Abstract
Background
Currently, patient selection in TAVI is based upon a multidisciplinary heart team assessment of patient comorbidities and surgical risk stratification. In an era of increasing need for precision medicine and quickly expanding TAVI indications, machine learning has shown promise in making accurate predictions of clinical outcomes. This study aims to predict different intrahospital clinical outcomes in patients undergoing TAVI using a machine learning-based approach. The main clinical outcomes include all-cause mortality, stroke, major vascular complications, paravalvular leakage, and new pacemaker implantations.
Methods and results
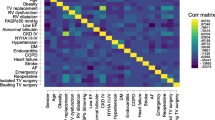
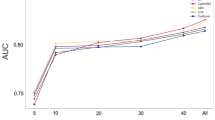
The dataset consists of 451 consecutive patients undergoing elective TAVI between February 2014 and June 2016. The applied machine learning methods were neural networks, support vector machines, and random forests. Their performance was evaluated using five-fold nested cross-validation. Considering all 83 features, the performance of all machine learning models in predicting all-cause intrahospital mortality (AUC 0.94–0.97) was significantly higher than both the STS risk score (AUC 0.64), the STS/ACC TAVR score (AUC 0.65), and all machine learning models using baseline characteristics only (AUC 0.72–0.82). Using an extreme boosting gradient, baseline troponin T was found to be the most important feature among all input variables. Overall, after feature selection, there was a slightly inferior performance. Stroke, major vascular complications, paravalvular leakage, and new pacemaker implantations could not be accurately predicted.
Conclusions
Machine learning has the potential to improve patient selection and risk management of interventional cardiovascular procedures, as it is capable of making superior predictions compared to current logistic risk scores.



Similar content being viewed by others
References
O'Brien SM, Shahian DM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP (2009) The society of thoracic surgeons 2008 cardiac surgery risk models: part 2—isolated valve surgery. Ann Thorac Surg 88(1 Suppl):S23–42. https://doi.org/10.1016/j.athoracsur.2009.05.056
Alvarez-Covarrubias HA, Xhepa E, Michel JM, Kasel AM (2019) Two birds with one stone: transcatheter valve-in-valve treatment of a failed surgical bioprosthesis with concomitant severe stenosis and paravalvular leak. Clin Res Cardiol Off J German Cardiac Soc 108(10):1069–1073. https://doi.org/10.1007/s00392-019-01519-6
Blumenstein J, Mollmann H, Bleiziffer S, Bauer T, Ensminger S, Bekeredjian R, Walther T, Frerker C, Beyersdorf F, Hamm C, Beckmann A (2020) Transcatheter aortic valve implantation in nonagenarians: insights from the german aortic valve registry (GARY). Clin Res Cardiol Off J German Cardiac Soc. https://doi.org/10.1007/s00392-020-01601-4
Doenst T, Bargenda S, Kirov H, Moschovas A, Tkebuchava S, Safarov R, Diab M, Faerber G (2019) Cardiac surgery 2018 reviewed. Clin Res Cardiol Off J German Cardiac Soc 108(9):974–989. https://doi.org/10.1007/s00392-019-01470-6
Droppa M, Borst O, Katzenberger T, Krause R, Bramlage K, Bramlage P, Lausberg HF, Schlensak C, Grasshoff C, Gawaz M, Geisler T (2019) Clinical and economical impact of the presence of an extended heart team throughout the balloon-expandable transcatheter aortic valve implantation procedure. Clin Res Cardiol Off J German Cardiac Soc 108(3):315–323. https://doi.org/10.1007/s00392-018-1359-3
Ebner M, Kresoja KP, Keller K, Hobohm L, Rogge NIJ, Hasenfuss G, Pieske B, Konstantinides SV, Lankeit M (2020) Temporal trends in management and outcome of pulmonary embolism: a single-centre experience. Clin Res Cardiol Off J German Cardiac Soc 109(1):67–77. https://doi.org/10.1007/s00392-019-01489-9
Frank D, Abdel-Wahab M, Gilard M, Digne F, Souteyrand G, Caussin C, Collart F, Letocart V, Wohrle J, Kuhn C, Hovorka T, Baumgartner H (2019) Characteristics and outcomes of patients ≤75 years who underwent transcatheter aortic valve implantation: insights from the SOURCE 3 Registry. Clin Res Cardiol Off J German Cardiac Soc 108(7):763–771. https://doi.org/10.1007/s00392-018-1404-2
