Abstract
Serum interleukin-8 (IL-8) levels and tumor neutrophil infiltration are associated with worse prognosis in advanced cancers. Here, using a large-scale retrospective analysis, we show that elevated baseline serum IL-8 levels are associated with poor outcome in patients (n = 1,344) with advanced cancers treated with nivolumab and/or ipilimumab, everolimus or docetaxel in phase 3 clinical trials, revealing the importance of assessing serum IL-8 levels in identifying unfavorable tumor immunobiology and as an independent biomarker in patients receiving immune-checkpoint inhibitors.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
K.A.S.’s laboratory designed, conducted, analyzed and interpreted the data presented in Fig. 2b–j and Extended Data Fig. 6 (Yale Human Investigation Committee protocols 9505008219 and 1608018220). Bristol-Myers Squibb funded the studies CheckMate 067 (NCT01844505), CheckMate 017 (NCT01642004), CheckMate 057 (NCT01673867), CheckMate 025 (NCT01668784), CheckMate 038 (NCT01621490) and CheckMate 064 (NCT01783938) and participated in the design, conduct, analyses, and interpretation of these studies and related data (Figs. 1, 2a, Extended Data Figs. 1–3, 5, 7–9). Source data for Figs. 1, 2 and Extended Data Fig. 4 are provided in Supplementary Data 1. Bristol-Myers Squibb’s policy on data sharing may be found at https://www.bms.com/researchers-and-partners/independent-research/data-sharing-request-process.html.
References
Ribas, A. & Wolchok, J. D. Cancer immunotherapy using checkpoint blockade. Science 359, 1350–1355 (2018).
Havel, J. J., Chowell, D. & Chan, T. A. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat. Rev. Cancer 19, 133–150 (2019).
O’Donnell, J. S., Teng, M. W. L. & Smyth, M. J. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat. Rev. Clin. Oncol. 16, 151–167 (2019).
Schalper, K. A., Kaftan, E. & Herbst, R. S. Predictive biomarkers for PD-1 axis therapies: the hidden treasure or a call for research. Clin. Cancer Res. 22, 2102–2104 (2016).
Moore, B. B. et al. Distinct CXC chemokines mediate tumorigenicity of prostate cancer cells. Am. J. Pathol. 154, 1503–1512 (1999).
Baggiolini, M. CXCL8 — the first chemokine. Front. Immunol. 6, 285 (2015).
Baggiolini, M., Walz, A. & Kunkel, S. L. Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J. Clin. Invest. 84, 1045–1049 (1989).
David, J. M., Dominguez, C., Hamilton, D. H. & Palena, C. The IL-8/IL-8R axis: a double agent in tumor immune resistance. Vaccines 4, 22 (2016).
Alfaro, C. et al. Tumor-produced interleukin-8 attracts human myeloid-derived suppressor cells and elicits extrusion of neutrophil extracellular traps (NETs). Clin. Cancer Res. 22, 3924–3936 (2016).
Sanmamed, M. F. et al. Changes in serum interleukin-8 (IL-8) levels reflect and predict response to anti-PD-1 treatment in melanoma and non-small-cell lung cancer patients. Ann. Oncol. 28, 1988–1995 (2017).
Templeton, A. J. et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J. Natl Cancer Inst. 106, dju124 (2014).
Coffelt, S. B., Wellenstein, M. D. & de Visser, K. E. Neutrophils in cancer: neutral no more. Nat. Rev. Cancer 16, 431–446 (2016).
Kapanadze, T. et al. Regulation of accumulation and function of myeloid derived suppressor cells in different murine models of hepatocellular carcinoma. J. Hepatol. 59, 1007–1013 (2013).
Gabrilovich, D. I., Ostrand-Rosenberg, S. & Bronte, V. Coordinated regulation of myeloid cells by tumours. Nat. Rev. Immunol. 12, 253–268 (2012).
Wargo, J. A., Reuben, A., Cooper, Z. A., Oh, K. S. & Sullivan, R. J. Immune effects of chemotherapy, radiation, and targeted therapy and opportunities for combination with immunotherapy. Semin. Oncol. 42, 601–616 (2015).
