Abstract
Aims
The first reports of declining hospital admissions for major cardiovascular emergencies during the COVID-19 pandemic attracted public attention. However, systematic evidence on this subject is sparse. We aimed to investigate the rate of emergent hospital admissions, subsequent invasive treatments and comorbidities during the COVID-19 pandemic in Germany.
Methods and results
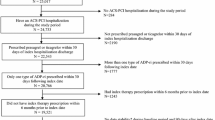
This was a retrospective analysis of health insurance claims data from the second largest insurance fund in Germany, BARMER. Patients hospitalized for acute myocardial infarction, acute limb ischemia, aortic rupture, stroke or transient ischemic attack (TIA) between January 1, 2019, and May 31, 2020, were included. Admission rates per 100,000 insured, invasive treatments and comorbidities were compared from January–May 2019 (pre-COVID) to January–May 2020 (COVID). A total of 115,720 hospitalizations were included in the current analysis (51.3% females, mean age 72.9 years). Monthly admission rates declined from 78.6/100,000 insured (pre-COVID) to 70.6/100,000 (COVID). The lowest admission rate was observed in April 2020 (61.6/100,000). Administration rates for ST-segment elevation myocardial infarction (7.3–6.6), non-ST-segment elevation myocardial infarction (16.8–14.6), acute limb ischemia (5.1–4.6), stroke (35.0–32.5) and TIA (13.7–11.9) decreased from pre-COVID to COVID. Baseline comorbidities and the percentage of these patients treated with interventional or open-surgical procedures remained similar over time across all entities. In-hospital mortality in hospitalizations for stroke increased from pre-COVID to COVID (8.5–9.8%).
Conclusions
Admission rates for cardiovascular and cerebrovascular emergencies declined during the pandemic in Germany, while patients’ comorbidities and treatment allocations remained unchanged. Further investigation is warranted to identify underlying reasons and potential implications on patients’ outcomes.
Graphic abstract

Similar content being viewed by others
Introduction
Since its outbreak in Wuhan, Hubei Province, China, in December 2019, the novel SARS coronavirus (SARS-CoV-2) has spread rapidly, causing an outbreak of acute and severe respiratory illness worldwide [1]. The first disease outbreak news from the World Health Organization (WHO) had been issued January 5, 2020. After a rapid spread of SARS-CoV-2 in Italy [2] and other European regions, several countries issued strict infection control measures. Elective in-hospital procedures were widely cancelled or postponed to provide additional capacities for the treatment of COVID-patients in Germany, starting in March 2020 [3, 4].
While an association between acute viral respiratory disease and subsequent cardiovascular events had been described for other diseases (e.g., influenza) [5, 6], several centers reported a decline in hospital admissions for acute cardiovascular and cerebrovascular emergencies during the COVID pandemic [7,8,9,10,11,12,13,14,15,16,17,18,19]. Since acute cardiovascular and cerebrovascular diseases remain leading causes for morbidity and mortality, further investigation of this concerning trend is warranted to identify potential implications for both health-care professionals and regulators.
This analysis sought to determine trends in admission rates, invasive treatments, and comorbidities of inpatients treated for cardiovascular and cerebrovascular emergencies during the SARS-CoV-2 pandemic in Germany.
Methods
Study design
This was a retrospective analysis of routinely collected health insurance claims data. Based on their primary or admission diagnosis, we included all patients with inpatient treatment between January 1, 2019, and May 31, 2020, for cardiovascular and cerebrovascular emergencies. These included (1A) ST-segment elevation myocardial infarction (STEMI), (1B) non-ST-segment elevation myocardial infarction (NSTEMI), (2) acute limb ischemia, (3) acute aortic rupture, (4A) acute stroke and (4B) transient ischemic attack (TIA) (for detailed coding see Supplemental Table 1).