Gaede L, Blumenstein J, Liebetrau C, Dorr O, Kim WK, Nef H, Husser O, Gulker J, Elsasser A, Hamm CW, Achenbach S, Mollmann H (2020) Transvascular transcatheter aortic valve implantation in 2017. Clin Res Cardiol Off J German Cardiac Soc 109(3):303–314. https://doi.org/10.1007/s00392-019-01509-8
Kim WK, Hamm CW (2018) Transcatheter aortic valve implantation in Germany. Clin Res Cardiol Off J German Cardiac Soc 107(Suppl 2):81–87. https://doi.org/10.1007/s00392-018-1297-0
Kochman J, Zbronski K, Koltowski L, Parma R, Ochala A, Huczek Z, Rymuza B, Wilimski R, Dabrowski M, Witkowski A, Scislo P, Grygier M, Lesiak M, Opolski G (2020) Transcatheter aortic valve implantation in patients with bicuspid aortic valve stenosis utilizing the next-generation fully retrievable and repositionable valve system: mid-term results from a prospective multicentre registry. Clin Res Cardiol Off J German Cardiac Soc 109(5):570–580. https://doi.org/10.1007/s00392-019-01541-8
Pellegrini C, Rheude T, Trenkwalder T, Mayr NP, Joner M, Kastrati A, Schunkert H, Husser O, Hengstenberg C (2019) One year VARC-2-defined clinical outcomes after transcatheter aortic valve implantation with the SAPIEN 3. Clin Res Cardiol Off J German Cardiac Soc 108(11):1258–1265. https://doi.org/10.1007/s00392-019-01461-7
Shameer K, Johnson KW, Glicksberg BS, Dudley JT, Sengupta PP (2018) Machine learning in cardiovascular medicine: are we there yet? Heart 104(14):1156–1164. https://doi.org/10.1136/heartjnl-2017-311198
Meder B, Radke P (2019) Digital Cardiology. Dtsch Med Wochenschr 144(7):447–451. https://doi.org/10.1055/a-0740-8631
Baumann S, Hirt M, Schoepf UJ, Rutsch M, Tesche C, Renker M, Golden JW, Buss SJ, Becher T, Bojara W, Weiss C, Papavassiliu T, Akin I, Borggrefe M, Schoenberg SO, Haubenreisser H, Overhoff D, Lossnitzer D (2019) Correlation of machine learning computed tomography-based fractional flow reserve with instantaneous wave free ratio to detect hemodynamically significant coronary stenosis. Clin Res Cardiol Off J German Cardiac Soc. https://doi.org/10.1007/s00392-019-01562-3
Ferreira JP, Pizard A, Machu JL, Bresso E, Rocca HB, Girerd N, Leroy C, Gonzalez A, Diez J, Heymans S, Devignes MD, Rossignol P, Zannad F (2020) Plasma protein biomarkers and their association with mutually exclusive cardiovascular phenotypes: the FIBRO-TARGETS case–control analyses. Clin Res Cardiol Off J German Cardiac Soc 109(1):22–33. https://doi.org/10.1007/s00392-019-01480-4
Frangieh AH, Michel J, Deutsch O, Joner M, Pellegrini C, Rheude T, Bleiziffer S, Kasel AM (2019) Aortic annulus sizing in stenotic bicommissural non-raphe-type bicuspid aortic valves: reconstructing a three-dimensional structure using only two hinge points. Clin Res Cardiol Off J German Cardiac Soc 108(1):6–15. https://doi.org/10.1007/s00392-018-1295-2
Kappetein AP, Head SJ, Genereux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es GA, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodes-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB (2013) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the valve academic research consortium-2 consensus document. J Thorac Cardiovasc Surg 145(1):6–23. https://doi.org/10.1016/j.jtcvs.2012.09.002
Friedman JH (2001) Greedy function approximation: a gradient boosting machine. Ann Statist 29(5):1189–1232
Hastie T, Tibshirani R, Friedman J (2008) The elements of statistical learning, 2nd edn. California, Stanford
Jung A (2019) Machine learning: basic principles. arXiv:180505052v11
Goodfellow IB, Bengio Y, Courville A (2016) Deep learning. MIT Press, USA
Breiman L (2016) Random forests. Mach Learn 45(1):5–32
Steinwart I, Christmann A (2008) Support vector machines. Springer-Verlag, New York
Masino AJ, Harris MC, Forsyth D, Ostapenko S, Srinivasan L, Bonafide CP, Balamuth F, Schmatz M, Grundmeier RW (2019) Machine learning models for early sepsis recognition in the neonatal intensive care unit using readily available electronic health record data. PLoS ONE 14(2):e0212665. https://doi.org/10.1371/journal.pone.0212665
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Python Software Foundation. Python Language Reference, version 3.6. Available at https://www.python.org.
