Abstract
Aims: The aim of this meta-analysis was to appraise the burden of cardiovascular mortality and morbidity among patients undergoing percutaneous coronary intervention (PCI) after out-of-hospital cardiac arrest (OHCA).
Methods and results: This was a meta-analysis of studies assessing the cardiovascular mortality or at least one other pre-defined outcome in OHCA patients undergoing PCI. Forty-nine studies with a total of 301,902 patients (73,634 OHCA and 228,268 non-OHCA patients) were included. Compared to non-OHCA patients, all-cause mortality was higher in OHCA patients (29% vs 4%). The cause of 39% of deaths among OHCA patients was cardiovascular: PCI was more frequently unsuccessful (9.2% vs 7.6%) and there were higher rates of stent thrombosis (2.9% vs 0.8%), myocardial infarction (1.7% vs 1.4%), relevant bleeding (10.2% vs 2.1%) and stroke (1.7% vs 0.5%). OHCA patients compared to non-OHCA patients had a higher risk of all-cause mortality (risk ratio [RR] 6.4, 95% CI: 5.5-7.4), cardiovascular death (4.6, 1.1-19), unsuccessful coronary revascularisation (1.4, 1.1-1.7), stent thrombosis (3.8, 0.6-22.7), myocardial infarction (1.4, 1.1-1.7), relevant bleeding (3.2, 2.5-4.1) and stroke (3.1, 2.3-4.3).
Conclusions: Almost one third of OHCA patients undergoing PCI die and more than one third of the fatalities are attributable to cardiovascular causes. The burden of ischaemic and bleeding complications was consistently higher and the success rates of PCI lower among OHCA as compared to non-OHCA patients.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a leading cause of death in the USA and Europe. The global incidence of emergency medical system (EMS)-attended OHCA is estimated to be 95.9 per 100,000 person-years and the survival rate is about 6%1. Despite advances in the field of resuscitation and intensive care management, acute mortality remains high2. The most frequent cause of in-hospital mortality in OHCA patients is withdrawal of life-sustaining therapy on the basis of poor neurological outcomes. However, it has also been observed that a relevant number of deaths during the initial days after OHCA are caused by persistent unstable haemodynamic conditions3.
Ischaemic coronary artery disease is the leading cause of OHCA and significant coronary lumen narrowing has been documented in more than 70% of patients according to autopsy4 or coronary angiography data5. Current ACC/AHA and ESC guidelines recommend immediate coronary angiography in OHCA patients with ST-elevation myocardial infarction (STEMI)6,7, whereas, in resuscitated patients without STEMI, coronary angiography is recommended in selected patients without overt evidence of a non-cardiac cause6.
Several observational studies and one recent randomised trial8 investigated the impact of coronary angiography and PCI on all-cause mortality in OHCA patients. However, the cause of death (i.e., cardiovascular vs non-cardiovascular) and the prevalence of ischaemic or bleeding events after PCI are less frequently reported, with heterogeneous results among studies. No systematic review and meta-analysis, with the exception of a single small study9, has appraised the prevalence of cardiovascular events and their potential impact on prognosis in OHCA patients. This information would enhance our understanding of this condition and help to develop dedicated management strategies for these patients.
Therefore, we conducted a systematic review and meta-analysis of studies reporting the aforementioned clinical outcomes in OHCA patients undergoing invasive management.
Methods
This study was performed based on a pre-specified protocol, available in PROSPERO (CRD 42019135553). Reporting and assessment are according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement10.
SOURCE OF EVIDENCE AND SEARCH
We performed a broad literature search in PubMed, Embase, and Cochrane Library Central Register of Controlled Trials (CENTRAL) which was concluded on 30 April 2020. Screening was performed in two stages by two investigators (A. Spirito and G. Gargiulo) working independently and in duplicate against a priori eligibility criteria. Search terms and details of the screening process are available in Supplementary Appendix 1.
STUDY INCLUSION
We considered original studies of any design reporting any of the outcomes of interest reported below in an OHCA study population in which at least 70% of patients underwent PCI. The rationale of this cut-off is explained in Supplementary Appendix 1. We excluded studies not reporting disease-specific causes of fatalities unless reporting at least one additional outcome of interest. The presence of a “non-OHCA” comparison group at the study level (patients with acute coronary syndrome but without OHCA undergoing PCI) was systematically screened but was not mandatory for study inclusion. We considered only studies with at least two thirds of patients enrolled after the year 2002 under the rationale that drug-eluting stents (DES) were not available and adoption of oral P2Y12 inhibitors limited until then, thus not reflecting current practice. Additional exclusion criteria are shown in Supplementary Appendix 1.