Data collected during the pandemic (COVID: January through May 2020) were compared to a control period in the previous year (pre-COVID: January through May 2019). The primary study end point was the absolute number of monthly hospitalizations and the corresponding admission rate per 100,000 insured inhabitants. Secondary end points included the absolute number and proportion of invasive procedures provided to these patients (for detailed coding see Supplemental Table 1), as well as all-cause mortality during the hospital stay and the proportion of relevant comorbidities and socio-demographic variables.
Sample and database
The longitudinal data of Germany’s second-largest insurance fund, BARMER, includes the outpatient and inpatient medical care provided to up to 9.4 million (from 2008 to 2020) German citizens (13.2% of Germany’s population) involving more than 24 million hospitalizations between January 1, 2008, and May 31, 2020. The BARMER cohort is similar to Western European countries and has been widely used for research projects before [20, 21]. A regular random sample validation of internal and external validity is performed by the Medical Service of the Health Funds (MDK) in Germany, and various peer-reviewed validation studies have been published before [22, 23].
Study variables
The diagnoses and comorbidities routinely collected in health insurance claims data follow the commonly accepted international standard for reporting diseases and health conditions using World Health Organization (WHO) International Classification of Diseases in its 10th revision of the German Modification (ICD-10-GM) and Operations and Procedures Codes (OPS) as a German adaptation of the International Classification of Procedures in Medicine (ICPM) by WHO.
The primary diagnosis of the hospital case was used to discriminate between the cardiovascular or cerebrovascular emergencies. In approximately 0.6% of the most current hospitalizations (in May 2020), the admission diagnosis was utilized on a supplementary basis if no primary diagnosis was available. In addition to age (in years) and gender (dichotomized), we used the following ICD-10 codes to identify diabetes (E10*, E11*, E12*, E13*, E14*), hypertension (I10*, I11*, I12*, I13*, I14*, I15*), heart failure (I50*), atrial fibrillation (I48*), chronic ischemic heart disease (I25*), obesity (E66*), chronic renal disease (N18*), chronic obstructive pulmonary disease (COPD, J44*), and cancer (C00-97*) as comorbidities among the study sample. All-cause mortality was provided during the index hospital stay.
Statistical analysis
We summarized the baseline characteristics of the patients with means for age and with percentages and 95% confidence interval (CI) for discrete variables. A comparison of 95% CI and Chi square test was used to test for differences. For Table 1, we compared symmetric samples from January 01, 2019, to May 31, 2019 (pre-COVID), vs. January 01, 2020, to May 31, 2020 (COVID), to adjust for seasonal effects. Missing data (0.6%) were handled by exclusion.
As additional sensitivity analysis, we compared the study variables using shorter time periods (e.g., March 2019 vs. March 2020, April 2019 vs. April 2020, May 2019 vs. May 2020). Besides, we determined the admission rates using either both primary and admission diagnosis vs. only primary diagnosis (only reimbursed cases).
Data processing was performed with software SAS version 9.04 (SAS Institute, North Carolina, USA) and SPSS version 25 (IBM Corporation, New York, USA), visualization was performed with software Adobe Illustrator version 24.1.2 (Adobe, California, USA).
Results
We identified 115,720 hospitalizations (mean age 72.9 years, 51.3% females, 95% CI 51.0% to 51.6%) for cardiovascular or cerebrovascular emergencies between January 1, 2019, and May 31, 2020 (monthly mean: 6,807 patients) (Table 1). Among all hospitalizations, a total of 8,202 deaths occurred. The monthly hospital admission rate for cardiovascular or cerebrovascular emergencies declined from a maximum of 83.8 per 100,000 in January 2019 to a minimum of 61.6 per 100,000 in April 2020, which increased to 67.1 per 100,000 in May 2020 (mean: 75.2 per 100,000).
