Abstract
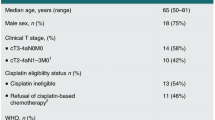
Immune checkpoint therapy is being tested in the neoadjuvant setting for patients with localized urothelial carcinoma1,2, with one study reporting data in cisplatin-ineligible patients who received anti-PD-L1 monotherapy2. The study reported that patients with bulky tumors, a known high-risk feature defined as greater than clinical T2 disease, had fewer responses, with pathological complete response rate of 17%2. Here we report on the first pilot combination neoadjuvant trial (NCT02812420) with anti-PD-L1 (durvalumab) plus anti-CTLA-4 (tremelimumab) in cisplatin-ineligible patients, with all tumors identified as having high-risk features (n = 28). High-risk features were defined by bulky tumors, variant histology, lymphovascular invasion, hydronephrosis and/or high-grade upper tract disease3,4,5. The primary endpoint was safety and we observed 6 of 28 patients (21%) with grade ≥3 immune-related adverse events, consisting of asymptomatic laboratory abnormalities (n = 4), hepatitis and colitis (n = 2). We also observed pathological complete response of 37.5% and downstaging to pT1 or less in 58% of patients who completed surgery (n = 24). In summary, we provide initial safety, efficacy and biomarker data with neoadjuvant combination anti-PD-L1 plus anti-CTLA-4, which warrants further development for patients with localized urothelial carcinoma, especially cisplatin-ineligible patients with high-risk features who do not currently have an established standard-of-care neoadjuvant treatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data generated or analyzed during this study are included in this article along with its supplementary information files. All WES and gene expression NanoString data that support the findings of this study (Fig. 2a–c and Extended Data Figs. 4, 5 and 8) are deposited in the European Genome-phenome Archive under accession number EGAS00001004074. The links to databases used for analysis of the data presented in this study: COSMIC, EXAC, ESP600, 1000 Genomes and UCSC Genome Browser are listed in Supplementary Table 6. All other relevant data related to the current study are available from the corresponding author (P.S.) on reasonable request, which does not include confidential patient information.
Code availability
No custom codes were used in analyses reported in this study. All relevant references are provided in the Methods.
References
Necchi, A. et al. Pembrolizumab as neoadjuvant therapy before radical cystectomy in patients with muscle-invasive urothelial bladder carcinoma (PURE-01): an open-label, single-arm, phase II study. J. Clin. Oncol. 36, 3353–3360 (2018).
Powles, T. et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nat. Med. 25, 1706–1714 (2019).
Culp, S. H. et al. Refining patient selection for neoadjuvant chemotherapy before radical cystectomy. J. Urol. 191, 40–47 (2014).
Siefker-Radtke, A. O. et al. A phase 2 clinical trial of sequential neoadjuvant chemotherapy with ifosfamide, doxorubicin, and gemcitabine followed by cisplatin, gemcitabine, and ifosfamide in locally advanced urothelial cancer: final results. Cancer 119, 540–547 (2013).
Moschini, M. et al. Validation of preoperative risk grouping of the selection of patients most likely to benefit from neoadjuvant chemotherapy before radical cystectomy. Clin. Genitourin. Cancer 15, e267–e273 (2017).
Plimack, E. R. et al. Accelerated methotrexate, vinblastine, doxorubicin, and cisplatin is safe, effective, and efficient neoadjuvant treatment for muscle-invasive bladder cancer: results of a multicenter phase II study with molecular correlates of response and toxicity. J. Clin. Oncol. 32, 1895–1901 (2014).
Griffiths, G., Hall, R., Sylvester, R., Raghavan, D. & Parmar, M. K. International phase III trial assessing neoadjuvant cisplatin, methotrexate, and vinblastine chemotherapy for muscle-invasive bladder cancer: long-term results of the BA06 30894 trial. J. Clin. Oncol. 29, 2171–2177 (2011).
