Abstract
Recurrent medulloblastoma and ependymoma are universally lethal, with no approved targeted therapies and few candidates presently under clinical evaluation. Nearly all recurrent medulloblastomas and posterior fossa group A (PFA) ependymomas are located adjacent to and bathed by the cerebrospinal fluid, presenting an opportunity for locoregional therapy, bypassing the blood–brain barrier. We identify three cell-surface targets, EPHA2, HER2 and interleukin 13 receptor α2, expressed on medulloblastomas and ependymomas, but not expressed in the normal developing brain. We validate intrathecal delivery of EPHA2, HER2 and interleukin 13 receptor α2 chimeric antigen receptor T cells as an effective treatment for primary, metastatic and recurrent group 3 medulloblastoma and PFA ependymoma xenografts in mouse models. Finally, we demonstrate that administration of these chimeric antigen receptor T cells into the cerebrospinal fluid, alone or in combination with azacytidine, is a highly effective therapy for multiple metastatic mouse models of group 3 medulloblastoma and PFA ependymoma, thereby providing a rationale for clinical trials of these approaches in humans.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
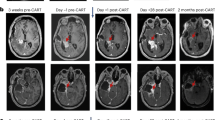
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All requests for raw and analyzed data and materials are promptly reviewed by the Hospital for Sick Children to verify whether the request is subject to any intellectual property or confidentiality obligations. Any materials that can be shared will be released via a material transfer agreement. All raw and analyzed sequencing datasets analyzed during the current study are open source, referenced and available from the following repositories: primary metastasis medulloblastoma pairs DNA methylation analysis, GSE63670; primary medulloblastoma genome-wide methylation and expression profile analysis, GSE85218; and primary ependymoma Affymetrix chip array analysis, GSE27279. All CAR T cell constructs used within the study have been previously published.
Change history
27 May 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41591-021-01362-1
References
Pui, C. H., Gajjar, A. J., Kane, J. R., Qaddoumi, I. A. & Pappo, A. S. Challenging issues in pediatric oncology. Nat. Rev. Clin. Oncol. 8, 540–549 (2011).
Vladoiu, M. C. et al. Childhood cerebellar tumors mirror conserved fetal transcriptional programs. Nature 572, 67–73 (2019).
Mack, S. C. et al. Therapeutic targeting of ependymoma as informed by oncogenic enhancer profiling. Nature 553, 101–105 (2018).
Khatua, S., Ramaswamy, V. & Bouffet, E. Current therapy and the evolving molecular landscape of paediatric ependymoma. Eur. J. Cancer 70, 34–41 (2017).
Ramaswamy, V. et al. Recurrence patterns across medulloblastoma subgroups: an integrated clinical and molecular analysis. Lancet Oncol. 14, 1200–1207 (2013).
Northcott, P. A. et al. The whole-genome landscape of medulloblastoma subtypes. Nature 547, 311–317 (2017).
Taylor, M. D. et al. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 123, 465–472 (2011).
Northcott, P. A et al. Medulloblastoma comprises four distinct molecular variants. J. Clin. Oncol. 29, 1408–1414 (2011).
Cavalli, F. M. et al. Intertumoral heterogeneity within medulloblastoma subgroups. Cancer Cell 31, 737–754 (2017).
Kulozik, A. E. et al. Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell 27, 728–743 (2015).
Morrissy, A. S. et al. Divergent clonal selection dominates medulloblastoma at recurrence. Nature 529, 351–357 (2016).
Garzia, L. et al. A hematogenous route for medulloblastoma leptomeningeal metastases. Cell 172, 1050–1062 (2018).
Bette, S. et al. Retrospective analysis of radiological recurrence patterns in glioblastoma, their prognostic value and association to postoperative infarct volume. Sci. Rep. 8, 1–12 (2018).
Mack, S. C. et al. Epigenomic alterations define lethal CIMP-positive ependymomas of infancy. Nature 506, 445–450 (2014).
Majzner, R. G. et al. CAR T cells targeting B7-H3, a pan-cancer antigen, demonstrate potent preclinical activity against pediatric solid tumors and brain tumors. Clin. Cancer Res. 25, 2560–2574 (2019).