Comparing pre-COVID to COVID time frames, overall monthly admission rates declined from 78.6 per 100,000 to 70.6 per 100,000. This was observed across all strata (Fig. 1): admission rates per 100,000 during COVID compared to pre-COVID decreased for STEMI (7.3 vs. 6.6, − 12.2% percentage points, p.p.), NSTEMI (16.8 vs. 14.6, − 15.2% p.p.), acute limb ischemia (5.1 vs. 4.6, − 12.4% p.p.), stroke (35.0 vs. 32.5, − 8.9% p.p.), and TIA (13.7 vs. 11.9, − 14.6% p.p.). No relevant differences were observed for aortic ruptures (0.6 vs. 0.5) (Fig. 1 and Table 1). The lowest admission rates were noted in April 2020 (61.6 per 100,000) with declines in STEMI (− 16.3%), NSTEMI (− 21.5%), acute limb ischemia (− 22.5%), stroke (− 17.8%), and TIA (− 30.2%) compared to the respective rates in April 2019. For May 2020, slowly recovering admission rates were observed for NSTEMI, STEMI, ALI, stroke, and TIA compared to April 2020 (Fig. 1). The admission rates of NSTEMI and STEMI and the corresponding numbers of daily SARS-CoV-2 infections in Germany from January through May 2020 are depicted in Fig. 1a.
Monthly admission rates for cardiovascular and cerebrovascular emergencies per 100,000 insured in Germany for ST-segment elevation myocardial infarction (dark red) and non-ST-segment elevation myocardial infarction (light red) (a) for acute limb ischemia (b), aortic rupture (c), and acute stroke (dark green) and transient ischemic attack (light green) (d) between January 2019 and May 2020. The gray line with shade denotes the annual mean for 2019 with a corresponding limit of agreement
Comorbidities, cardiovascular risk profiles and socio-demographic variables were similar among patients admitted during COVID compared to pre-COVID eras (Table 1).
Besides patients admitted for stroke (8.5–9.8%), the in-hospital mortality was similar among patients admitted during COVID compared to pre-COVID eras (Table 1).
The percentage of patients admitted for cardiovascular or cerebrovascular emergencies, who underwent interventional or open-surgical procedures during the hospital stay, were similar between pre-COVID and COVID periods for STEMI (84.7–86.3%), NSTEMI (58.0–60.5%), acute limb ischemia (81.9–82.8%), aortic rupture (51.5–56.7%), stroke (18.4–19.1%), and TIA (2.1–2.2%) (Fig. 2 and Table 1). All sensitivity analyses were confirmative (not shown).
Percentage of patients admitted for cardiovascular and cerebrovascular emergencies, who underwent respective interventional or open-surgical treatment. Rates per month are given for ST-segment elevation myocardial infarction (dark red) and non-ST-segment elevation myocardial infarction (light red) (a) for acute limb ischemia (b), aortic rupture (c), and acute stroke (dark green) and transient ischemic attack (light green) (d) between January 2019 and May 2020. The gray line denotes the annual mean for 2019
Discussion
This analysis of a large dataset of routinely collected health insurance claims demonstrated a marked decrease in hospital admission rates for several cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany. These patients’ comorbidities and the percentage of them, who were treated invasively, remained unchanged.
A concerning decline of more than 40% in hospital admissions for acute coronary syndromes after the COVID-19 outbreak had been reported in smaller series of severely affected regions [9, 11,12,13,14, 18, 24]. We observed reductions of 12.2% in patients presenting with STEMI and 15.2% with NSTEMI in a large representative sample of the German population during a longer phase of observation (January through May 2020). The maximum decline of NSTEMI presentations was detected in April 2020 (− 21.5% compared to 2019), followed by a slow recovery in May 2020, essentially mirroring SARS-CoV-2 infection rates in Germany. These observations were of particular interest as—opposed to other countries—Germany was not affected as strongly by the COVID-19 pandemic and a significant limitations of health-care resources did not become evident. This may explain why we found a milder decline compared to regions heavily affected by the disease outbreak [25] and was in line with reports from other less-affected areas reporting reductions of approximately 25% in acute cases. Interestingly, admissions for several cardiovascular and cerebrovascular emergencies started to increase again in May, suggesting a potential recovery after a significant drop in new daily COVID-19 cases and a liberalization of public restrictions in Germany.