Iyer, G. et al. Multicenter prospective phase II trial of neoadjuvant dose-dense gemcitabine plus cisplatin in patients with muscle-invasive bladder cancer. J. Clin. Oncol. 36, 1949–1956 (2018).
Grossman, H. B. et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N. Engl. J. Med. 349, 859–866 (2003).
Sonpavde, G. et al. Quality of pathologic response and surgery correlate with survival for patients with completely resected bladder cancer after neoadjuvant chemotherapy. Cancer 115, 4104–4109 (2009).
Rosenblatt, R. et al. Pathologic downstaging is a surrogate marker for efficacy and increased survival following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive urothelial bladder cancer. Eur. Urol. 61, 1229–1238 (2012).
Galsky, M. D. et al. Treatment of patients with metastatic urothelial cancer “unfit” for cisplatin-based chemotherapy. J. Clin. Oncol. 29, 2432–2438 (2011).
National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Bladder Cancer, Vol. 2019 (NCCN, 2019).
Bellmunt, J. et al. Bladder cancer: ESMO Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 25, iii40–iii48 (2014).
European Association of Urology. European Association of Urology Guidelines (EAU Guidelines Office, 2019).
Sharma, P. et al. Nivolumab monotherapy in recurrent metastatic urothelial carcinoma (CheckMate 032): a multicentre, open-label, two-stage, multi-arm, phase 1/2 trial. Lancet Oncol. 17, 1590–1598 (2016).
Powles, T. et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: updated results from a phase 1/2 open-label study. JAMA Oncol. 3, e172411 (2017).
Powles, T. et al. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): a multicentre, open-label, phase 3 randomised controlled trial. Lancet 391, 748–757 (2018).
Bellmunt, J. et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N. Engl. J. Med. 376, 1015–1026 (2017).
Patel, M. R. et al. Avelumab in metastatic urothelial carcinoma after platinum failure (JAVELIN Solid Tumor): pooled results from two expansion cohorts of an open-label, phase 1 trial. Lancet Oncol. 19, 51–64 (2018).
Balar, A. V. et al. First-line pembrolizumab in cisplatin-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): a multicentre, single-arm, phase 2 study. Lancet Oncol. 18, 1483–1492 (2017).
Balar, A. V. et al. Atezolizumab as first-line treatment in cisplatin-ineligible patients with locally advanced and metastatic urothelial carcinoma: a single-arm, multicentre, phase 2 trial. Lancet 389, 67–76 (2017).
Millikan, R. et al. Integrated therapy for locally advanced bladder cancer: final report of a randomized trial of cystectomy plus adjuvant M-VAC versus cystectomy with both preoperative and postoperative M-VAC. J. Clin. Oncol. 19, 4005–4013 (2001).
Wolchok, J. D. et al. Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 369, 122–133 (2013).
Motzer, R. J. et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N. Engl. J. Med. 378, 1277–1290 (2018).
Bamias, A. et al. Impact of contemporary patterns of chemotherapy utilization on survival in patients with advanced cancer of the urinary tract: a Retrospective International Study of Invasive/Advanced Cancer of the Urothelium (RISC). Ann. Oncol. 29, 361–369 (2018).
Kim, J. et al. The cancer genome atlas expression subtypes stratify response to checkpoint inhibition in advanced urothelial cancer and identify a subset of patients with high survival probability. Eur. Urol. 75, 961–964 (2019).
Wei, S. C. et al. Distinct cellular mechanisms underlie anti-CTLA-4 and anti-PD-1 checkpoint blockade. Cell 170, 1120–1133 e1117 (2017).
Wei, S. C. et al. Combination anti-CTLA-4 plus anti-PD-1 checkpoint blockade utilizes cellular mechanisms partially distinct from monotherapies. Proc. Natl Acad. Sci. USA 116, 22699–22709 (2019).
Wei, S. C. et al. Negative co-stimulation constrains T cell differentiation by imposing boundaries on possible cell states. Immunity 50, 1084–1098 (2019).