DATA EXTRACTION AND OUTCOME DEFINITIONS
Data were extracted and summarised at the study level on an Excel spreadsheet for the OHCA and, if present, also for the comparison population (non-OHCA).
The primary outcome of interest was cardiovascular death. Secondary outcomes were all-cause mortality, unsuccessful PCI, stent thrombosis, myocardial infarction, bleeding, stroke and neurological status at discharge. We focused on events which occurred during the index hospitalisation or up to 30 days. For all-cause mortality, we also considered the 6- and 12-month follow-up.
The quality of studies was evaluated according to the Newcastle-Ottawa score. For each study, we also assessed the adherence to 2004 and 2015 Utstein core criteria.
Data extraction and study quality assessment were performed by one reviewer and verification was carried out by a second reviewer. Disagreements among reviewers were resolved through consensus or by third-party adjudication. Items extracted and definitions used for the outcomes are listed in Supplementary Appendix 1.
DATA SYNTHESIS
Summary proportion estimates with 95% confidence intervals (CI) and heterogeneity using a random effects model were obtained separately for OHCA and non-OHCA populations. Moreover, after selecting only studies reporting data for both OHCA and non-OHCA populations, we used a random effects model to calculate summary risk ratios (RR) and heterogeneity for each outcome comparing the two groups. We used the I2 metric to assess the extent of heterogeneity. Among OHCA populations, we evaluated the role of patient and study characteristics by using stratified meta-analyses for the outcome of cardiovascular and all-cause mortality. Further details about data synthesis are provided in Supplementary Appendix 1.