Bilusic, M. et al. Phase I trial of HuMax-IL8 (BMS-986253), an anti-IL-8 monoclonal antibody, in patients with metastatic or unresectable solid tumors. J. Immunother. Cancer 7, 240 (2019).
Conroy, S., Kruyt, F. A. E., Wagemakers, M., Bhat, K. P. L. & den Dunnen, W. F. A. IL-8 associates with a pro-angiogenic and mesenchymal subtype in glioblastoma. Oncotarget 9, 15721–15731 (2018).
Ayers, M. et al. IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Invest. 127, 2930–2940 (2017).
Siemers, N. O. et al. Genome-wide association analysis identifies genetic correlates of immune infiltrates in solid tumors. PLoS ONE 12, e0179726 (2017).
Larkin, J. et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 373, 23–34 (2015).
Brahmer, J. et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N. Engl. J. Med. 373, 123–135 (2015).
Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N. Engl. J. Med. 373, 1627–1639 (2015).
Motzer, R. J. et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 373, 1803–1813 (2015).
Carleton, M. et al. Serum interleukin 8 (IL-8) may serve as a biomarker of response to immuno-oncology (I-O) therapy. J. Clin. Oncol. 36, 3025 (2018).
Ribas, A. et al. Immunomodulatory effects of nivolumab and ipilimumab in combination or nivolumab monotherapy in advanced melanoma patients: CheckMate 038. Cancer Res. 77, CT073 (2017).
Riaz, N. et al. Tumor and microenvironment evolution during immunotherapy with nivolumab. Cell 171, 934–949 (2017).
Weber, J. S. et al. Sequential administration of nivolumab and ipilimumab with a planned switch in patients with advanced melanoma (CheckMate 064): an open-label, randomised, phase 2 trial. Lancet Oncol. 17, 943–955 (2016).
Heagerty, P. J., Lumley, T. & Pepe, M. S. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 56, 337–344 (2000).
The Cancer Genome Atlas Research Network et al. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 45, 1113–1120 (2013).
Chalmers, Z. R. et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9, 34 (2017).
Villarroel-Espindola, F. et al. Spatially resolved and quantitative analysis of VISTA/PD-1H as a novel immunotherapy target in human non–small cell lung cancer. Clin. Cancer Res. 24, 1562–1573 (2018).
Datar, I. et al. Expression analysis and significance of PD-1, LAG-3, and TIM-3 in human non–small cell lung cancer using spatially resolved and multiparametric single-cell analysis. Clin. Cancer Res. 25, 4663–4673 (2019).
Schalper, K. A. et al. Objective measurement and clinical significance of TILs in non-small cell lung cancer. J. Natl Cancer Inst. 107, dju435 (2015).
Acknowledgements
We thank the patients and their families who made this study possible and the clinical study teams who participated in this study; DAKO for collaborative development of the PD-L1 IHC 28-8 pharmDx assay; Bristol-Myers Squibb and ONO Pharmaceutical Company Ltd. This study was supported by Bristol-Myers Squibb, Yale SPORE in Lung Cancer (P50CA196530), Department of Defense–Lung Cancer Research Program (W81XWH-16-1-0160), Yale Cancer Center Support Grant (P30CA016359), Stand Up To Cancer–American Cancer Society Lung Cancer Dream Team Translational Research Grant (SU2C-AACR-DT1715 and SU2C-AACR-DT22-17) and a grant from the Mark Foundation (19-029-MIA). I.M. is funded by MINECO SAF2017-83267-C2-1-R (AEI/FEDER, UE; I.M), European Union’s Horizon 2020 research and innovation program (635122, PROCROP) and Fundación de la Asociación Española Contra el Cáncer (AECC). M.F.S. is supported by a Miguel Servet contract from Instituto de Salud Carlos III, Fondo de Investigacion Sanitaria (Spain). The results shown here are in part based on data generated by the TCGA Research Network (https://www.cancer.gov/tcga). Writing and editorial assistance was provided by B. L. Phillips of Chrysalis Medical Communications, funded by Bristol-Myers Squibb.