Miao, D. et al. Genomic correlates of response to immune checkpoint blockade in microsatellite-stable solid tumors. Nat. Genet. 50, 1271–1281 (2018).
Ng Tang, D. et al. Increased frequency of ICOS+CD4+ T cells as a pharmacodynamic biomarker for anti-CTLA-4 therapy. Cancer Immunol. Res. 1, 229–234 (2013).
Liakou, C. I. et al. CTLA-4 blockade increases IFN-γ-producing CD4++ ICOShihi cells to shift the ratio of effector to regulatory T cells in cancer patients. Proc. Natl Acad. Sci. USA 105, 14987–14992 (2008).
Carthon, B. C. et al. Preoperative CTLA-4 blockade: tolerability and immune monitoring in the setting of a presurgical clinical trial. Clin. Cancer Res. 16, 2861–2871 (2010).
Cabrita, R. et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature 577, 561–565 (2020).
Helmink, B. A. et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577, 549–555 (2020).
Petitprez, F. et al. B cells are associated with survival and immunotherapy response in sarcoma. Nature 577, 556–560 (2020).
Amaria, R. N. et al. Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat. Med. 24, 1649–1654 (2018).
Forde, P. M. et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N. Engl. J. Med. 378, 1976–1986 (2018).
Van der Heijden, M. S. et al. Pre-operative ipilimumab and nivolumab in locoregionally advanced, stage III, urothelial cancer (NABUCCO). Ann. Oncol. 30, v358 (2019).
Thall, P. F., Simon, R. M. & Estey, E. H. Bayesian sequential monitoring designs for single-arm clinical trials with multiple outcomes. Stat. Med. 14, 357–379 (1995).
Nowicka, M. et al. CyTOF workflow: differential discovery in high-throughput high-dimensional cytometry datasets. F1000Res 6, 748 (2017).
Lee, E., Chuang, H.-Y., Kim, J.-W., Ideker, T. & Lee, D. Inferring pathway activity toward precise disease classification. PLoS Comput. Biol. 4, e1000217 (2008).
Herbst, R. S. et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature 515, 563 (2014).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows–Wheeler transform. Bioinforma. 25, 1754–1760 (2009).
Cibulskis, K. et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219 (2013).
Ye, K., Schulz, M. H., Long, Q., Apweiler, R. & Ning, Z. Pindel: a pattern growth approach to detect break points of large deletions and medium sized insertions from paired-end short reads. Bioinforma. 25, 2865–2871 (2009).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Wang, Y.-Y. et al. HLA-VBSeq v2: improved HLA calling accuracy with full-length Japanese class-I panel. Hum. Genome Var. 6, 29 (2019).
Hundal, J. et al. pVAC-seq: a genome-guided in silico approach to identifying tumor neoantigens. Genome Med. 8, 11 (2016).
Hundal, J. et al. Accounting for proximal variants improves neoantigen prediction. Nat. Genet. 51, 175–179 (2019).
Mayakonda, A., Lin, D. C., Assenov, Y., Plass, C. & Koeffler, H. P. Maftools: efficient and comprehensive analysis of somatic variants in cancer. Genome Res. 28, 1747–1756 (2018).
Nombela, P. et al. BRCA2 and other DDR genes in prostate cancer. Cancers 11, 352 (2019).
Stack, E. C., Wang, C., Roman, K. A. & Hoyt, C. C. Multiplexed immunohistochemistry, imaging, and quantitation: a review, with an assessment of tyramide signal amplification, multispectral imaging and multiplex analysis. Methods 70, 46–58 (2014).
Acknowledgements
This research is supported in part through an alliance between AstraZeneca/MedImmune and the MDACC Immunotherapy Platform, the MD Anderson Physician Scientist Award (J.G.), Khalifa Physician Scientist Award (J.G.), Andrew Sabin Family Foundation Fellows Award (J.G.) and Wendy and Leslie Irvin Barnhart Fund (J.G.). We thank the genomic medicine, CGL core team for WES. In addition, we thank Ashura Khan (Program Director) and the Immunotherapy Platform team for technical support. P.S. and J.P.A. are members of the Parker Institute for Cancer Immunotherapy, which supports their research work at MDACC.
