Abstract
Background
Low-flow low-gradient (LF-LG) aortic stenosis (AS) is associated with high mortality, even after transcatheter aortic valve replacement (TAVR). Further knowledge of risk indicators is needed and a clinical risk score would be desirable for optimizing patient selection and therapeutic strategy.
Methods
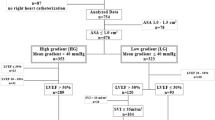
The study cohort comprised of 219 consecutive LF-LG AS patients undergoing TAVR from 2008 to 2018 in two high-volume German centers. Predictive factors for one-year all-cause mortality were defined according to a Cox proportional hazard model.
Results
At one-year follow-up after TAVR, 28% of patients had died. A multivariate model revealed six independent predictors of one-year mortality: history of myocardial infarction (HR 2.05, 95%CI 1.13–3.72), eGFR < 30 ml/min/1.73m2 (HR 2.75, 95%CI 1.48–5.11), tricuspid regurgitation moderate or more (HR 2.06, 95%CI 1.14–3.72), stroke volume index < 25 mL/m2 (HR 2.03, 95%CI 1.14–3.62), self-expandable device (HR 2.72, 95%CI 1.17–6.27), and non-transfemoral approach (HR 3.42, 95%CI 1.28–9.14). The Rhineland Risk Score (RRS) consisting of these variables (c statistic 0.75, 95%CI 0.68–0.82, p < 0.001) was superior to the EuroSCORE II (c statistic 0.63) and STS-PROM score (c statistic 0.69) at predicting one-year mortality. Patients with a RRS ≥ 8 had a prohibitive risk of one-year mortality of 67.6% (95%CI 52.0–82.4%).
Conclusion
In patients with LF-LG AS, history of myocardial infarction, renal dysfunction, tricuspid regurgitation, a low stroke volume index, self-expandable device, and non-femoral approach were associated with increased 1-year mortality after TAVR. The RRS might serve as a helpful tool for risk prediction and patient selection for TAVR in patients with LF-LG AS.




Similar content being viewed by others
References
Clavel MA, Magne J, Pibarot P (2016) Low-gradient aortic stenosis. Eur Heart J 37:2645–2657
Pereira JJ, Lauer MS, Bashir M et al (2002) Survival after aortic valve replacement for severe aortic stenosis with low transvalvular gradients and severe left ventricular dysfunction. J Am Coll Cardiol 39:1356–1363
Monin JL, Quéré JP, Monchi M et al (2003) Low-gradient aortic stenosis: operative risk stratification and predictors for long-term outcome: a multicenter study using dobutamine stress hemodynamics. Circulation 108:319–324
Connolly HM, Oh JK, Schaff HV et al (2000) Severe aortic stenosis with low transvalvular gradient and severe left ventricular dysfunction:result of aortic valve replacement in 52 patients. Circulation 101:1940–1946
Clavel MA, Fuchs C, Burwash IG et al (2008) Predictors of outcomes in low-flow, low-gradient aortic stenosis: results of the multicenter TOPAS Study. Circulation 118:S234–S242
Mack MJ, Leon MB, Thourani VH et al (2019) Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med 380:1695–1705
Popma JJ, Deeb GM, Yakubov SJ et al (2019) Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med 380:1706–1715
Chetcuti SJ, Deeb GM, Popma JJ et al (2019) Self-expanding transcatheter aortic valve replacement in patients with low-gradient aortic stenosis. JACC Cardiovasc Imaging 12:67–80
Ribeiro HB, Lerakis S, Gilard M et al (2018) Transcatheter aortic valve replacement in patients with low-flow, low-gradient aortic stenosis: the TOPAS-TAVI registry. J Am Coll Cardiol 71:1297–1308
Bonow RO, Brown AS, Gillam LD et al (2018) ACC/AATS/AHA/ASE/EACTS/HVS/SCA/SCAI/SCCT/SCMR/STS 2017 appropriate use criteria for the treatment of patients with severe aortic Stenosis: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, European Association for Cardio-Thoracic Surgery, Heart Valve Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons. J Am Soc Echocardiogr 31:117–147
Martin AK, Mohananey D, Ranka S et al (2018) The 2017 European Society of Cardiology (ESC)/European Association of Cardiothoracic Surgeons (EACTS) Guidelines for management of valvular heart disease-highlights and perioperative implications. J Cardiothorac Vasc Anesth 32:2810–2816
Kappetein AP, Head SJ, Généreux P et al (2013) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Thorac Cardiovasc Surg 145:6–23
Pellegrini C, Rheude T, Trenkwalder T et al (2019) One year VARC-2-defined clinical outcomes after transcatheter aortic valve implantation with the SAPIEN 3. Clin Res Cardiol 108:1258–1265
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Kataoka A, Watanabe Y, Kozuma K et al (2018) Prognostic impact of low-flow severe aortic stenosis in small-body patients undergoing TAVR: The OCEAN-TAVI Registry. JACC Cardiovasc Imaging 11:659–669
Maes F, Lerakis S, Barbosa Ribeiro H et al (2019) Outcomes from transcatheter aortic valve replacement in patients with low-flow, low-gradient aortic stenosis and left ventricular ejection fraction less than 30%: a substudy from the TOPAS-TAVI Registry. JAMA Cardiol 4:64–70
Codner P, Levi A, Gargiulo G et al (2016) Impact of renal dysfunction on results of transcatheter aortic valve replacement outcomes in a large multicenter cohort. Am J Cardiol 118:1888–1896
Pineda AM, Kevin Harrison J, Kleiman NS et al (2019) Clinical impact of baseline chronic kidney disease in patients undergoing transcatheter or surgical aortic valve replacement. Catheter Cardiovasc Interv 93:740–748
Taniguchi Y, Sakakura K, Yuri K et al. Determinants of prolonged hospitalization in patients who underwent trans-femoral transcatheter aortic valve implantation. Postepy w kardiologii interwencyjnej = Adv Interv Cardiol 2019; 15: 431–8.