Similar trends were observed for patients with acute cerebrovascular and peripheral vascular diseases. Using surrogate markers for the quantity of care, a large recent analysis reported a decrease of 39% in March 2020 in patients presenting with acute ischemic stroke to US hospitals [8]. The results of the current study confirmed declines in strokes and TIA during the pandemic in Germany, albeit less severe. Consistent with these observations, we detected a marked decline in the admission rates for acute limb ischemia during the pandemic. Whether this translates into increased disease severity and worse outcomes as others have suggested [26] will need to be investigated.
Additional information on age, gender, and comorbidities revealed patient populations to be similar before and during the pandemic, arguing against the notion that milder affected patients might particularly refrain from seeking medical care, thus shifting the severity of diseases. Likewise, treatment allocation of the patients admitted remained unchanged. Furthermore, in the current study, patients presenting to the emergency departments with acute cardiovascular or cerebrovascular disease had a similar chance to receive interventional or open-surgical therapy before and during the pandemic in Germany. This seems to be an indicator for an ongoing high-level medical therapy during this time period. Since rapid diagnosis and treatment of acute coronary syndromes are important to avoid further complications [27, 28], recently published results from Italy are alarming reporting a delay in coronary revascularization and increasing rates of case fatality and major complications in patients suffering from acute myocardial infarction during COVID-19 [14]. To guide the management of acute coronary syndromes and cardiovascular disease during the COVID-19 pandemic and to contain collateral damage, the European Association of Percutaneous Cardiovascular Interventions and German Cardiac Society recently issued comprehensive expert documents [29, 30].
The root causes for the observed decline in acute admissions for cardiovascular and cerebrovascular diseases remain unclear and may be multifactorial: avoidance of medical care due to patient-based anxiety and fear of contagion during the pandemic may play an important role. However, an attitude toward increased deferrals of less urgent cases by health-care personnel and lifestyle changes among other confounders during the time of extensive social restrictions need to be evaluated as well. Patient information and public education will be of paramount importance to contain collateral damages caused by delayed medical treatment for acute cardiovascular and cerebrovascular diseases.
Most previous reports on this topic used either surveys [31], selective multi-center data, or surrogate parameters (e.g., use of imaging software) [8] to quantity patient care. Population-based data investigating emergency admissions in this setting validly remain scarce. Nevertheless, the following limitations merit consideration. First, health insurance claims data were not primarily collected for research purposes and retrospective observational studies are unsuitable to prove underlying causal relationships. However, data from health insurance claims, as used in this analysis, may help to identify potential implications for both health-care professionals and regulators at an early stage. Second, while longitudinal data were available between 2008 and today, pandemic measures in Germany began in February 2020 with no relevant follow-up available. Therefore, future analyses investigating patients’ outcomes are required. This is particularly important for mortality, albeit differentiating COVID-19-related mortality from mortality due to other causes in the light of COVID infection will remain complex from insurance claims data. Third, admission diagnoses were used for current analyses in a small share of cases in May 2020 (0.6%) if the main diagnosis was not yet submitted. However, comorbidities were only analyzed for individuals with complete datasets available to avoid classification bias. Last, the BARMER sample included a relevant proportion of the entire population in Germany. A selection bias appeared unlikely and the BARMER cohort was comparable to other European countries in terms of comorbidities, age, and gender. In contrast to clinical registries or administrative data, the BARMER cohort was less affected by selection bias and includes all age groups, all hospitals, and all medical specialties. However, spatial analyses aiming for regional differences were not feasible in the existing dataset.
Conclusions
In this large-scale retrospective analysis of health insurance claims, we observed a marked decrease of in-hospital admission rates for acute cardiovascular and cerebrovascular emergencies including myocardial infarction, acute limb ischemia, stroke, and transient ischemic attack during the COVID-19 pandemic in Germany. No changes were seen in these patients’ comorbidities and treatment allocations. The underlying root cause for these developments and subsequent implications on patient outcomes warrant further investigation. Public education will be important to contain collateral damage caused by delayed treatment for acute cardiovascular and cerebrovascular diseases.
