Abstract
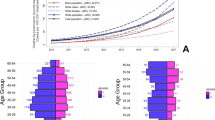
The ongoing substance misuse epidemic in the United States is complex and dynamic and should be approached as such in the development and evaluation of policy1. Drug overdose deaths (largely attributable to opioid misuse) in the United States have grown exponentially for almost four decades, but the mechanisms of this growth are poorly understood2. From analysis of 661,565 overdose deaths from 1999 to 2017, we show that the age-specific drug overdose mortality curve for each birth-year cohort rises and falls according to a Gaussian-shaped curve. The ascending portion of each successive birth-year cohort mortality curve is accelerated compared with that of all preceding birth-year cohorts. This acceleration can be attributed to either of two distinct processes: a stable peak age, with an increasing amplitude of mortality rate curves from one birth-year cohort to the next; or a youthward shift in the peak age of the mortality rate curves. The overdose epidemic emerged and increased in amplitude among the 1945–1964 cohort (Baby Boomers), shifted youthward among the 1965–1980 cohort (Generation X), and then resumed the pattern of increasing amplitude in the 1981–1990 Millennials. These shifting age and generational patterns are likely to be driven by socioeconomic factors and drug availability, the understanding of which is important for the development of effective overdose prevention measures.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Multiple Cause of Death Data from the Centers for Disease Control and Prevention is available by request at https://wonder.cdc.gov/mcd.html. Population demographics from the US Census is available at https://data.census.gov/. The code for creating the hexamaps is provided in ref. 5. In addition, all the equations to reproduce the quadratic fits and the transformation equations to the set of Gaussian curves are presented in the online Methods. The numerical results of the quadratic fits are presented in Supplementary Table 1.
References
Burke, D. S. Forecasting the opioid epidemic. Science 354, 529–529 (2016).
Jalal, H. et al. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science 361, eaau1184 (2018).
Best, A. F. et al. Premature mortality projections in the USA through 2030: a modelling study. Lancet Public Health 3, e374–e384 (2018).
Keyes, K. M. & Li, G. Age–period–cohort modeling. In Injury Research (eds., Li, G., Baker, S.) 409–426 (Springer, 2012).
Jalal H. J., & Burke D. S. Hexamaps for visualizing age-period-cohort data trends. Preprint at medRxiv https://doi.org/10.1101/19011700 (2019)
Pew Research Center. The Whys and Hows of Generations Research. Pew Research Center, September, 2015 https://www.people-press.org/2015/09/03/the-whys-and-hows-of-generations-research/
Ciccarone, D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int. J. Drug Policy 46, 107–111 (2017).
Ciccarone, D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int. J. Drug Policy 71, 183–188 (2019).
Bjork, J. M. & Pardini, D. A. Who are those “risk-taking adolescents”? Individual differences in developmental neuroimaging research. Dev. Cogn. Neurosci. 11, 56–64 (2015).
Viboud, C., Simonsen, L. & Chowell, G. A generalized-growth model to characterize the early ascending phase of infectious disease outbreaks. Epidemics 15, 27–37 (2016).
Smith, M. K., Graham, M., Latkin, C. A., Mehta, S. H. & Cummings, D. A. T. Quantifying potentially infectious sharing patterns among people who inject drugs in baltimore, USA. Epidemiol. Infect. 146, 1845–1853 (2018).
Mossong, J. et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 5, e74 (2008).
Duncan, D. F., Nicholson, T., White, J. B., Bradley, D. B. & Bonaguro, J. The baby boomer effect: changing patterns of substance abuse among adults ages 55 and older. J. Aging Soc. Policy 22, 237–248 (2010).
Magura, S. et al. Determinants of needle sharing among intravenous drug users. Am. J. Public Health 79, 459–462 (1989).
Luthar, S. S., Anton, S. F., Merikangas, K. R. & Rounsaville, B. J. Vulnerability to drug abuse among opioid addicts’ siblings: individual, familial, and peer influences. Compr. Psychiatry 33, 190–196 (1992).
Needle, R. et al. Interpersonal influences in adolescent drug use—the role of older siblings, parents, and peers. Int. J. Addict. 21, 739–766 (1986).