Mount, C. W et al. Potent antitumor efficacy of anti-GD2 CAR T cells in H3-K27M+ diffuse midline gliomas. Nat. Med. 24, 572–579 (2018).
Brown, C. E et al. Bioactivity and safety of IL13Rα2-redirected chimeric antigen receptor CD8+ T cells in patients with recurrent glioblastoma. Clin. Cancer Res. 21, 4062–4072 (2105).
Keu, K. V. et al. Reporter gene imaging of targeted T cell immunotherapy in recurrent glioma. Sci. Transl. Med. 9, eaag2196 (2017).
Brown, C. E. et al. Regression of glioblastoma after chimeric antigen receptor T cell therapy. N. Engl. J. Med. 375, 2561–2569 (2016).
Ahmed, N. et al. HER2-specific chimeric antigen receptor-modified virus-specific T cells for progressive glioblastoma. JAMA Oncol. 3, 1094 (2017).
O'Rourke, D. M. et al. A single dose of peripherally infused EGFRvIII-directed CAR T cells mediates antigen loss and induces adaptive resistance in patients with recurrent glioblastoma. Sci. Transl. Med. 9, eaaa0984 (2017).
Ahmed, N. et al. Regression of experimental medulloblastoma following transfer of HER2-specific T cells. Cancer Res. 67, 5957–5964 (2007).
Nellan, A. et al. Durable regression of medulloblastoma after regional and intravenous delivery of anti-HER2 chimeric antigen receptor T cells. J. Immunother. Cancer 6, 30 (2018).
Chow, K. K. et al. T cells redirected to EphA2 for the immunotherapy of glioblastoma. Mol. Ther. 21, 629–637 (2013).
Krebs, S. et al. T cells redirected to interleukin-13Rα2 with interleukin-13 mutein-chimeric antigen receptors have anti-glioma activity but also recognize interleukin-13Rα1. Cytotherapy 16, 1121–1131 (2014).
Wu, X. et al. Clonal selection drives genetic divergence of metastatic medulloblastoma. Nature 482, 529–533 (2012).
Bielamowicz, K. et al. Trivalent CAR T cells overcome interpatient antigenic variability in glioblastoma. Neuro. Oncol. 20, 506–518 (2018).
Schulz, H. et al. Intraventricular treatment of relapsed central nervous system lymphoma with the anti-CD20 antibody rituximab. Haematologica 89, 753–754 (2004).
Kramer, K. et al. A phase II study of radioimmunotherapy with intraventricular 131I-3F8 for medulloblastoma. Pediatr. Blood Cancer 65, (2018).
Hwu, P. Lymphodepletion plus adoptive cell transfer with or without dendritic cell immunization in patients with metastatic melanoma. ClinicalTrials.gov Identifier: NCT00338377 (2006).
Witt, H. et al. Delineation of two clinically and molecularly distinct subgroups of posterior fossa ependymoma. Cancer Cell 20, 143–157 (2011).
Morrissy, A. S. et al. Spatial heterogeneity in medulloblastoma. Nat. Genet. 49, 780–788 (2017).
Priceman, S. J. et al. Regional delivery of chimeric antigen receptor-engineered T cells effectively targets HER2+ breast cancer metastasis to the brain. Clin. Cancer Res. 24, 95–105 (2018).
Brown, C. E. et al. Optimization of IL13Rα2-targeted chimeric antigen receptor T cells for improved anti-tumor efficacy against glioblastoma. Mol. Ther. 26, 31–44 (2018).
Stritesky, G. L., Yeh, N. & Kaplan, M. H. IL-23 promotes maintenance but not commitment to the Th17 lineage. J. Immunol. 181, 5948–5955 (2008).
Rasouli, J. et al. Expression of GM-CSF in T cells is increased in multiple sclerosis and suppressed by IFN-β therapy. J. Immunol. 194, 5085–5093 (2015).
Bergamaschi, C. et al. Circulating IL-15 exists as heterodimeric complex with soluble IL-15Rα in human and mouse serum. Blood 120, e1–8 (2012).
Hegde, M. et al. Tandem CAR T cells targeting HER2 and IL-13Rα2 mitigate tumor antigen escape. J. Clin. Invest. 126, 3036–3052 (2016).