References
Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global health concern. Lancet 395(10223):470–473. https://doi.org/10.1016/S0140-6736(20)30185-9
Melissano G, Mascia D, Baccellieri D, Kahlberg A, Bertoglio L, Rinaldi E, Chiesa R (2020) Pattern of vascular disease in Lombardy, Italy, during the first month of the COVID-19 outbreak. J Vasc Surg 72(1):4–5. https://doi.org/10.1016/j.jvs.2020.04.481
Bashir M, Moughal S (2020) Cardiovascular disease and surgery amid COVID-19 pandemic. J Vasc Surg. https://doi.org/10.1016/j.jvs.2020.04.479
Ng JJ, Ho P, Dharmaraj RB, Wong JCL, Choong A (2020) The global impact of COVID-19 on vascular surgical services. J Vasc Surg 71(6):2182–2183 e2181. https://doi.org/10.1016/j.jvs.2020.03.024
Corrales-Medina VF, Madjid M, Musher DM (2010) Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis 10(2):83–92. https://doi.org/10.1016/S1473-3099(09)70331-7
Kwong JC, Schwartz KL, Campitelli MA (2018) Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 378(26):2540–2541. https://doi.org/10.1056/NEJMc1805679
Bellosta R, Luzzani L, Natalini G, Pegorer MA, Attisani L, Cossu LG, Ferrandina C, Fossati A, Conti E, Bush RL, Piffaretti G (2020) Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. https://doi.org/10.1016/j.jvs.2020.04.483
Kansagra AP, Goyal MS, Hamilton S, Albers GW (2020) Collateral effect of covid-19 on stroke evaluation in the United States. N Engl J Med. https://doi.org/10.1056/NEJMc2014816
Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD (2020) Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 75(22):2871–2872. https://doi.org/10.1016/j.jacc.2020.04.011
Mestres G, Puigmacia R, Blanco C, Yugueros X, Esturrica M, Riambau V (2020) Risk of peripheral arterial thrombosis in COVID-19. J Vasc Surg. https://doi.org/10.1016/j.jvs.2020.04.477
Piccolo R, Bruzzese D, Mauro C, Aloia A, Baldi C, Boccalatte M, Bottiglieri G, Briguori C, Caiazzo G, Calabro P, Cappelli-Bigazzi M, De Simone C, Di Lorenzo E, Golino P, Monda V, Perrotta R, Quaranta G, Russolillo E, Scherillo M, Tesorio T, Tuccillo B, Valva G, Villari B, Tarantini G, Varricchio A, Esposito G, Collaborators (2020) Population trends in rates of percutaneous coronary revascularization for acute coronary syndromes associated with the COVID-19 outbreak. Circulation 141(24):2035–2037. https://doi.org/10.1161/CIRCULATIONAHA.120.047457
De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L, Iannaccone M, Galvani M, Ugo F, Barbero U, Infantino V, Olivotti L, Mennuni M, Gili S, Infusino F, Vercellino M, Zucchetti O, Casella G, Giammaria M, Boccuzzi G, Tolomeo P, Doronzo B, Senatore G, Grosso Marra W, Rognoni A, Trabattoni D, Franchin L, Borin A, Bruno F, Galluzzo A, Gambino A, Nicolino A, Truffa Giachet A, Sardella G, Fedele F, Monticone S, Montefusco A, Omede P, Pennone M, Patti G, Mancone M, De Ferrari GM (2020) Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. https://doi.org/10.1056/NEJMc2009166
Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ (2020) Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 41(19):1852–1853. https://doi.org/10.1093/eurheartj/ehaa314
De Rosa S, Spaccarotella C, Basso C, Calabro MP, Curcio A, Filardi PP, Mancone M, Mercuro G, Muscoli S, Nodari S, Pedrinelli R, Sinagra G, Indolfi C, Societa Italiana di C, the CCUAig (2020) Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 41(22):2083–2088. https://doi.org/10.1093/eurheartj/ehaa409
Enache B, Claessens YE, Boulay F, Dor V, Eker A, Civaia F, Pathak A (2020) Reduction in cardiovascular emergency admissions in Monaco during the COVID-19 pandemic. Clin Res Cardiol. https://doi.org/10.1007/s00392-020-01687-w
Settelmeier S, Rassaf T, Giannitsis E, Münzel T, Breuckmann F (2020) Capacity changes in German certified chest pain units during COVID-19 outbreak response. Clin Res Cardiol. https://doi.org/10.1007/s00392-020-01676-z(in press)