Gomes B, Geis NA, Chorianopoulos E, Meder B, Leuschner F, Katus HA, Bekeredjian R (2016) Improvements of procedural results with a new-generation self-expanding transfemoral aortic valve prosthesis in comparison to the old-generation device. J Interv Cardiol. https://doi.org/10.1111/joic.12356
Wendler O, Schymik G, Treede H, Baumgartner H, Dumonteil N, Ihlberg L, Neumann FJ, Tarantini G, Zamarano JL, Vahanian A (2017) SOURCE 3 registry: design and 30-day results of the european postapproval registry of the latest generation of the SAPIEN 3 transcatheter heart valve. Circulation 135(12):1123–1132. https://doi.org/10.1161/circulationaha.116.025103
Lopes RR, van Mourik MS, Schaft EV, Ramos LA, Baan J Jr, Vendrik J, de Mol B, Vis MM, Marquering HA (2019) Value of machine learning in predicting TAVI outcomes. Neth Heart J Monthly J Neth Soc Cardiol the Neth Heart Found 27(9):443–450. https://doi.org/10.1007/s12471-019-1285-7
Hernandez-Suarez DF, Kim Y, Villablanca P, Gupta T, Wiley J, Nieves-Rodriguez BG, Rodriguez-Maldonado J, Feliu Maldonado R, da Luz SI, Sanina C, Cox-Alomar P, Ramakrishna H, Lopez-Candales A, O'Neill WW, Pinto DS, Latib A, Roche-Lima A (2019) Machine learning prediction models for in-hospital mortality after transcatheter aortic valve replacement. JACC Cardiovasc Interv 12(14):1328–1338. https://doi.org/10.1016/j.jcin.2019.06.013
Hein M, Minners J, Jander N, Breitbart P, Stratz C, Pache G, Neumann FJ, Ruile P (2019) Haemodynamic prosthetic valve performance in patients with early leaflet thrombosis after transcatheter aortic valve implantation. Clin Res Cardiol Off J German Cardiac Soc 108(9):1017–1024. https://doi.org/10.1007/s00392-019-01429-7
Hirschberg K, Reinhart M, Mereles D, Uhlmann L, Andre F, Riffel J, Ochs M, Katus HA (2019) Echocardiographic calcification score in patients with low/intermediate cardiovascular risk. Clin Res Cardiol Off J German Cardiac Soc 108(2):194–202. https://doi.org/10.1007/s00392-018-1343-y
Marino PN, Binda G, Calzaducca E, Panizza A, Ferrari I, Bellacosa I, Ambrosio G (2019) Transcatheter aortic valve replacement acutely improves left ventricular mechanical efficiency in severe aortic stenosis: effects of different phenotypes. Clin Res Cardiol Off J German Cardiac Soc. https://doi.org/10.1007/s00392-019-01570-3
Pilecky D, Vamos M, Bogyi P, Muk B, Stauder D, Racz H, Nyolczas N, Duray GZ, Zacher G, Zima E (2019) Risk of cardiac arrhythmias after electrical accident: a single-center study of 480 patients. Clin Res Cardiol Off J German Cardiac Soc 108(8):901–908. https://doi.org/10.1007/s00392-019-01420-2
Schaefer A, Schirmer J, Schofer N, Schneeberger Y, Deuschl F, Blankenberg S, Reichenspurner H, Conradi L, Schafer U (2019) Transaxillary transcatheter aortic valve implantation utilizing a novel vascular closure device with resorbable collagen material: a feasibility study. Clin Res Cardiol Off J German Cardiac Soc 108(7):779–786. https://doi.org/10.1007/s00392-018-1407-z
Schmidt T, Bohne M, Schluter M, Kitamura M, Wohlmuth P, Schewel D, Schewel J, Schmoeckel M, Kuck KH, Frerker C (2019) The impact of biventricular heart failure on outcomes after transcatheter aortic valve implantation. Clin Res Cardiol Off J German Cardiac Soc 108(7):741–748. https://doi.org/10.1007/s00392-018-1400-6