Momparler, R. L., Côté, S., Momparler, L. F. & Idaghdour, Y. Epigenetic therapy of acute myeloid leukemia using 5-aza-2′-deoxycytidine (decitabine) in combination with inhibitors of histone methylation and deacetylation. Clin. Epigenetics 6, 19 (2014).
Montalban-Bravo, G. & Garcia-Manero, G. Myelodysplastic syndromes: 2018 update on diagnosis, risk-stratification and management. Am. J. Hematol. 93, 129–147 (2018).
Stresemann, C. & Lyko, F. Modes of action of the DNA methyltransferase inhibitors azacytidine and decitabine. Int. J. Cancer 123, 8–13 (2008).
Qiu, X. et al. Equitoxic doses of 5-azacytidine and 5-aza-2'deoxycytidine induce diverse immediate and overlapping heritable changes in the transcriptome. PLoS ONE 5, (2010).
Gang, A. O. et al. 5-azacytidine treatment sensitizes tumor cells to T cell mediated cytotoxicity and modulates NK cells in patients with myeloid malignancies. Blood Cancer J. 4, e197 (2014).
Goodyear, O. C. et al. Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood 119, 3361–3369 (2012).
Fozza, C. et al. Azacitidine improves the T cell repertoire in patients with myelodysplastic syndromes and acute myeloid leukemia with multilineage dysplasia. Leuk. Res. 39, 957–963 (2015).
Mokhtari, R. B. et al. Combination therapy in combating cancer. Oncotarget 8, 38022–38043 (2017).
Rodríguez-Paredes, M. & Esteller, M. Cancer epigenetics reaches mainstream oncology. Nat. Med. 17, 330–339 (2011).
Terracina, K. P. et al. DNA methyltransferase inhibition increases efficacy of adoptive cellular immunotherapy of murine breast cancer. Cancer Immunol. Immunother. 65, 1061–1073 (2016).
Quddus, J. et al. Treating activated CD4+ T cells with either of two distinct DNA methyltransferase inhibitors, 5-azacytidine or procainamide, is sufficient to cause a lupus-like disease in syngeneic mice. J. Clin. Invest. 92, 38–53 (1993).
Niu, L. CAR T cell immunotherapy for EphA2-positive malignant glioma patients. ClinicalTrials.gov Identifier: NCT02575261 (2017).
Goff, S. L. et al. Pilot trial of adoptive transfer of chimeric antigen receptor-transduced T cells targeting EGFRvIII in patients with glioblastoma. J. Immunother. 42, 126–135 (2019).
Morgan, R. A. et al. Case report of a serious adverse event following the administration of T cells transduced with a chimeric antigen receptor recognizing ERBB2. Mol. Ther. 18, 843–851 (2010).
Akhavan, D. et al. CAR T cells for brain tumors: lessons learned and road ahead. Immunol. Rev. 290, 60–84 (2019).
Azemar, M. et al. Regression of cutaneous tumor lesions in patients intratumorally injected with recombinant single-chain antibody-toxic targeted to ErbB2/HER2. Breast Cancer Res. Treat. 82, 155–164 (2003).
Jin, C. et al. Safe engineering of CAR T cells for adoptive cell therapy of cancer using long-term episomal gene transfer. EMBO Mol. Med. 8, 702–711 (2016).
McLendon, R. E. et al. Production and characterization of two ependymoma xenografts. J. Neuropathol. Exp. Neurol. 55, 540–548 (1996).
Kimura, S. et al. Antiproliferative and antitumor effects of azacytidine against the human myelodysplastic syndrome cell line SKM-1. Anticancer Res. 32, 795–798 (2012).
Ramaswamy, V. Treatment of children with refractory brain/solid tumors and recurrent ependymoma. ClinicalTrials.gov Identifier: NCT03206021 (2017).
Wang, X. et al. Medulloblastoma subgroups remain stable across primary and metastatic compartments. Acta Neuropathol. 154, 2262–2265 (2014).