Author information
Authors and Affiliations
Contributions
I.M. conceptually designed and supervised the study, performed the data analysis, wrote the manuscript and critically revised the manuscript. K.A.S. conceptually designed and supervised the study, performed data acquisition, analysis or interpretation, wrote the manuscript and critically revised the manuscript. M.C. performed the data acquisition, analysis, or interpretation, conceptually designed the study, served as Bristol-Myers Squibb lead in managing internal Bristol-Myers Squibb efforts across multiple functional groups to assemble data for analysis and figure generation and critically revised the manuscript. M.F.S. conceptually designed and supervised the study, wrote the manuscript and critically revised the manuscript. T.P.R. conceptually designed the study and critically revised the manuscript. P.P. contributed to the data planning, analysis and figure designs for Figs. 1, 2a, Extended Data Figs. 1, 3 and 7. J.G. analyzed TCGA data used in this work and reviewed the TCGA data analysis section of the manuscript. M.Z. performed data acquisition, analysis or interpretation, including statistical analyses, and critically revised the manuscript. A.M.W., S.-P.H., T.C., Y.F., Q.W. and H.Z. performed the data acquisition, analysis or interpretation and critically revised the manuscript. D.P., D.L. and J.L.P.-G. conceptually designed the study, wrote the manuscript, critically revised the manuscript and performed the data acquisition, analysis or interpretation. T.B. performed the digital pathology image analysis of immunostained histology slides. V.B. performed the computational image analysis of commercial samples stained with CD15 (neutrophil marker) and IL-8 to demonstrate the positive correlation across multiple indications and interpreted the data, which provided additional supporting evidence for the overall hypothesis. V.N. measured levels of IL-8 protein and neutrophil markers in NSCLC and melanoma tumor tissues and analyzed their relationship. N.G. performed the QIF data acquisition and analyses and contributed to the manuscript figures. All authors contributed to and approved the work presented in this study.
Corresponding authors
Ethics declarations
Competing interests
I.M. reports receiving commercial research grants from Bristol-Myers Squibb, Bioncotech, Alligator, AstraZeneca and Roche; has received speakers bureau honoraria from MSD; and is a consultant/advisory board member for Bristol-Myers Squibb, Roche, Genmab, F-Star, Bioncotech, Bayer, Numab, Alligator, Boehringer Ingelheim and AstraZeneca. K.A.S. reports receiving research funding from Genoptix/Navigate (Novartis), Vasculox/Tioma, Tesaro, Moderna Therapeutics, Takeda, Surface Oncology, Pierre-Fabre Research Institute, Merck, Bristol-Myers Squibb, AstraZeneca and Eli Lilly; has received consultant/advisory board fees from Celgene, Moderna Therapeutics, Shattuck Labs, Pierre-Fabre, AbbVie, AstraZeneca, EMD Serono, Ono Pharmaceuticals, Clinica Alemana de Santiago, Dynamo Therapeutics, Torque Therapeutics, Agenus and Takeda; and has received speaker honoraria and/or travel support for meetings from Takeda, Merck, Bristol-Myers Squibb, Fluidigm, Peerview, Biotrac, Cambridge Healthtech Institute, Shattuck Labs and Genentech. J.L.P.-G. reports grants, personal fees and nonfinancial support from Roche, Bristol-Myers Squibb and MSD; and reports grants and personal fees from Ipsen and Eisai, and grants from Incyte and Janssen. M.C., M.Z., S.-P.H., T.C. and Y.F. have a patent (‘Combination Therapy with Anti-IL-8 Antibodies and Anti-PD-1 Antibodies for Treating Cancer’, publication number WO 2019140150). T.P.R. is a co-inventor in a provisional patent application (application number 62/650047) regarding the use of anti-IL-8 and anti-PD1 for the treatment of cancer. M.C., M.Z., T.C., Y.F., S.-P.H., A.M.W, V.B, D.P., T.B., D.L., T.P.R., P.P., J.G. and H.Z. are current or former employees of Bristol-Myers Squibb, which is developing anti-IL-8 (NCT03400332). T.P.R., A.M.W., D.L. and S.-P.H. own stock in Bristol-Myers Squibb. None of the remaining authors have relevant conflicts of interest to report.
Additional information
Peer review information Saheli Sadanand was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Statistical identification of a baseline serum IL-8 cutoff below which patients were more likely to benefit from Nivo-based therapy.