Windle, M. Parental, sibling, and peer influences on adolescent substance use and alcohol problems. Appl. Dev. Sci. 4, 98–110 (2000).
Scholl, L., Seth, P., Kariisa, M., Wilson, N. & Baldwin, G. Drug and opioid-Involved overdose deaths—United States, 2013–2017. MMWR Morb. Mortal. Wkly Rep. 67, 1419–1427 (2018).
Rudd, R. A., Seth, P., David, F. & Scholl, L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb. Mortal. Wkly Rep. 65, 1445–1452 (2016).
Ahmad, F. B., Rossen, L. M. & Sutton, P. Provisional drug overdose death counts. National Center for Health Statistics; 2019. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm.
Blanco, C. & Volkow, N. D. Management of opioid use disorder in the USA: present status and future directions. Lancet 393, 1760–1772 (2019).
Coffin, P. O. & Rich, J. D. Overdose research: 15 Years Later. J. Urban Health 96, 1–5 (2019).
Ruhm, C. J. Drivers of the fatal drug epidemic. J. Health Econ. 64, 25–42 (2019).
Bao, Y. et al. Prescription drug monitoring programs are associated with sustained reductions in opioid prescribing by physicians. Health Aff. 35, 1045–1051 (2016).
Patrick, S. W., Fry, C. E., Jones, T. F. & Buntin, M. B. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff. 35, 1324–1332 (2016).
Oldfield, B. J., Fuller, W. S. & Becker, W. C. Opioids are not better than non-opioid pain medications for chronic back, hip, or knee pain. J. Gen. Intern. Med. 34, 1854–1856 (2019).
Yim, N. & Don Parsa, F. From the origins of the opioid use (and misuse) to the challenge of opioid-free pain management in surgery. In From Conventional to Innovative Approaches for Pain Treatment (ed., Cascella, M.) 1–10 (2019).
Lambdin, B. H., Davis, C. S., Wheeler, E., Tueller, S. & Kral, A. H. Naloxone laws facilitate the establishment of overdose education and naloxone distribution programs in the United States. Drug Alcohol Depend. 188, 370–376 (2018).
Wheeler, E., Jones, T. S., Gilbert, M. K. & Davidson, P. J. Opioid overdose prevention programs providing naloxone to laypersons — United States, 2014. MMWR Morb. Mortal. Wkly Rep. 64, 631–635 (2015).
McGinty, E. E. et al. Public support for safe consumption sites and syringe services programs to combat the opioid epidemic. Prev. Med. 111, 73–77 (2018).
Des Jarlais, D. C., McKnight, C., Goldblatt, C. & Purchase, D. Doing harm reduction better: syringe exchange in the United States. Addiction 104, 1441–1446 (2009).
Bluthenthal, R. N., Kral, A. H., Lorvick, J. & Watters, J. K. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Med. Anthropol. 18, 61–83 (1997).
Compton, W. M., Jones, C. M. & Baldwin, G. T. Relationship between nonmedical prescription-opioid use and heroin use. N. Engl. J. Med. 374, 154–163 (2016).
Mars, S. G. et al. Heroin-related overdose: the unexplored influences of markets, marketing and source-types in the United States. Soc. Sci. Med. 140, 44–53 (2015).
Mars, S. G., Bourgois, P., Karandinos, G., Montero, F. & Ciccarone, D. “Every ‘never’ I ever said came true”: transitions from opioid pills to heroin injecting. Int. J. Drug Policy 25, 257–266 (2014).
Weatherburn, D., Jones, C., Freeman, K. & Makkai, T. Supply control and harm reduction: lessons from the Australian heroin ‘drought’. Addiction 98, 83–91 (2003).
O’Donnell, J. K., Gladden, R. M. & Seth, P. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by Census Region—United States, 2006–2015. MMWR Morb. Mortal. Wkly Rep. 66, 897–903 (2017).
O’Donnell, J. K., Halpin, J., Mattson, C. L., Goldberger, B. A. & Gladden, R. M. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 States, July–December 2016. MMWR Morb. Mortal. Wkly Rep. 66, 1197–1202 (2017).
Seth, P., Scholl, L., Rudd, R. A. & Bacon, S. Overdose deaths involving opioids, cocaine, and psychostimulants—United States, 2015–2016. MMWR Morb. Mortal Wkly Rep. 67, 349–358 (2018).
