mission L (2017) Contemporary management of cardiogenic shock: a scientific statement from the American Heart Association. Circulation 136:e232–e268
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Group ESCSD (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200
Thiele H, Jobs A, Ouweneel DM, Henriques JPS, Seyfarth M, Desch S, Eitel I, Poss J, Fuernau G, de Waha S (2017) Percutaneous short-term active mechanical support devices in cardiogenic shock: a systematic review and collaborative meta-analysis of randomized trials. Eur Heart J 38:3523–3531
Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J, Richardt G, Hennersdorf M, Empen K, Fuernau G, Desch S, Eitel I, Hambrecht R, Fuhrmann J, Bohm M, Ebelt H, Schneider S, Schuler G, Werdan K, Investigators I-SIT (2012) Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med 367:1287–1296
Aubin H, Petrov G, Dalyanoglu H, Saeed D, Akhyari P, Paprotny G, Richter M, Westenfeld R, Schelzig H, Kelm M, Kindgen-Milles D, Lichtenberg A, Albert A (2016) A Suprainstitutional network for remote extracorporeal life support: a retrospective cohort study. JACC Heart Fail 4:698–708
Guenther SP, Brunner S, Born F, Fischer M, Schramm R, Pichlmaier M, Massberg S, Hagl C, Khaladj N (2016) When all else fails: extracorporeal life support in therapy-refractory cardiogenic shock. Eur J Cardiothorac Surg 49:802–809
Schmidt M, Burrell A, Roberts L, Bailey M, Sheldrake J, Rycus PT, Hodgson C, Scheinkestel C, Cooper DJ, Thiagarajan RR, Brodie D, Pellegrino V, Pilcher D (2015) Predicting survival after ECMO for refractory cardiogenic shock: the survival after veno-arterial-ECMO (SAVE)-score. Eur Heart J 36:2246–2256
Thiagarajan RR, Barbaro RP, Rycus PT, McMullan DM, Conrad SA, Fortenberry JD, Paden ML, centers Em (2017) Extracorporeal life support organization registry international report 2016. ASAIO J 63:60–67
Sattler S, Khaladj N, Zaruba MM, Fischer M, Hausleiter J, Mehilli J, Kaab S, Hagl C, Massberg S, Theiss HD (2014) Extracorporal life support (ECLS) in acute ischaemic cardiogenic shock. Int J Clin Pract 68:529–531
Kapur NK, Paruchuri V, Urbano-Morales JA, Mackey EE, Daly GH, Qiao X, Pandian N, Perides G, Karas RH (2013) Mechanically unloading the left ventricle before coronary reperfusion reduces left ventricular wall stress and myocardial infarct size. Circulation 128:328–336
Ostadal P, Mlcek M, Gorhan H, Simundic I, Strunina S, Hrachovina M, Kruger A, Vondrakova D, Janotka M, Hala P, Mates M, Ostadal M, Leiter JC, Kittnar O, Neuzil P (2018) Electrocardiogram-synchronized pulsatile extracorporeal life support preserves left ventricular function and coronary flow in a porcine model of cardiogenic shock. PLoS One 13:e0196321
Brunner S, Guenther SPW, Lackermair K, Peterss S, Orban M, Boulesteix AL, Michel S, Hausleiter J, Massberg S, Hagl C (2019) Extracorporeal life support in cardiogenic shock complicating acute myocardial infarction. J Am Coll Cardiol 73:2355–2357
Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, Nordbeck P, Geisler T, Landmesser U, Skurk C, Fach A, Lapp H, Piek JJ, Noc M, Goslar T, Felix SB, Maier LS, Stepinska J, Oldroyd K, Serpytis P, Montalescot G, Barthelemy O, Huber K, Windecker S, Savonitto S, Torremante P, Vrints C, Schneider S, Desch S, Zeymer U, Investigators C-S (2017) PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med 377:2419–2432
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P, Group ESCSD (2018) 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39:119–177
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S, Group ESCSD (2016) 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 37:267–315
Werdan K, Russ M, Buerke M, Delle-Karth G, Geppert A, Schondube FA, German Cardiac S, German Society of Intensive C, Emergency M, German Society for T, Cardiovascular S, German Interdisciplinary Association of Intensive C, Emergency M, Austrian Society of C, German Society of A, Intensive Care M, German Society of Preventive M, Rehabilitation (2012) Cardiogenic shock due to myocardial infarction: diagnosis, monitoring and treatment: a German–Austrian S3 guideline. Dtsch Arztebl Int 109:343–351