Author information
Authors and Affiliations
Contributions
P.S. conceptualized clinical trial and design and supervision of immune monitoring studies. J.G. served as Principal Investigator of the clinical trial and supervised the clinical trial. R.S.T. and Y.S. performed statistical analysis. J.G., P.S., S.S.Y., S.G. and O.A. Contributed to writing, review and/or revision of the manuscript. N.M., C.D., A.S.-R., M.T.C., C.C.G, A.M.K., S.F.M., J.C.A., A.Y.S., P.M., P.C., J.W., J.N.P., J.M.B., F.D., S.B., W.L., Y.S., Y.Z., M.D.M., Y.W., J.C., J.Z., A.F. and J.P.A. provided administrative, technical or material support (reporting or organizing data and constructing databases).
Corresponding authors
Ethics declarations
Competing interests
J.G. served as a consultant on a scientific advisory board for AstraZeneca and received compensation as an advisor. A.M.K. served on a scientific advisory board for AstraZeneca and received compensation as an advisor. A.S.-R. is on a scientific advisory board for AstraZeneca and receives compensation as an advisor. J.B. became an AstraZeneca employee after the work on this manuscript was completed. P.S. and J.P.A. do not have any competing interest with this manuscript. However, they provided a list of all disclosures for transparency. P.S. has ownership in Jounce, BioNTx, Constellation, Oncolytics, BioAtla, Forty-Seven, Apricity, Polaris, Marker Therapeutics, Codiak, ImaginAb, Dragonfly, Lytix, Lava Therapeutics, Infinity Pharma, Adaptive Biotechnologies and Hummingbird. J.P.A. has ownership in Jounce, BioNTx, BioAtla, Forty-Seven, Apricity, Polaris, Marker Therapeutics, Adaptive Biotechnologies and Codiak. P.S. serves as a consultant for Constellation, Jounce, Kite Pharma, Neon, BioAtla, Oncolytics Biotech, Forty-Seven, Polaris, Apricity, Marker Therapeutics, Codiak, ImaginAb, Dragonfly, Lava Therapeutics, Infinity Pharma, Lytix and Hummingbird. J.P.A. serves as a consultant for Jounce, Neon, Forty-Seven, Apricity, Polaris, Marker Therapeutics, Codiak, ImaginAb, Lava Therapeutics, Dragonfly, Lytix and Hummingbird. J.G. serves as a consultant for ARMO Biosciences, CRISPR Therapeutics, Jounce, Nektar, Pfizer, Polaris and Symphogen.
Additional information
Peer review information Javier Carmona was the primary editor on this article, and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Trial schema (NCT02812420).
Patients each had baseline TURBT for tumor resection, pathologic diagnosis, staging, and risk stratification. The first cohort of 28 patients each received durvalumab at 1500 mg plus tremelimumab 75 mg every 4 weeks for a total of 2 doses. The second cohort of 17 patients was planned to receive durvalumab at 1500 mg plus tremelimumab 300 mg x 1 dose and then only durvalumab at 1500 mg 4 weeks later (not reported in this manuscript). Surgery (radical cystectomy or applicable surgery to resect tumors) was performed 4–6 weeks after the last dose of treatment. A cystoscopy (or applicable imaging) with optional TURBT was performed at week 4 (post-treatment dose 1) to rule out patients with rapid disease progression. In the case of rapid disease progression, these patients were taken off the trial per clinical judgement from the treating physicians and the principal investigators. Pre- and post-treatment blood and tumor tissues were collected for correlative studies. TURBT-transurethral resection of bladder tumor. * A cystoscopy and optional TURBT prior to second dose.