Results
LITERATURE SEARCH AND STUDY SELECTION
We screened 1,618 unique citations. Of these, 400 were judged potentially eligible during screening of titles and abstracts, and 49 deemed eligible after full text review (Figure 1).
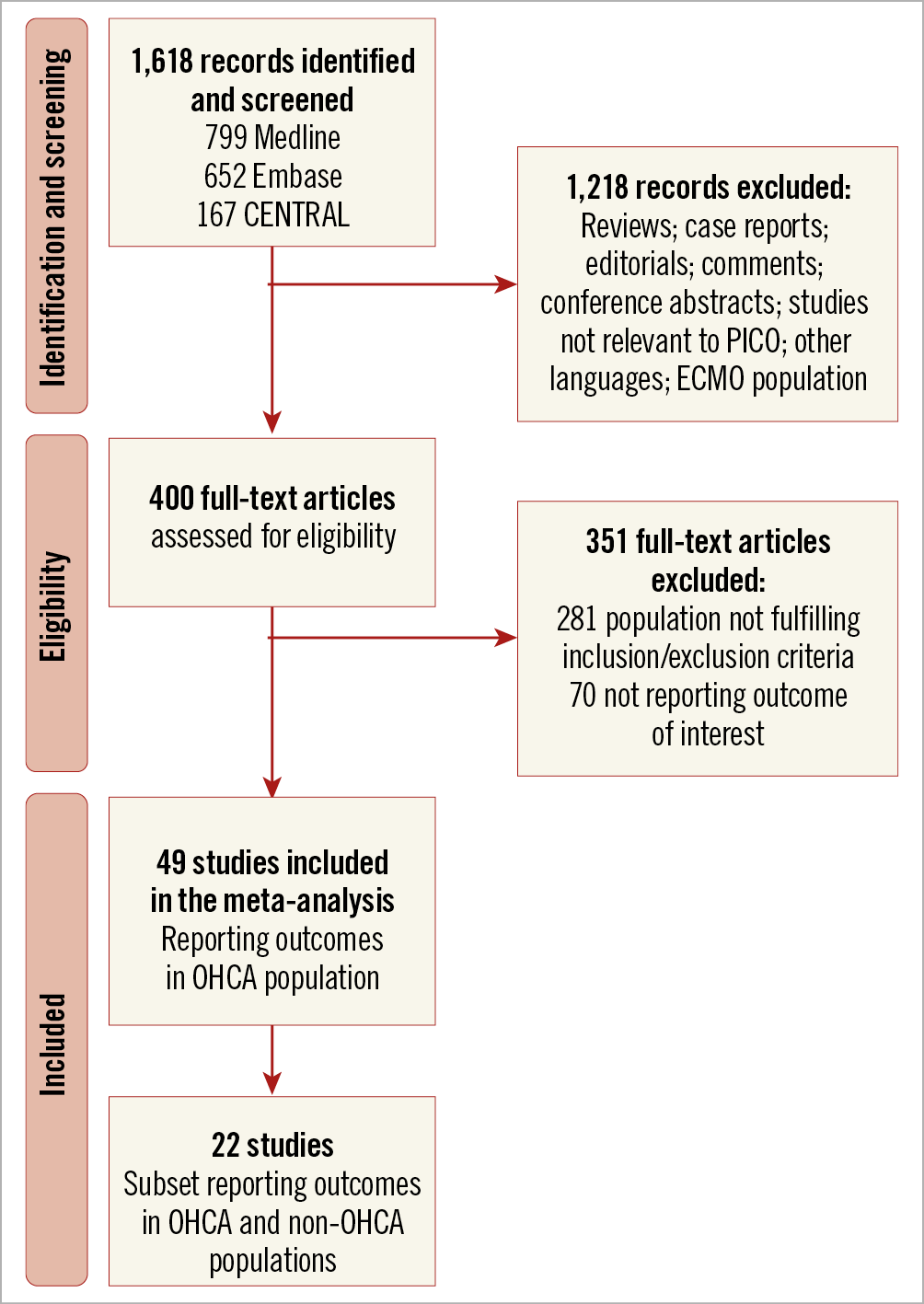
Figure 1. Flow diagram of the selection of the articles for the systematic review and meta-analysis. ECMO: extracorporeal membrane oxygenatio
STUDY CHARACTERISTICS
Among the 49 studies which were published between 2007 and 2020 and included patients from 1997 to 2018, the majority were single-centre (38 studies or 78%), small-scale (34 or 70%), observational (46 or 94%), retrospective (30 or 61%) or conducted in Europe (31 or 63%). According to the Newcastle-Ottawa score, the quality of 25 studies (or 51%) was good (Table 1, Supplementary Table 1).
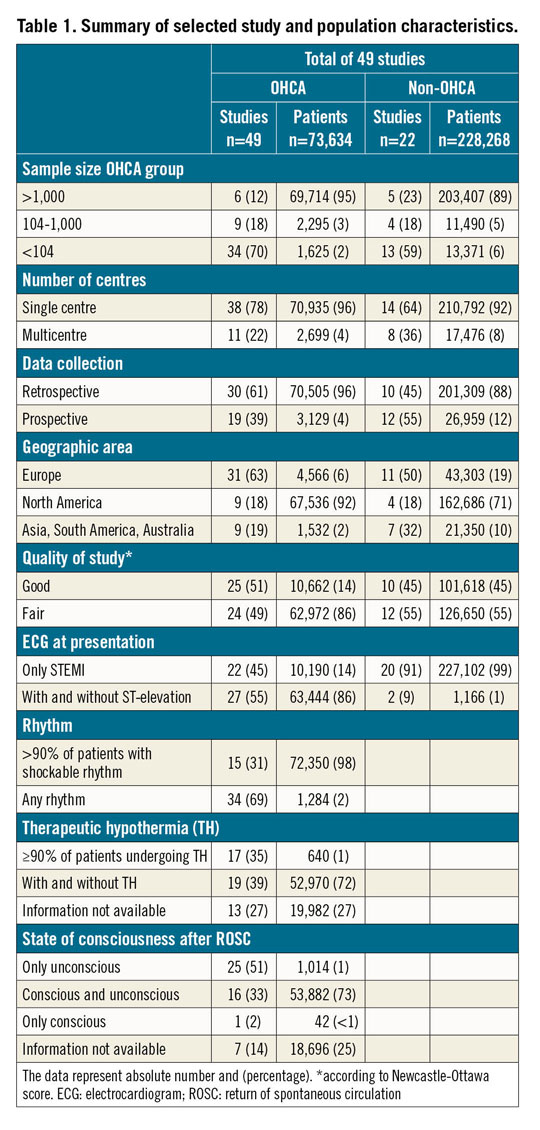
A total of 22 out of 49 studies (45%) had a comparator group, consisting of patients with ACS (restricted to STEMI in 20 studies) without OHCA undergoing invasive management (non-OHCA group) (Supplementary Table 2).
A further description of the study characteristics is available in Supplementary Appendix 2 and Supplementary Table 3.
POPULATION CHARACTERISTICS
A total of 73,634 OHCA patients were included of whom 71,961 (98%) underwent PCI. Age ranged from 54 to 68 years and 52,143 (71%) patients were male. Among the 49 studies, 40 specified the type of ACS at presentation and 85.6% (20,560 out of 24,033) of the patients had STEMI (Table 1).