Guenther SPW, Buchholz S, Born F, Brunner S, Schramm R, Hoechter DJ, von Dossow V, Pichlmaier M, Hagl C, Khaladj N (2017) Remote ECLS-implantation and transport for retrieval of cardiogenic shock patients. Air Med J 36:320–326
Seyfarth M, Sibbing D, Bauer I, Frohlich G, Bott-Flugel L, Byrne R, Dirschinger J, Kastrati A, Schomig A (2008) A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J Am Coll Cardiol 52:1584–1588
Cha KC, Kim HI, Kim OH, Cha YS, Kim H, Lee KH, Hwang SO (2018) Echocardiographic patterns of postresuscitation myocardial dysfunction. Resuscitation 124:90–95
Kern KB, Hilwig RW, Rhee KH, Berg RA (1996) Myocardial dysfunction after resuscitation from cardiac arrest: an example of global myocardial stunning. J Am Coll Cardiol 28:232–240
Lorusso R, Barili F, Mauro MD, Gelsomino S, Parise O, Rycus PT, Maessen J, Mueller T, Muellenbach R, Belohlavek J, Peek G, Combes A, Frenckner B, Pesenti A, Thiagarajan RR (2016) In-hospital neurologic complications in adult patients undergoing Venoarterial extracorporeal membrane oxygenation: results from the extracorporeal life support organization registry. Crit Care Med 44:e964–e972
Lorusso R (2017) Extracorporeal life support and neurologic complications: still a long way to go. J Thorac Dis 9:E954–E956
Wong JK, Smith TN, Pitcher HT, Hirose H, Cavarocchi NC (2012) Cerebral and lower limb near-infrared spectroscopy in adults on extracorporeal membrane oxygenation. Artif Organs 36:659–667
Busl KM, Greer DM (2010) Hypoxic-ischemic brain injury: pathophysiology, neuropathology and mechanisms. NeuroRehabilitation 26:5–13
Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, Long J, Slowther A, Pocock H, Black JJM, Moore F, Fothergill RT, Rees N, O’Shea L, Docherty M, Gunson I, Han K, Charlton K, Finn J, Petrou S, Stallard N, Gates S, Lall R, Collaborators P (2018) A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med 379:711–721
Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, Bottiger BW, Friberg H, Sunde K, Sandroni C (2015) European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-resuscitation Care 2015: Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 95:202–222
Funding
LivaNova (Munich, Germany) supported the study, but did not have any involvement in trial design or evaluation.
Author information
Authors and Affiliations
Contributions
KL (conception and design or analysis and interpretation of data, drafting of the manuscript or revising it critically for important intellectual content), SB (conception and design or analysis and interpretation of data, drafting of the manuscript or revising it critically for important intellectual content), MO (final approval of the manuscript submitted), SP (final approval of the manuscript submitted), MO (final approval of the manuscript submitted), HDT (conception and design or analysis and interpretation of data), BCH (final approval of the manuscript submitted), GJ (final approval of the manuscript submitted), FB (conception and design or analysis and interpretation of data), A-LB (conception and design or analysis and interpretation of data), AB (conception and design or analysis and interpretation of data), MP (conception and design or analysis and interpretation of data), JH (conception and design or analysis and interpretation of data, drafting of the manuscript or revising it critically for important intellectual content), SM (conception and design or analysis and interpretation of data, drafting of the manuscript or revising it critically for important intellectual content), CH (conception and design or analysis and interpretation of data), SPWG (conception and design or analysis and interpretation of data, final approval of the manuscript submitted).
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lackermair, K., Brunner, S., Orban, M. et al. Outcome of patients treated with extracorporeal life support in cardiogenic shock complicating acute myocardial infarction: 1-year result from the ECLS-Shock study. Clin Res Cardiol 110, 1412–1420 (2021). https://doi.org/10.1007/s00392-020-01778-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01778-8