Acknowledgements
M.D.T. is supported by the National Institutes of Health (R01CA148699 and R01CA159859), the Pediatric Brain Tumour Foundation, the Terry Fox Research Institute, the Canadian Institutes of Health Research, the Cure Search Foundation, b.r.a.i.n.child, Meagan’s Walk, SWIFTY Foundation, the Brain Tumour Charity, Genome Canada, Genome BC, Genome Quebec, the Ontario Research Fund, Worldwide Cancer Research, V-Foundation for Cancer Research and the Ontario Institute for Cancer Research through funding provided by the Government of Ontario. M.D.T. is also supported by a Canadian Cancer Society Research Institute Impact grant, a Cancer Research UK Brain Tumour Award and by a Stand Up To Cancer (SU2C) St. Baldrick’s Pediatric Dream Team Translational Research Grant (SU2C-AACR-DT1113) and SU2C Canada Cancer Stem Cell Dream Team Research Funding (SU2C-AACR-DT-19-15) provided by the Government of Canada through Genome Canada and the Canadian Institutes of Health Research, with supplementary support from the Ontario Institute for Cancer Research through funding provided by the Government of Ontario. SU2C is a program of the Entertainment Industry Foundation administered by the American Association for Cancer Research. M.D.T. is also supported by the Garron Family Chair in Childhood Cancer Research at the Hospital for Sick Children and the University of Toronto. N.A. is supported by National Institutes of Health (U54 CA232568-01), SU2C St. Baldrick’s Pediatric Dream Team Translational Research Grant (SU2C-AACR-DT1113). L.K.D. was supported by funding from Brain Canada NeuroDevNet. We thank P. Rose Matthew for her valuable help in making CAR T cells; S. Gottschalk for designing and constructing EPHA2 CAR; D. Trono for gifting psPAX2 and pMD2.G plasmids; S. Keir and D. Bigner for gifting Ep612 cells; and M. Essand for gifting pBMN(CMV-copGFP-Luc2-Puro) plasmid. The authors thank J. Loukides (Manager, Brain Tumour Biobank at SickKids) and recognize the Labatt Brain Tumour Research Centre and the Michael and Amira Dan Brain Tumour Bank Network. We gratefully thank the Pathology Research Program Laboratory, UHN, for their pathology assistance and the Centre for Phenogenomics for their animal husbandry support and BLI assistance. We thank S. Archer for technical writing assistance and editing and A. Carlow for manuscript support.
Author information
Authors and Affiliations
Contributions
L.K.D. designed, performed and analyzed the majority of experiments in this study and co-wrote the manuscript. A.D. performed and analyzed IHC. K.B., S.K.J., K.F., M.H. and A.Z.G. designed CAR constructs, produced CAR T cells and presented technical assistance. D.S. assisted with sample collections, DNA extractions, statistical analysis and figure preparation. R.V.O., Z.A. and S.V. supported azacytidine analysis. D.P. and C.R. provided in vitro support. B.L.H. and L.G. aided with MB PDX expansions and offered technical support. A.M., J.G.P., T.D. and B.L. assisted with animal husbandry, necropsies and drug administrations. J.H, A.G.S. and P.D.A. assisted with LV infusions. A.S.M., F.M.G.C. and V.R. helped perform microarray analysis. S.C.M. performed microarray and methylation analysis. C.N. and C.M.K.-F. aided with sample collection and drug administration. M.L.B. performed computational CAR modeling. M.C.V. assisted with BLI. A.M. and S.A.K. helped with EP cell expansions. L.Q. and N.H. provided pathology support. X.W. provided technical and reagents assistance. R.S. provided technical assistance. C.D., A.C.M.J., A.R., L.H., M.L., P.B. and K.K. supported manuscript and figure preparation. O.S. performed imaging analysis. C.C.F. provided histology samples. S.Y. and J.H. provided the multicenter EP TMA. C.H. provided the SickKids MB TMA. K.A. supplied sequencing assistance and support. M.D. provided pathology analysis. J.M.M. provided CHOP MB TMA and provided technical support. P.H.S. provided valuable pathology support. N.A. and M.D.T. supervised the project and co-wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Saheli Sadanand was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 EPHA2, HER2 and IL13Rα2 are immunotherapy targets in Group 3 medulloblastoma.