The comparator group consisted of 228,268 patients of whom 212,450 (93%) underwent PCI. Age ranged from 56 to 75 years, 164,028 (72%) were male and 227,109 patients (99%) had STEMI (Table 1). OHCA patients compared to those without OHCA more frequently suffered from cardiogenic shock (37% vs 6%) and more often received mechanical support (30% vs 8%). In 4,272 (85%) out of 5,038 OHCA patients in whom information on mechanical support was available, intra-aortic balloon pump was the only assist device used.
SHORT-TERM OUTCOMES
MORTALITY
The proportion of all-cause mortality in OHCA patients obtained from 43 studies was 29% (95% confidence interval [CI]: 27% to 32%, I2=94%) as compared to 4% (95% CI: 3% to 4%, I2=97%) in the non-OHCA group (from 18 studies) (Figure 2A, Supplementary Figure 1).
Across the 17 OHCA studies which ascertained causes of mortality, 39% of all fatalities were deemed cardiovascular (95% CI: 24% to 55%, I2=95%) with an absolute cardiovascular death proportion of 12% (95% CI: 7% to 18%, I2=93%).
In 2 out of 17 studies which included a comparison group (n=773 OHCA patients and n=12,507 non-OHCA patients), the proportion of cardiovascular death in the non-OHCA group was 4% (95% CI: 4% to 5%), representing 80% of all fatalities (95% CI: 77% to 83%) (Figure 2A, Figure 2B, Supplementary Figure 2, Supplementary Figure 3). The absolute proportion of cardiovascular death was almost fivefold higher in OHCA than non-OHCA patients (risk ratio [RR] 4.6, 95% CI: 1.1 to 19) (Figure 2C, Supplementary Figure 4).
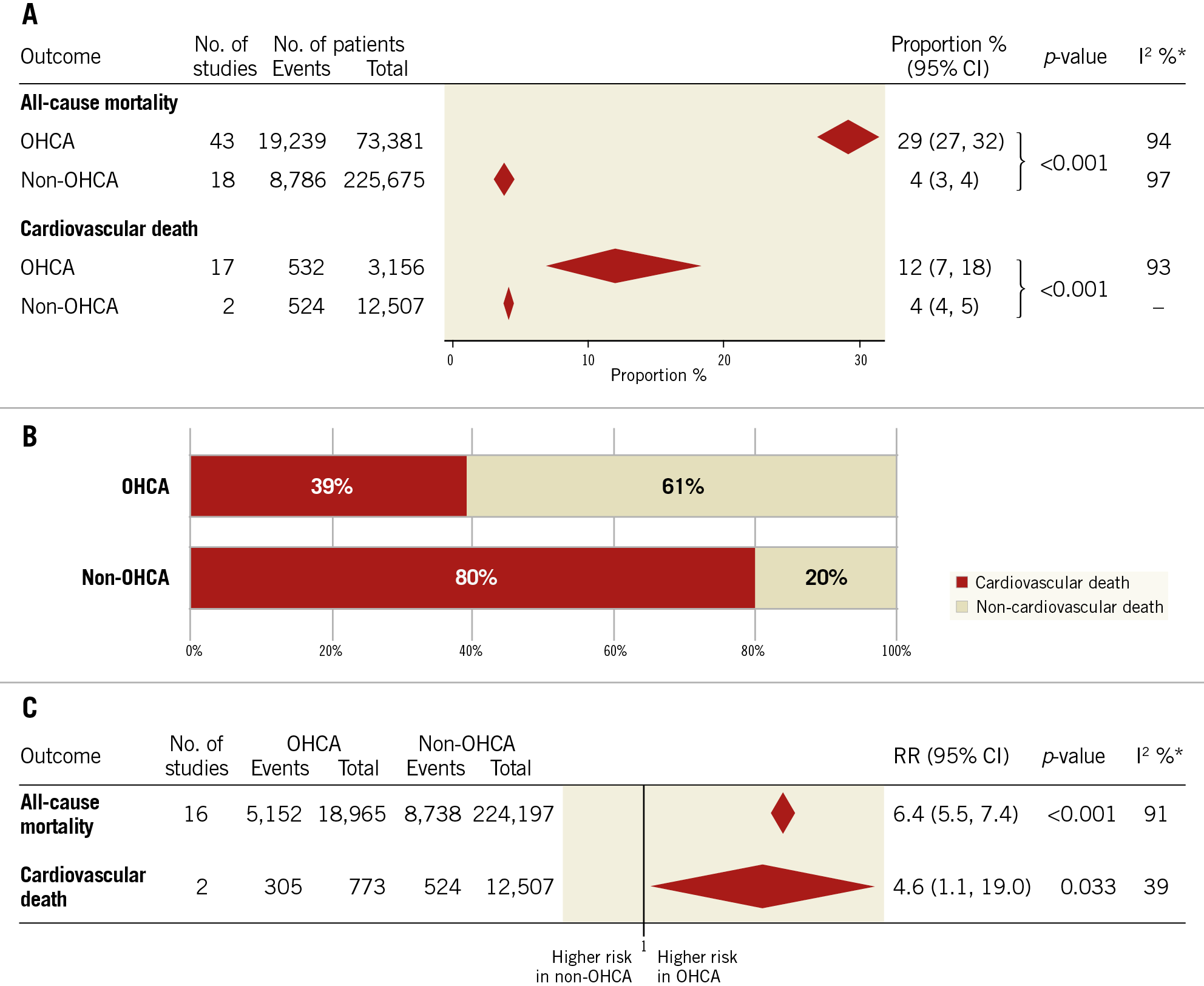
Figure 2. Summary of proportion estimates of all-cause and cardiovascular death (A), proportion of cardiovascular versus non-cardiovascular death (B) and relative risk for all-cause and cardiovascular death (C) in hospital or at 30 days in OHCA compared to non-OHCA patients. *values around 25%, 50% and 75% indicate low, intermediate and high heterogeneity among studies, respectively.