van Camp G, de Beenhouwer H, Beles M, Collet C, Nasser R, Schelfaut D et al (2020) Disturbing effect of lockdown for COVID-19 on the incidence of infective endocarditis: a word of caution. Clin Res Cardiol. https://doi.org/10.1007/s00392-020-01686-x(in press)
Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL et al (2020) Declines in hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic: a multicenter tertiary care experience. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2020.05.038(in press)
Rattka M, Baumhardt M, Dreyhaupt J, Rothenbacher D, Thiessen K, Markovic S et al (2020) 31 days of COVID-19-cardiac events during restriction of public life-a comparative study. Clin Res Cardiol. https://doi.org/10.1007/s00392-020-01681-2 (in press)
Kreutzburg T, Peters F, Riess HC, Hischke S, Marschall U, Kriston L, L'Hoest H, Sedrakyan A, Debus ES, Behrendt CA (2020) Editor's choice-comorbidity patterns among patients with peripheral arterial occlusive disease in Germany: a trend analysis of health insurance claims data. Eur J Vasc Endovasc Surg 59(1):59–66. https://doi.org/10.1016/j.ejvs.2019.08.006
Behrendt CA, Sedrakyan A, Peters F, Kreutzburg T, Schermerhorn M, Bertges DJ, Larena-Avellaneda A, L'Hoest H, Kolbel T, Debus ES (2020) Editor's choice - long term survival after femoropopliteal artery revascularisation with paclitaxel coated devices: a propensity score matched cohort analysis. Eur J Vasc Endovasc Surg 59(4):587–596. https://doi.org/10.1016/j.ejvs.2019.12.034
Czwikla J, Jobski K, Schink T (2017) The impact of the lookback period and definition of confirmatory events on the identification of incident cancer cases in administrative data. BMC Med Res Methodol 17(1):122. https://doi.org/10.1186/s12874-017-0407-4
Ohlmeier C, Langner I, Hillebrand K, Schmedt N, Mikolajczyk R, Riedel O, Garbe E (2015) Mortality in the German Pharmacoepidemiological Research Database (GePaRD) compared to national data in Germany: results from a validation study. BMC Public Health 15:570. https://doi.org/10.1186/s12889-015-1943-7
Tsioufis K, Chrysohoou C, Kariori M, Leontsinis I, Dalakouras I, Papanikolaou A, Charalambus G, Sambatakou H, Siassos G, Panagiotakos D, Tousoulis D (2020) The mystery of "missing" visits in an emergency cardiology department, in the era of COVID-19; a time-series analysis in a tertiary Greek General Hospital. Clin Res Cardiol. https://doi.org/10.1007/s00392-020-01682-1
Range G, Hakim R, Motreff P (2020) Where have the STEMIs gone during COVID-19 lockdown? Eur Heart J Qual Care Clin Outcomes. https://doi.org/10.1093/ehjqcco/qcaa034
Sena G, Gallelli G (2020) An increased severity of peripheral arterial disease in the COVID-19 era. J Vasc Surg. https://doi.org/10.1016/j.jvs.2020.04.489
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P, Group ESCSD (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39(2):119–177. https://doi.org/10.1093/eurheartj/ehx393
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW, American College of Cardiology Foundation, American Heart Association Task Force on Practice G (2013) 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 127(4):e362–425. https://doi.org/10.1161/CIR.0b013e3182742cf6
Chieffo A, Stefanini GG, Price S, Barbato E, Tarantini G, Karam N, Moreno R, Buchanan GL, Gilard M, Halvorsen S, Huber K, James S, Neumann FJ, Mollmann H, Roffi M, Tavazzi G, Mauri Ferre J, Windecker S, Dudek D, Baumbach A (2020) EAPCI position statement on invasive management of acute coronary syndromes during the COVID-19 pandemic. Eur Heart J 41(19):1839–1851. https://doi.org/10.1093/eurheartj/ehaa381
Bohm M, Frey N, Giannitsis E, Sliwa K, Zeiher AM (2020) Coronavirus Disease 2019 (COVID-19) and its implications for cardiovascular care: expert document from the German Cardiac Society and the World Heart Federation. Clin Res Cardiol. https://doi.org/10.1007/s00392-020-01656-3
Acknowledgment
Open Access funding provided by Projekt DEAL.