a, EPHA2 mRNA expression in human Group 3 medulloblastoma versus normal human adult and fetal cerebellum; b, HER2 expression in human Group 3 medulloblastoma versus normal human adult and fetal cerebellum; and c, IL13Rα2 expression in human Group 3 medulloblastoma versus normal human fetal and adult cerebellum, by expression microarray, two-sided Mann-Whitney U test. mRNA differential expression across human medulloblastoma subtypes versus normal adult and fetal cerebellum control for d, EPHA2; e, HER2; and f, IL13Rα2; as compared by expression microarray, * P < 0.05; **P < 0.005, two-sided Mann-Whitney U-test. g, EPHA2 mRNA expression in human WNT, SHH and Group 4 medulloblastoma subgroups versus normal human adult and fetal cerebellum h, HER2 mRNA expression in human WNT, SHH and Group 4 medulloblastoma subgroups versus normal human adult and fetal cerebellum; and i. IL13Rα2 mRNA expression in human WNT, SHH and Group 4 medulloblastoma subgroups versus normal human adult and fetal cerebellum as compared by expression microarray, two-sided one-way ANOVA with post-hoc Tukey HSD. All boxplot center lines show data median; box limits indicate the 25th and 75th percentiles; lower and upper whiskers extend 1.5 times the interquartile range (IQR) from the 25th and 75th percentiles, respectively. Outliers are represented by individual points. Error bars ± SEM j, H score of EPHA2 IHC (P = 0.6); k, H score of HER2 IHC (P = 0.6); l, H score of IL13Rα2 IHC (P = 0.9 two-sided Mann-Whitney U test) in human paediatric primary and metastases or recurrence for Group 3 medulloblastoma. m, Normal skeletal muscle used for EPHA2 and HER2-negative controls; normal colon used for EPHA2-positive controls; HER2-positive breast cancer used as HER2-positive controls; normal pancreas and testis used for IL13Rα2-negative and positive controls, respectively. Scale bar represents 100 mM, data represents 3 Biological replicates.
Extended Data Fig. 2 Defining EPHA2, HER2 and IL13Rα2 as immunotherapy targets in Group 3 primary and matched metastases or recurrence.
a, EPHA2 expression in human primary and metastatic Group 3 medulloblastomas; b, HER2 expression in human primary and metastatic Group 3 medulloblastoma; and c, IL13Rα2 is expressed in both human primary and metastatic compartments of Group 3 medulloblastoma, by expression microarray, n = 2 primary and 6 metastatic or recurrence group 3 medulloblastomas. All boxplot center lines show data median; box limits indicate the 25th and 75th percentiles; lower and upper whiskers extend 1.5 times the interquartile range (IQR) from the 25th and 75th percentiles, respectively. Outliers are represented by individual points. d, EPHA2 immunohistochemistry (IHC); e, HER2 IHC; and f, IL13Rα2 IHC staining analysis of paired human paediatric primary and metastases or recurrence in Group 3 medulloblastoma, representative membrane-staining H-scores displayed in lower corner. Scale bars represent 80 μM, data represents 3 biological replicates. g, H score of EPHA2 IHC (P = 0.6 two-sided Mann-Whitney U test); h, H score of HER2 IHC (P = 0.6 two-sided Mann-Whitney U test); i, H score of IL13Rα2 IHC (P = 0.9 two-sided Mann-Whitney U test) in n = 6 independent human paediatric primary and metastases or recurrence for Group 3 medulloblastoma samples; j, EPHA2, HER2 and IL13Rα2 protein expression in normal paediatric brain compartments. Scale bar represents 80 μM, numbers represent H-scores data represents 6 biological replicates.
Extended Data Fig. 3 Two doses of EPHA2-CAR T cells improves antitumour response in Group 3 medulloblastoma orthotopic xenograft models.