At subgroup analysis we found lower estimated proportions of cardiovascular death in the OHCA population across studies conducted in North America and Europe, with a prospective design or in which more than 50% of patients received a bystander basic life support (Supplementary Figure 5, Supplementary Table 4). Results remained consistent for geographic area when all-cause mortality and cardiovascular mortality relative to all-cause mortality were analysed. The proportion of all-cause mortality was also lower in studies of fair quality, published before 2011, in which ≥90% of patients had witnessed arrest, in those including ≥90% of patients with shockable rhythm or in which <30% of patients presented a cardiogenic shock at admission (Supplementary Figure 6, Supplementary Figure 7, Supplementary Table 4).
PCI AND PROCEDURAL FEATURES
PCI was unsuccessful in 9.2% (95% CI: 7.5% to 11.15%, I2=69%) of the patients with OHCA (across 22 studies) and in 7.6% (95% CI: 6.3% to 9.1%, I2=97%) of the patients without OHCA (out of 12 studies) (Figure 3A, Supplementary Figure 8). Compared to non-OHCA, unsuccessful PCI was 40% more frequent in OHCA patients (RR 1.4, 95% CI: 1.1% to 1.7%) (Figure 3B, Supplementary Figure 4).
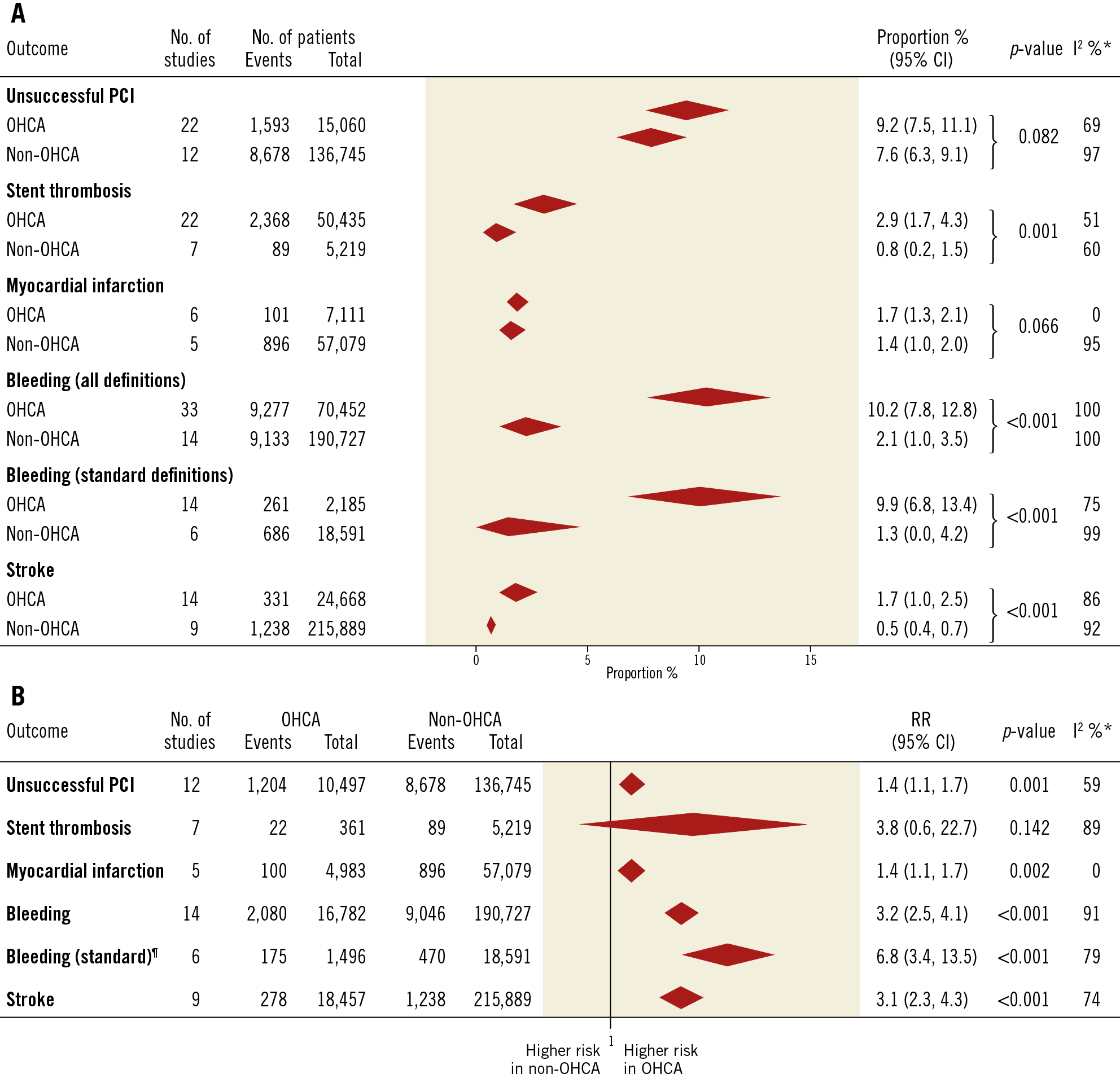
Figure 3. Summary of proportion estimates (A) and relative risk (B) of secondary outcomes in hospital or at 30 days in OHCA compared to non-OHCA patients. ¶only studies using standard bleeding definition (TIMI, GUSTO, BARC). * values around 25%, 50% and 75% indicate low, intermediate and high heterogeneity among studies, respectively.
The culprit vessel, reported for both OHCA and non-OHCA patients in ten studies, was more frequently the left main coronary artery (RR 2.8, 95% CI: 1.8-4.4) or left anterior descending artery (LAD) (RR 1.3, 95% CI: 1.2-1.3) or left circumflex artery (LCX) (RR 1.19, 95% CI: 1.03-1.37) and less frequently the right coronary artery (RCA) (RR 0.6, 