Extended Data Fig. 2 Response rate in association with adverse events or variant histology.
a, Pathologic response based on grade of immune-related adverse events. b, Pathologic response in pure urothelial carcinoma vs. urothelial carcinoma with variant histology.
Extended Data Fig. 3 Distribution of PD-L1 expression in the immune and tumor cell compartments in pre-treatment tumor tissues of responders compared to non-responders.
a, Box plot showing density of immune cells expressing PD-L1 in pre-treatment tumor tissue samples from responders (R, n = 13, red) and non-responders (NR, n = 13, blue). b, Box plot showing density of tumor cells expressing PD-L1 in pre-treatment tumor tissue samples from responders (R, n = 13, red) and non-responders (NR, n = 13, blue). In the box plots of a and b, the horizontal bold line represents the median. The lower and upper hinges of the box correspond to the first and third quartiles (the 25th and 75th percentiles); the upper whisker extends from the hinge to the largest value no further than 1.5 × IQR from the hinge (where IQR is the distance between the first and third quartiles); and the lower whisker extends from the hinge to the smallest value at most 1.5 × IQR from the hinge. Statistical analysis was performed using two-sided Wilcoxon rank-sum test. P < 0.05 is considered statistically significant.
Extended Data Fig. 4 Predicted neoantigen load in pre-treatment tumor tissue samples.
Box plot showing neoantigen load did not differ significantly between the R (n = 13, red) and NR (n = 10, blue) patients. The horizontal bold line represents the median. The lower and upper hinges of the box correspond to the first and third quartiles (the 25th and 75th percentiles); the upper whisker extends from the hinge to the largest value no further than 1.5 × IQR from the hinge (where IQR is the distance between the first and third quartiles); and the lower whisker extends from the hinge to the smallest value at most 1.5 × IQR from the hinge. The P value was calculated using two-sided Wilcoxon rank sum test. P < 0.05 is considered statistically significant.
Extended Data Fig. 5 Mutational analysis of specific genes in pre-treatment tumor tissue samples in correlation with response.
a, CoOncoplot showing mutations in DNA-damage response (DDR) genes in responders (R, n = 13, right) and non-responders (NR, n = 10, left). b, CoOncoplot showing mutations in KRAS, PIK3CA, PBRM1, EGFR, NRAS, APC2 and FGFR genes in responders (R, n = 13, right) and non-responders (NR, n = 10, left). Each row represents a gene and the gene name is listed in the middle of the two heatmaps and their respective frequencies are listed on the left of the first heatmap (NR) and on the right of the second heatmap (R). Each column represents a patient. Each row represents a gene and the gene name is listed in the middle of the two heatmaps and their respective frequencies are listed on the left of the first heatmap (NR) and on the right of the second heatmap (R). The p-values comparing the distribution of mutations between R and NR are shown within parentheses next to each gene name. N/A denotes not applicable. The colors of rectangles in the body of the heatmap indicates different types of somatic mutations and the key identifying each mutation type is shown at the bottom. P values calculated using two-sided Fisher’s exact test.
Extended Data Fig. 6 Biological responses in peripheral blood and tumor tissue samples after treatment with durvalumab plus tremelimumab.