Sannino A, Gargiulo G, Schiattarella GG et al (2014) Increased mortality after transcatheter aortic valve implantation (TAVI) in patients with severe aortic stenosis and low ejection fraction: a meta-analysis of 6898 patients. Int J Cardiol 176:32–39
Dahou A, Magne J, Clavel MA et al (2015) Tricuspid regurgitation is associated with increased risk of mortality in patients with low-flow low-gradient aortic stenosis and reduced ejection fraction: results of the multicenter TOPAS Study (True or Pseudo-Severe Aortic Stenosis). JACC Cardiovasc Interv 8:588–596
Shamekhi J, Sugiura A, Tabata N et al (2020) Impact of tricuspid regurgitation in patients undergoing transcatheter aortic valve replacement. JACC Cardiovasc Interv 13:1135–1137
Winter MP, Bartko PE, Krickl A et al (2020) Adaptive development of concomitant secondary mitral and tricuspid regurgitation after transcatheter aortic valve replacement. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jeaa106
Taramasso M, Benfari G, van der Bijl P et al (2019) Transcatheter versus medical treatment of patients with symptomatic severe tricuspid regurgitation. J Am Coll Cardiol 74:2998–3008
Elmariah S, Fearon WF, Inglessis I et al (2017) Transapical transcatheter aortic valve replacement is associated with increased cardiac mortality in patients with left ventricular dysfunction: insights from the PARTNER I Trial. JACC Cardiovasc Interv 10:2414–2422
Ribeiro HB, Nombela-Franco L, Munoz-Garcia AJ et al (2015) Predictors and impact of myocardial injury after transcatheter aortic valve replacement: a multicenter registry. J Am Coll Cardiol 66:2075–2088
Van Belle E, Vincent F, Labreuche J et al (2020) Balloon-expandable versus self-expanding transcatheter aortic valve replacement: a propensity-matched comparison from the FRANCE-TAVI Registry. Circulation 141:243–259
Hellhammer K, Piayda K, Afzal S et al (2018) The latest evolution of the Medtronic CoreValve system in the era of transcatheter aortic valve replacement: matched comparison of the Evolut PRO and Evolut R. JACC Cardiovasc Interv 11:2314–2322
Leon MB, Smith CR, Mack M et al (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Généreux P, Webb JG, Svensson LG et al (2012) Vascular complications after transcatheter aortic valve replacement: insights from the PARTNER (Placement of AoRTic TraNscathetER Valve) trial. J Am Coll Cardiol 60:1043–1052
Hayashida K, Lefèvre T, Chevalier B et al (2012) Impact of post-procedural aortic regurgitation on mortality after transcatheter aortic valve implantation. JACC Cardiovasc Interv 5:1247–1256
Acknowledgement
We thank Dr. Meghan Campbell (scientific coordinator for the Heart Center Bonn, Bonn, Germany) for proofreading the manuscript. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
392_2020_1752_MOESM1_ESM.pdf
Supp. Figure 1. Study flow chart. The study cohort comprised of 219 consecutive LF-LG AS patients undergoing TAVR from 2008 to 2018 in two high-volume German centers. Supp. Figure 2. Receiver operating characteristics curves for each scoring system. Figures depicting the area under the curve (AUC) for each scoring system. The AUC for RRS was higher compared to other traditional surgical risk scores (logistic EuroSCORE, EuroSCORE and STS-PROM) (PDF 629 kb)
Rights and permissions
About this article
Cite this article
Wilde, N., Sugiura, A., Sedaghat, A. et al. Risk of mortality following transcatheter aortic valve replacement for low-flow low-gradient aortic stenosis. Clin Res Cardiol 110, 391–398 (2021). https://doi.org/10.1007/s00392-020-01752-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01752-4