95% CI: 0.5-0.7) among OHCA patients. The involvement of a coronary artery bypass conduit and the presence of multivessel disease did not differ between the two groups (Supplementary Figure 9). The use of glycoprotein IIb/IIIa inhibitors, reported in 12/22 and 7/12 studies for OHCA and non-OHCA groups, was 48% and 56%, respectively. The reasons for suboptimal PCI, type of lesion as well as other PCI-related information were largely underreported (Supplementary Table 5).
STENT THROMBOSIS
A total of 2,368 stent thromboses in 50,435 OHCA patients was reported across 22 studies, with a summary proportion estimate of 2.9% (95% CI: 1.70% to 4.3%, I2=51%), whereas, among 5,219 non-OHCA patients from seven studies, stent thrombosis was observed in 89 cases (0.8%; 95% CI: 0.2% to 1.5%, I2=60%) (Figure 3A, Supplementary Figure 10).
Across five studies which provided this information, stent thrombosis was associated with greater but statistically not relevant risk of all-cause mortality among OHCA patients (RR 1.63, 95% CI: 0.97 to 2.73) (Supplementary Figure 11).
IN-HOSPITAL RECURRENT MYOCARDIAL INFARCTION
Reinfarction during index hospitalisation occurred in 107 out of 5,050 OHCA patients (nine studies) and in 896 out of 57,079 non-OHCA patients (five studies), providing a summary proportion estimate of 1.4% in both populations (Supplementary Figure 12). After exclusion of stent thrombosis-related myocardial infarction, the summary proportion was 1.7% in the OHCA group with a risk ratio of 1.4 (95% CI: 1.1 to 1.7) compared with non-OHCA patients (Figure 3B, Supplementary Figure 4).
BLEEDING RATES
In-hospital severe or relevant bleeding was reported in 9,277 out of 70,452 OHCA patients across 33 studies with a cumulative proportion of 10% (95% CI: 8% to 13%, I2=100%) and in 9,133 out of 190,727 non-OHCA patients, leading to a summary proportion of 2% (95% CI: 1% to 4%, I2=100%) from 14 studies (Figure 3A, Supplementary Figure 13).