a–e, Immune profiling by CyTOF analysis was performed on peripheral blood samples collected pre- and post-treatment. a-c, Categorical scatter plots showing frequency of subsets of CD4 T cells expressing PD-1, LAG3, and TIM3 pre- and post-treatment. Pre- indicates pre-treatment (blue circles; n = 22); Post1 indicates post-treatment, dose 1 (brown squares; n = 22); Post2 indicates post-treatment, dose 2 (pink triangles; n = 21). d, Categorical scatter plot showing frequency of ICOS + CD4 T cells pre- and post-treatment. Sample numbers and color schema same as in a-c. For a-d, error bars are shown as mean±standard deviation. e, Paired dot plots showing frequency of ICOS+ CD4 T cells in matched pre- and post-treatment (Post2) blood samples. NR indicates non-responders (n = 7); R indicates responders (n = 10). P values were calculated using the two-sided Wilcoxon rank-sum test in a-d and Wilcoxon signed-rank test in e. f, Representative multiplex immunofluorescence images (magnification; 20X) from one non-responder, NR (top) and one responder, R (bottom) patient at pre-treatment, Pre (left) and post-treatment, Post2 (right) time points. The samples were stained for the following markers: ICOS (red) and CD4 (green). Nuclei were stained with DAPI (blue). White arrows point to CD4 T cells expressing ICOS. Matched pre- and post-treatment samples from 10 patients (R = 5 and NR = 5) had similar analyses completed with corresponding images that were used to generate the data in g. g, Paired dot plots showing percentage of ICOS+CD4 T cells in matched pre- (blue circles) and post- (pink triangles) treatment tumor tissue samples from non-responders, NR (n = 5) and responders, R (n = 5). P values were calculated using the two-sided Wilcoxon rank-sum test. P < 0.05 is considered statistically significant.
Extended Data Fig. 7 Distribution of B cells, CD4 T cells, and CD8 T cells in pre-treatment tumor tissues of responders compared to non-responders.
a, Box plot showing density of B cells (CD20 + ) in pre-treatment tumor tissue samples from responders (R, n = 10) and non-responders (NR, n = 9). b, Box plot showing density of CD4 T cells in pre-treatment tumor tissue samples from responders (R, n = 10) and non-responders (NR, n = 9). c, Box plot showing density of CD8 T cells in pre-treatment tumor tissue samples from responders (R, n = 10) and non-responders (NR, n = 9). In the box plots, the horizontal bold line represents the median. The lower and upper hinges of the box correspond to the first and third quartiles (the 25th and 75th percentiles); the upper whisker extends from the hinge to the largest value no further than 1.5 × IQR from the hinge (where IQR is the distance between the first and third quartiles); and the lower whisker extends from the hinge to the smallest value at most 1.5 × IQR from the hinge. Statistical analysis was performed using two-sided Wilcoxon rank-sum test. P < 0.05 is considered statistically significant.
Extended Data Fig. 8 Association of POU2AF1 gene and TLS signature with response.
Pre-treatment tumor tissue samples from patients with TLS were analyzed by Nanostring. a, Box plot showing a comparison of POU2AF1 gene expression level between R (n = 9, red) and NR (n = 7, blue) patients. b, Box plot showing a comparison of 4-gene TLS signature derived from gene expression profiling of pre-treatment tumor tissue samples from R (n = 9, red) and NR (n = 7, blue) patients. In the box plots, the horizontal bold line represents the median. The lower and upper hinges of the box correspond to the first and third quartiles (the 25th and 75th percentiles); the upper whisker extends from the hinge to the largest value no further than 1.5 × IQR from the hinge (where IQR is the distance between the first and third quartiles); and the lower whisker extends from the hinge to the smallest value at most 1.5 × IQR from the hinge. P values were calculated using the two-sided unpaired student’s t–test, P < 0.05 is considered statistically significant.
Supplementary information
Supplementary Information
Supplementary Tables 1–6.
Rights and permissions
About this article
Cite this article
Gao, J., Navai, N., Alhalabi, O. et al. Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma. Nat Med 26, 1845–1851 (2020). https://doi.org/10.1038/s41591-020-1086-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-1086-y
This article is cited by
-
Pan-cancer analysis reveals PDK family as potential indicators related to prognosis and immune infiltration
Scientific Reports (2024)
-
Spatial relationships in the urothelial and head and neck tumor microenvironment predict response to combination immune checkpoint inhibitors
Nature Communications (2024)
-
Turning up the heat: CTLA4 blockade in urothelial cancer
Nature Reviews Urology (2024)
-
Tertiary lymphoid structures predict survival and response to neoadjuvant therapy in locally advanced rectal cancer
npj Precision Oncology (2024)
-
Increasing cure rates of solid tumors by immune checkpoint inhibitors
Experimental Hematology & Oncology (2023)