Seoudy H, Gussefeld N, Frank J, Freitag-Wolf S, Lutter G, Eden M, Rangrez AY, Kuhn C, Frey N, Frank D (2019) Incidence and impact of prosthesis-patient mismatch following transcatheter aortic valve implantation. Clin Res Cardiol Off J German Cardiac Soc 108(6):660–668. https://doi.org/10.1007/s00392-018-1394-0
Stundl A, Shamekhi J, Bernhardt S, Starke M, Al-Kassou B, Weber M, Sedaghat A, Treede H, Grube E, Nickenig G, Werner N, Sinning JM (2019) Fractional flow reserve in patients with coronary artery disease undergoing TAVI: a prospective analysis. Clin Res Cardiol Off J German Cardiac Soc. https://doi.org/10.1007/s00392-019-01563-2
Tabata N, Al-Kassou B, Sugiura A, Kandt J, Shamekhi J, Stundl A, Zimmer S, Treede H, Ishii M, Tsujita K, Nickenig G, Werner N, Sinning JM (2020) Prognostic impact of cancer history in patients undergoing transcatheter aortic valve implantation. Clin Res Cardiol Off J German Cardiac Soc. https://doi.org/10.1007/s00392-020-01615-y
Tabata N, Al-Kassou B, Sugiura A, Shamekhi J, Sedaghat A, Treede H, Tsujita K, Werner N, Grube E, Nickenig G, Sinning JM (2020) Predictive factors and long-term prognosis of transcatheter aortic valve implantation-associated endocarditis. Clin Res Cardiol Off J German Cardiac Soc. https://doi.org/10.1007/s00392-020-01609-w
Krapf S, von Scheidt W, Thilo C (2020) Periprocedural embolisation of a Sapien 3 TAVI prosthesis: failure and success. Clin Res Cardiol Off J German Cardiac Soc 109(5):649–651. https://doi.org/10.1007/s00392-019-01573-0
Testa L, Latib A, De Marco F, De Carlo M, Fiorina C, Barbanti M, Montone RA, Agnifili M, Petronio AS, Ettori F, Klugmann S, Tamburino C, Brambilla N, Colombo A, Bedogni F (2016) The failing right heart: implications and evolution in high-risk patients undergoing transcatheter aortic valve implantation. EuroIntervention 12(12):1542–1549. https://doi.org/10.4244/eij-d-15-00148
Mollmann H, Husser O, Blumenstein J, Liebetrau C, Dorr O, Kim WK, Nef H, Tesche C, Hamm CW, Elsasser A, Achenbach S, Gaede L (2020) Lower mortality in an all-comers aortic stenosis population treated with TAVI in comparison to SAVR. Clin Res Cardiol Off J German Cardiac Soc 109(5):611–615. https://doi.org/10.1007/s00392-019-01548-1
Schaefer A, Neumann N, Linder M, Schofer N, Schneeberger Y, Deuschl F, Schoen G, Blankenberg S, Reichenspurner H, Conradi L, Schafer U (2018) Outcomes with a latest generation self-expandable, intra-annular, re-sheathable transcatheter heart valve system: analysis of patients with impaired left ventricular function and determinants for pacemaker implantation. Clin Res Cardiol Off J German Cardiac Soc 107(10):914–923. https://doi.org/10.1007/s00392-018-1263-x
Trenkwalder T, Pellegrini C, Holzamer A, Rheude T, Riester J, Reinhard W, Mayr NP, Kasel AM, Gaede L, Blumenstein J, Kastrati A, Schunkert H, Joner M, Hilker M, Hengstenberg C, Husser O (2019) Prophylactic ECMO during TAVI in patients with depressed left ventricular ejection fraction. Clin Res Cardiol Off J German Cardiac Soc 108(4):366–374. https://doi.org/10.1007/s00392-018-1364-6