The proportions of relevant bleeding in OHCA patients appeared consistent across studies adopting standardised (Bleeding Academic Research Consortium [BARC], Thrombolysis In Myocardial Infarction [TIMI] or Global Registry of Acute Coronary Events [GRACE] scales) or study-specific definitions (Supplementary Figure 13).
When considering only studies presenting a comparison group, we observed a threefold risk increase of severe or relevant bleeding in OHCA versus non-OHCA patients (RR 3.2, 95% CI: 2.5 to 4.1) and a sevenfold increase if the analysis is limited to the six studies that adopted standardised definitions (Figure 3B, Supplementary Figure 4).
STROKE
In OHCA patients 331/24,668 and in non-OHCA patients 1,238/215,889 had a stroke; the summary proportion estimates were 1.7% (95% CI: 1.0% to 2.5%, I2=86%) and 0.5% (95% CI: 0.4% to 0.7%, I2=92%), respectively (Figure 3A, Supplementary Figure 14), with an estimated relative risk in OHCA versus non-OHCA patients of 3.1 (95% CI: 2.3 to 4.3) (Figure 3B, Supplementary Figure 4).
NEUROLOGICAL OUTCOMES IN OHCA PATIENTS
Across 20 studies, a poor neurological outcome was observed in 230 out of 1,355 OHCA patients alive at discharge (19%; 95% CI: 14% to 25%, I2=82%) and it was significantly lower in studies in which the assessment was carried out at one year (10%; 95% CI: 6% to 17%), instead of at discharge or at six months (Supplementary Figure 15) .
SIX- AND TWELVE-MONTH FOLLOW-UP
Among patients discharged alive, all-cause mortality at six months was 5.5% (95% CI: 1.6% to 10.9%, I2=30%) for OHCA patients and 1.9% (95% CI: 1.4% to 2.5%) for non-OHCA patients; at 12-month follow-up it was 6.9% (95% CI: 3.7% to 10.8%, I2=58%) for OHCA patients and 3.1% (95% CI: 2.3% to 3.9%, I2=79%) for non-OHCA patients (Supplementary Figure 16). If considering only studies with a comparison group, OHCA patients had a 2.5-fold (95% CI: 0.9 to 6.6) higher risk of death at six months and 1.8-fold (95% CI: 1.01 to 3.34) higher risk at 12 months (Supplementary Figure 17).
REPORTING OF UTSTEIN CORE CRITERIA
Adherence to 2004 or updated 2015 Utstein core criteria for reporting was generally poor (Supplementary Table 6, Supplementary Appendix 2).
Discussion
The salient findings of this systematic review and meta-analysis involving 73,634 OHCA patients who underwent PCI, and 228,268 control patients with ACS but without cardiac arrest, can be summarised as follows:
1. Cardiovascular death occurs almost five times more frequently in OHCA patients and it accounts for 39% of in-hospital fatalities.
2. All-cause mortality was 29% in OHCA and 4% in non-OHCA patients; among OHCA patients who survived to discharge, 19% had a poor neurological outcome.
3. PCI in OHCA patients was more frequently unsuccessful; the culprit lesions appeared more frequently located in the left coronary artery in OHCA as compared to non-OHCA patients, whereas the prevalence of multivessel disease was similar.
4. OHCA patients have higher in-hospital proportions of bleeding and ischaemic events, including myocardial infarction, stent thrombosis and stroke.
5. Adherence to the original or updated Utstein criteria for standardised reporting was generally poor across studies.
The aetiology of OHCA is heterogeneous, but coronary artery disease remains the predominant cause. We focused on patients with OHCA who underwent PCI because we wanted to restrict the analysis to patients in whom the aetiology of OHCA was deemed cardiac. Cardiovascular death had an absolute incidence of 12% and a cardiovascular cause was responsible for 39% of deaths in OHCA patients. Cardiovascular together with all-cause mortality varied greatly across selected studies (from 0 to 55% and from 7 to 77%, respectively). The selection of patients with favourable prognosis (e.g., witnessed arrest, bystander cardiopulmonary resuscitation, shockable rhythm, undergoing therapeutic hypothermia) greatly influences mortality and explains the heterogeneity observed. This notion was confirmed in the subgroup analysis.
Our meta-analysis confirmed the high prevalence of cardiogenic shock in OHCA patients, which was six times higher than in non-OHCA patients. The most frequent measure of mechanical support was by far intra-aortic balloon pump (IABP); however, this information was largely underreported across included studies. In a randomised study of patients in cardiogenic shock, in which 40% suffered cardiac arrest but did not require prolonged resuscitation, systematic use of IABP did not demonstrate a reduction in mortality11. Other forms of mechanical support such as extracorporeal membrane oxygenation (ECMO) or Impella® (Abiomed, Danvers, MA, USA) are being investigated12,13.