ROC curve analyses were used to assess ORR, 6-month PFS, and 12-month OS. OS AUC (12-month) is indicated and identifies ≥23 pg/ml as a cutoff. All cases with nivolumab-containing therapies were analyzed. AUC, area under the curve; Nivo, nivolumab; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; ROC, receiver operator characteristic.
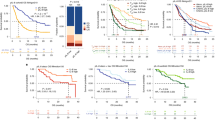
Extended Data Fig. 2 Association between elevated IL-8 and survival across treatments and tumor types.
Percentage of patients with baseline serum IL-8 levels ≥23 pg/ml across Mel (CheckMate 067: nivolumab, n = 292; ipilimumab, n = 298; nivolumab plus ipilimumab, n = 297), RCC (CheckMate 025, n = 392), sqNSCLC (CheckMate 017, n = 108), and nsqNSCLC (CheckMate 057, n = 255) with nivolumab monotherapy, ipilimumab monotherapy, or nivolumab plus ipilimumab combination therapy, as indicated. PFS and OS hazard ratios (IL-8 ≥ 23 pg/ml versus IL-8 < 23 pg/mL) are also presented (95% CI). HR, hazard ratio; IL, interleukin; Mel, melanoma; nsqNSCLC, nonsquamous non-small cell lung cancer; OS, overall survival; PFS, progression-free survival; RCC, renal cell carcinoma; sqNSCLC, squamous NSCLC.
Extended Data Fig. 3 Association between elevated IL-8 level and reduced survival was also seen in the non-immunotherapy trial arms.
The specific study, 2-sided log-rank test P values for the survival analysis, the number of independent patients with available IL-8 and OS data (n), and the OS HR (based on Cox proportional hazard model) between IL-8 subgroups (≥23 pg/ml versus <23 pg/ml) are indicated within each chart. a, Probability of OS with <23 pg/ml or ≥23 pg/ml IL-8 levels in patients with RCC treated with everolimus from CheckMate 025 (n = 348). b, Probability of OS with <23 pg/ml or ≥23 pg/ml IL-8 levels in patients with nsqNSCLC treated with docetaxel from CheckMate 057 (n = 253). HR, hazard ratio; IL, interleukin; nsqNSCLC, nonsquamous non-small cell lung cancer; OS, overall survival; RCC, renal cell carcinoma.
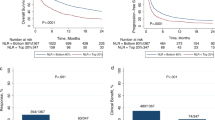
Extended Data Fig. 4 ORR by IL-8 subgroup across trials and treatment arms.
ORR vs baseline serum IL-8 levels <23 pg/ml or ≥23 pg/ml across treatment arms in CheckMate 067 (Mel), CheckMate 025 (RCC), CheckMate 017 (sqNSCLC), and CheckMate 057 (nsqNSCLC). IL, interleukin; Mel, melanoma; nsqNSCLC, nonsquamous non-small cell lung cancer; ORR, objective response rate; RCC, renal cell carcinoma; sqNSCLC, squamous NSCLC. aPatients with complete response or partial response per RECIST v1.1.
Extended Data Fig. 5 Percentage of patients in each IL-8 subgroup by PD-L1 status (negative or positive) across cohorts.
Percentage of patients with baseline serum IL-8 levels <23 pg/ml or ≥23 pg/ml by PD-L1 status (negative [<1%] or positive [≥1%]) in Mel (CheckMate 067 [PD-L1 < 1%, n = 183; PD-L1 ≥ 1%, n = 673; P = 0.296]) (a), RCC (CheckMate 025 [PD-L1 < 1%, n = 514; PD-L1 ≥ 1%, n = 168; P = 0.884]) (b), sqNSCLC (CheckMate 017 [PD-L1 < 1%, n = 85; PD-L1 ≥ 1%, n = 99; P = 0.263]) (c), and nsqNSCLC (CheckMate 057 [PD-L1 < 1%, n = 181; PD-L1 ≥ 1%, n = 224; P = 0.171]) (d). IL, interleukin; Mel, melanoma; nsqNSCLC, nonsquamous non-small cell lung cancer; PD-L1, programmed death-ligand 1; RCC, renal cell carcinoma; sqNSCLC, squamous NSCLC; P, p-value for chi-squared test of independence between IL-8 subgroup (≥23 pg/ml vs < 23 pg/ml) and PD-L1 status (≥1% vs < 1%).