Von Scheidt W, Welz A, Pauschinger M, Fischlein T, Schachinger V, Treede H, Zahn R, Hennersdorf M, Albes JM, Bekeredjian R, Beyer M, Brachmann J, Butter C, Bruch L, Dorge H, Eichinger W, Franke UFW, Friedel N, Giesler T, Gradaus R, Hambrecht R, Haude M, Hausmann H, Heintzen MP, Jung W, Kerber S, Mudra H, Nordt T, Pizzulli L, Sack FU, Sack S, Schumacher B, Schymik G, Sechtem U, Stellbrink C, Stumpf C, Hoffmeister HM (2020) Interdisciplinary consensus on indications for transfemoral transcatheter aortic valve implantation (TF-TAVI) : joint consensus document of the Arbeitsgemeinschaft Leitende Kardiologische Krankenhausarzte e.V. (ALKK) and cooperating Cardiac Surgery Departments. Clin Res Cardiol Off J German Cardiac Soc 109(1):1–12. https://doi.org/10.1007/s00392-019-01528-5
Wernly B, Eder S, Navarese EP, Kretzschmar D, Franz M, Alushi B, Beckhoff F, Jung C, Lichtenauer M, Datz C, Schulze PC, Landmesser U, Hoppe UC, Falk V, Lauten A (2019) Transcatheter aortic valve replacement for pure aortic valve regurgitation: “on-label” versus “off-label” use of TAVR devices. Clin Res Cardiol Off J German Cardiac Soc 108(8):921–930. https://doi.org/10.1007/s00392-019-01422-0
Wernly B, Zappe AK, Unbehaun A, Sinning JM, Jung C, Kim WK, Fichtlscherer S, Lichtenauer M, Hoppe UC, Alushi B, Beckhoff F, Wewetzer C, Franz M, Kretzschmar D, Navarese E, Landmesser U, Falk V, Lauten A (2019) Transcatheter valve-in-valve implantation (VinV-TAVR) for failed surgical aortic bioprosthetic valves. Clin Res Cardiol Off J German Cardiac Soc 108(1):83–92. https://doi.org/10.1007/s00392-018-1326-z
Jackson RG, Patel R, Jayatilleke N, Kolliakou A, Ball M, Gorrell G, Roberts A, Dobson RJ, Stewart R (2017) Natural language processing to extract symptoms of severe mental illness from clinical text: the clinical record interactive search comprehensive data extraction (CRIS-CODE) project. BMJ Open 7(1):e012012. https://doi.org/10.1136/bmjopen-2016-012012
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Meder is part of the Scientific Advisory Board of Fleischhacker GmbH. All other authors have no conflicts of interest to declare.
Ethics approval and consent to participate
All patients were informed about specific risks and alternatives of TAVI and gave informed written consent to TAVI and pre- and post-interventional monitoring (data collection). The study protocol was approved by the local ethics committee (S-299/2015).
Availability of data and material
An anonymized spreadsheet regarding the data population is annexed to the supplementary data.
Code availability
Preprocessing code, machine learning implementations, and trained clinical outcomes classifications models are all open source and available at: “https://github.com/AIforTAVI/OutcomesTAVIwithML”.
Additional information
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gomes, B., Pilz, M., Reich, C. et al. Machine learning-based risk prediction of intrahospital clinical outcomes in patients undergoing TAVI. Clin Res Cardiol 110, 343–356 (2021). https://doi.org/10.1007/s00392-020-01691-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01691-0