Successful and prompt myocardial revascularisation remains the only evidence-based treatment to mitigate fatality risk in patients with shock and ongoing myocardial ischaemia6. Instead, in haemodynamically stable OHCA patients without ST-elevation on ECG, a recent randomised controlled trial did not show any benefit of an early versus delayed invasive strategy8.
Among OHCA patients, compared to non-OHCA patients, the rate of successful PCI was lower and recurrent myocardial infarction or the occurrence of ST was higher. The broad confidence intervals of risk ratio obtained for stent thrombosis are attributable to the limited number of studies included in this analysis (7 out of 22). Our results showed a trend towards increased mortality for patients experiencing a stent thrombosis.
Oral P2Y12 inhibitors show delayed onset and attenuated antiplatelet effects among STEMI patients14,15 as well as OHCA patients16,17. At variance with ACS patients without OHCA18,19, in the OHCA population the benefit derived from the use of newer P2Y12 inhibitors such as prasugrel or ticagrelor is less clear9. While the use of parenteral antiplatelet agents may be conceptually appealing to overcome the delay in platelet inhibition15,20,21, our meta-analysis raises concerns about the liberal use of potent antithrombotic agents in OHCA patients, due to a threefold higher prevalence of relevant bleeding in this population.
We observed that fatality rates remained higher at 12-month follow-up among OHCA as compared to non-OHCA patients. However, this observation is hampered by the limited number of studies reporting mortality rates after hospital discharge.
Finally, our meta-analysis showed a poor adherence to Utstein core criteria across included studies and reinforces the need for standardised reporting and use of validated outcome definitions.
Limitations
The different selection of patients and outcome definitions across studies explain the high degree of heterogeneity observed for almost all clinical endpoints. Moreover, we observed a certain degree of heterogeneity in follow-up length. We tried to overcome these problems by performing a subgroup analysis and stratifying by selection criteria and outcome definition whenever possible. Some thresholds applied in the subgroup meta-analysis were arbitrary, but the results remained consistent if different thresholds were applied. The lack of individual patient data and the absence or underreporting of some important data across studies prevented subgroup analysis of interest (e.g., STEMI vs no-STEMI). The comparison of summary proportion estimates obtained from a different pool of studies for OHCA and non-OHCA populations has to be considered only exploratory. The risk ratio analysis is affected by potential confounders as well, because of the absence of propensity score matching in almost all studies with a comparison group. However, the results obtained with the two methods (proportion meta-analysis and classic meta-analysis) were largely consistent and showed remarkable differences between OHCA and non-OHCA patients. As we selected only OHCA patients undergoing PCI, the results are applicable only to this subgroup of OHCA patients.
Conclusions
Almost one third of OHCA patients undergoing PCI die and more than one third of the fatalities are attributable to cardiovascular causes. In addition, the burden of ischaemic and bleeding complications is consistently higher and the success rates of percutaneous intervention lower among OHCA as compared to non-OHCA patients. Our meta-analysis reinforces the need for high-quality studies adhering to previously proposed standardised criteria for reporting (e.g., Utstein criteria) and suggests the need to investigate new therapeutic strategies affecting neurological but also cardiovascular mortality and morbidity burden in OHCA patients undergoing PCI.
|
Impact on daily practice More than one third of the fatalities in OHCA patients undergoing coronary revascularisation are attributable to cardiovascular causes, and the burden of cardiovascular ischaemic and bleeding complications is remarkably higher compared to non-OHCA patients. Dedicated treatment strategies aimed at reducing ischaemic and bleeding risks in this vulnerable and so far largely neglected population are warranted in clinical practice and future clinical studies. |
Conflict of interest statement
G. Gargiulo reports personal fees from Daiichi Sankyo, outside the submitted work. M. Valgimigli reports personal fees/grants from AstraZeneca, Terumo, Abbott Vascular, Alvimedica/CLD, Daiichi Sankyo, Opsens, Bayer, CoreFlow, Idorsia Pharmaceuticals Ltd, Universität Basel, Dept. Klinische Forschung, Vifor, Bristol-Myers Squibb SA, iVascular and Medscape, outside the submitted work. S. Windecker reports grants from Amgen, Abbott, Biotronik, Boston Scientific, Bayer, BMS, CSL Behring, Edwards Lifesciences, Medtronic, Polares and Sinomed, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.