Rosenberg, P. S., Check, D. P. & Anderson, W. F. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol. Biomarkers Prev. 23, 2296–2302 (2014).
Rosenberg, P. S. A new age-period-cohort model for cancer surveillance research. Stat. Methods Med. Res. 28, 3363–3391 (2011).
Chernyavskiy, P., Little, M. P. & Rosenberg, P. S. A unified approach for assessing heterogeneity in age-period-cohort model parameters using random effects. Stat. Methods Med. Res. 28, 20–34 (2019).
Acknowledgements
This study was in part supported by National Institutes of Health/National Center for Advancing Translational Sciences grant no. 1KL2TR0001856 (H.J.), and Robert Wood Johnson Foundation grant no. 72858 (J.B. and D.S.B.).
Author information
Authors and Affiliations
Contributions
D.S.B. and H.J. conceived of the study, H.J. and J.M.B. conducted the data analyses, and H.J., D.S.B., J.M.B., D.R.S. and M.S.R. all contributed to the interpretation of results and writing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Jennifer Sargent was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Results of age–period–cohort analysis from the first Poisson log-linear regression model.
Black horizontal line represents no effect, the black curves represent the estimated effect and the orange and green shaded area represent the associated confidence interval. a, b and c show the age, period and cohort deviations which reveal significant statistical deviation for most ages, periods and cohorts (since the confidence interval does not cover 0). The net drift from this analysis was 8.23% per year CI = (8.17, 8.30) and is also statistically significant since the confidence interval does not cover 0 (D). d also shows statistically significant differences in the age-specific local drifts against the net drift which range between 4% to 11%. e shows the cross-sectional and longitudinal age curves for overdose mortality. The cross-sectional curve reveals the age-specific mortality rates for the reference period of p0 = 2000, and the longitudinal age curve reveals the age-specific mortality rate for the reference cohort of c0 = 1960. The clear divergence of these two age curves indicates important cohort effects that can also be revealed from the net drift. (F) and (G) reveal the period and cohort rate ratios of mortality rate against the reference period (p0 = 2000) and reference cohort (c0 = 1960), respectively.
Extended Data Fig. 2 Hexamaps showing the reproducibility of overdose deaths from the Gaussian curves.
The raw drug overdose mortality rates are shown in a and a reconstruction from the quadratic equation Gaussian curves is shown in b. Both the original data plot and the reconstructed plot are limited to birth-year cohorts after 1940.
Extended Data Fig. 3 Relationship between the peak age for overdose mortality and peak overdose mortality rates.
The purple line indicates the estimated peak age and overdose mortality for birth-years from 1940 through 1990. Decennial cohorts are marked with a red circle and labeled. The horizontal and vertical blue lines represent the 95% confidence interval of the estimated peak age for overdose mortality and peak overdose mortality rate, respectively.
Supplementary information
Supplementary Information
Supplementary Table 1.
Supplementary Video 1
Fitted age-specific mortality rate curves by single birth-year cohorts from 1940 to 1990 are displayed in sequence. For each birth-year cohort, the red data points and lines represent the observed data, the solid blue lines represent the fitted Gaussian curve and dotted blue lines represent the projected curve. The shaded area around each line represents the confidence interval.
Rights and permissions
About this article
Cite this article
Jalal, H., Buchanich, J.M., Sinclair, D.R. et al. Age and generational patterns of overdose death risk from opioids and other drugs. Nat Med 26, 699–704 (2020). https://doi.org/10.1038/s41591-020-0855-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-0855-y
This article is cited by
-
Comparative age-period-cohort analysis
BMC Medical Research Methodology (2023)
-
Responding to the US opioid crisis: leveraging analytics to support decision making
Health Care Management Science (2023)
-
Opioid-related deaths in Ontario correctional facilities and penitentiaries (2009–2019)
Forensic Science, Medicine and Pathology (2023)
-
Characteristics of events in which police responded to overdoses: an examination of incident reports in Rhode Island
Harm Reduction Journal (2022)
-
A Large-Scale Observational Study on the Temporal Trends and Risk Factors of Opioid Overdose: Real-World Evidence for Better Opioids
Drugs - Real World Outcomes (2021)