Funding
This work was not funded.
Author information
Authors and Affiliations
Contributions
Contributor Roles Taxonomy CRediT Statement: MS: conceptualization, methodology, validation, investigation, writing—original draft, writing—review and editing, visualization, project administration, supervision. FB: conceptualization, methodology, validation, investigation, writing—original draft, writing—review and editing, visualization, project administration, supervision. MR: conceptualization, validation, investigation, writing—original draft, writing—review and editing. GT: writing—review and editing. UM: formal analysis, validation, data curation, writing—review and editing. HL: formal analysis, validation, data curation, writing—review and editing. LA: formal analysis, validation, data curation, writing—review and editing. SD: writing—review and editing. SB: writing—review and editing. CG: writing—review and editing. CAB: conceptualization, methodology, validation, formal analysis, investigation, writing—original draft, writing—review and editing, visualization, project administration, supervision.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Seiffert reports non-financial support from Abbott Vascular, personal fees from Abiomed, personal fees from AstraZeneca, personal fees from Bayer Healthcare, non-financial support from Biotronik, personal fees from Boehringer Ingelheim, personal fees and non-financial support from Boston Scientific, personal fees from Bristol-Myers Squibb, non-financial support from Edwards Lifesciences, non-financial support from Nicolai Medizintechnik, non-financial support from OrbusNeich Medical, grants and personal fees from Philips, and personal fees from Medtronic outside the submitted work. Dr. Brunner reports grant from the ASPIRE Cardiovascular grant award, Pfizer, outside the submitted work. Dr. Thomalla has received reports grant support and lecture fees from Bayer, personal fees from Acandis, Boehringer Ingelheim, Bristol-Myers Squibb/Pfizer, and Daiichi Sankyo, Portola, and Stryker outside the submitted work. Dr. Gerloff reports personal fees from Amgen, Bayer Vital, Bristol-Myers Squibb, Boehringer Ingelheim, Sanofi Aventis, Abbott, and Prediction Biosciences outside the submitted work. Dr. Behrendt and Dr. Debus report grants from the German Federal Joint Committee and grants from German Stifterverband outside the submitted work. The other authors declare no conflicts of interest.
Ethics approval
Several review boards have determined that using anonymized data from claims or national statistics retrospectively is not human subject research because de-identified datasets were used.
Consent to participate
All analyses were following the European Union General Data Privacy Regulation (EU-GDPR), considering the theoretical concept of k-anonymity. Thus, patient informed consent was not obtained for this retrospective secondary data analysis [31].
Availability of data and material (data transparency)
The data will be shared on reasonable request to the corresponding author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seiffert, M., Brunner, F.J., Remmel, M. et al. Temporal trends in the presentation of cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany: an analysis of health insurance claims. Clin Res Cardiol 109, 1540–1548 (2020). https://doi.org/10.1007/s00392-020-01723-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01723-9