Extended Data Fig. 6 Association between IL-8 expression and TMB in human malignancies.
Association between IL-8 mRNA expression and TMB in human Mel (a, n = 324), RCC (b, n = 291), nsqNSCLC (c, n = 427), and sqNSCLC (d, n = 382) from TCGA cohort. The levels of IL-8 transcripts are presented as log10 transformed FPKM units. TMB level was determined as previously reported, including both nonsynonymous and synonymous variants. Dots represent individual samples. Linear regression lines are indicated by purple lines within each chart. IL, interleukin; FPKM, kilobase per million mapped reads; Mel, melanoma; nsqNSCLC, nonsquamous non-small cell lung cancer; RCC, renal cell carcinoma; sqNSCLC, squamous NSCLC; TMB, tumor mutational burden.
Extended Data Fig. 7 Youden’s index by baseline IL-8 cutoff (in pg/ml) from OS ROC curve analyses.
Determination of optimal IL-8 cutoff value for the Nivo-containing arm of CheckMate 067 (n = 589) (a), nivolumab arm of CheckMate 025 (n = 392) (b), nivolumab arm of CheckMate 017 (n = 108) (c), nivolumab arm of CheckMate 057 (n = 255) (d), and all studies pooled (N = 1,344) (e). Red dotted lines indicate 23 pg/ml. IL, interleukin; Nivo, nivolumab; OS, overall survival; ROC, receiver operating characteristic.
Extended Data Fig. 8 Peripheral blood and tumor samples from 1,344 patients treated with nivolumab or nivolumab plus ipilimumab in 4 phase 3 clinical trials included in the analyses.
Summary of 4 phase 3 clinical trials (CheckMate 067, CheckMate 017, CheckMate 057, CheckMate 025, N = 1,344 patients). IL, interleukin; Mel, melanoma; nsqNSCLC, nonsquamous non-small cell lung cancer; RCC, renal cell carcinoma; sqNSCLC, squamous NSCLC. aIncludes patients who were treated with nivolumab or nivolumab + ipilimumab and had nonmissing serum IL-8 levels.
Extended Data Fig. 9 Kaplan-Meier analyses to assess overall survival stratified by baseline serum IL-8 levels.
Analysis of pooled data from 1,344 patients receiving nivolumab-based therapy in 4 phase 3 trials—including patients with melanoma, renal cell carcinoma, squamous non-small cell lung cancer, and nonsquamous non-small cell lung cancer—confirmed that elevated baseline serum IL-8 levels were associated with overall survival. This association was significant after adjustment for baseline tumor burden and tumor programmed death-ligand 1 expression (P < 0.001). aOS data from patients in CheckMate trials −017, −057, −067, −025. IL, interleukin.
Supplementary information
Supplementary Data 1
Supplementary datasets for Figs. 1, 2 and Extended Data Fig. 4.
Rights and permissions
About this article
Cite this article
Schalper, K.A., Carleton, M., Zhou, M. et al. Elevated serum interleukin-8 is associated with enhanced intratumor neutrophils and reduced clinical benefit of immune-checkpoint inhibitors. Nat Med 26, 688–692 (2020). https://doi.org/10.1038/s41591-020-0856-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-0856-x
This article is cited by
-
Preoperative IL-8 levels as prognostic indicators of overall survival: an extended follow-up in a prospective cohort with colorectal liver metastases
BMC Cancer (2024)
-
Blood-based biomarkers in patients with non-small cell lung cancer treated with immune checkpoint blockade
Journal of Experimental & Clinical Cancer Research (2024)
-
S100A9+CD14+ monocytes contribute to anti-PD-1 immunotherapy resistance in advanced hepatocellular carcinoma by attenuating T cell-mediated antitumor function
Journal of Experimental & Clinical Cancer Research (2024)
-
Harnessing innate immune pathways for therapeutic advancement in cancer
Signal Transduction and Targeted Therapy (2024)
-
Extramedullary hematopoiesis in cancer
Experimental & Molecular Medicine (2024)