a, Hematoxylin-eosin (H&E) staining analysis of NSG mice xenografted with luciferase-expressing MDT-MMB, following one round of EPHA2 CAR T-cells and one versus two rounds of non-transduced T-cells, with associated IHC analysis for EPHA2 protein expression for the cerebellar tumour and matched spinal metastases, data represents 3 independent replicates. b, Measurement log Total Flux (photon/second) following one versus two rounds of intraventricular EPHA2 CAR T-cell therapy. ***P < 0.0005, **P < 0.005, *P < 0.05 by two-sided ANOVA followed by Tukey post hoc test, n = 5 MDT-MMB treated with EPHA2 CAR T-cells 1 round of therapy, n = 3 MDT-MMB treated with EPHA2 CAR T-cells 2 rounds of therapy, error bars represent SEM, centre line represents the mean. EPHA2 one round versus EPHA2 two rounds: Day 1: P = 0.3796; Day 120: P = 0.0009112; Day 150 P = 0.00141. c, Measurement of log Total Flux (photon/second) following one round of intraventricular versus i.v. EPHA2 CAR T-cell therapy. ***P < 0.0005, **P < 0.005, *P < 0.05, by two-sided ANOVA followed by Tukey post hoc test, n = 19 EPHA2 CAR T-cells delivered intraventricularly, n = 15 EPHA2 CAR T-cells delivered IV, error bars represent SEM, centre line represents mean. EPHA2 IV versus EPHA2 intraventricular: Day 1: P = 0.2038; Day 21: P = 0.2321; Day 42 P = 0.2731.
Extended Data Fig. 4 EPHA2, HER2 and IL13Rα2 are immunotherapy targets in PFA ependymoma.
a, EPHA2 differential expression across ependymoma subgroups (PF-EPN-A vs ST-EPN-RELA P = 0.05; PF-EPN-A vs SP-EPN P = 0.5207, two-sided Mann Whitney U test); b, HER2 differential expression across ependymoma subgroups (PF-EPN-A vs ST-EPN-RELA P = 0.0026; PF-EPN-A vs SP-EPN P = 0.146; SP-EPN vs ST-EPN-RELA P = 0.0027, two-sided Mann Whitney U test); and c, IL13Rα2 differential expression across ependymoma subgroups (PF-EPN-A vs ST-EPN-RELA P = 0.99; PF-EPN-A vs SP-EPN P = 0.7024, two-sided Mann Whitney U test), as compared by expression microarray, n = 54 PF-EPN-A, 15 SP-EPN, 31 ST-EPN-RELA. All boxplot centre lines show data median; box limits indicate the 25th and 75th percentiles; lower and upper whiskers extend 1.5 times the interquartile range (IQR) from the 25th and 75th percentiles, respectively. Outliers are represented by individual points. d, IHC membrane staining of EPHA2 in ependymoma primary tumour TMAs; e, IHC membrane staining of HER2 in ependymoma primary tumour TMAs; and f, IHC membrane staining of IL13Rα2 in ependymoma primary tumour TMAs, representative membrane-staining H-scores displayed in lower corner. Scale bars represent 80 μM. g, EPHA2, HER2 and IL13Rα2 protein expression in normal paediatric brain compartments, as comparative protein staining analysis in the normal brain. Scale bar represents 80 μM, numbers represent H-scores, data representative of 2 independent replicates. h, Summary of membrane-staining H score of EPHA2 IHC of human paediatric paired primary and recurrence for PFA ependymoma (P = 0.9 two-sided Mann-Whitney U test) i, Summary of membrane-staining H score of HER2 IHC of human paediatric paired primary and recurrence for PFA ependymoma (P = 0.9 two-sided Mann-Whitney U test) j, Summary of membrane-staining H score of IL13Rα2 IHC of human paediatric paired primary and recurrence for PFA ependymoma (P = 0.6 two-sided Mann-Whitney U test), n = 16 primary and 16 matched recurrences of biologically independent paired samples.
Extended Data Fig. 5 EPHA2 protein expression in primary paediatric ependymoma.
a, EPHA2 protein expression in primary paediatric ependymoma. Top panel displays spinal ependymoma, bottom panel displays RELA ependymoma. b, HER2 protein expression in primary paediatric ependymoma. Top panel displays spinal ependymoma, bottom panel displays RELA ependymoma. c, IL13Rα2 protein expression in primary paediatric ependymoma. Top panel displays spinal ependymoma, bottom panel displays RELA ependymoma. d, EPHA2 protein expression in primary paediatric, desmoplastic medulloblastoma by CHOP TMA. e, HER2 protein expression in primary paediatric, desmoplastic medulloblastoma by CHOP TMA. Scale bar represents 80 μM. Data representative of 3 biological replicates.
Extended Data Fig. 6 EPHA2 protein expression in primary paediatric ependymoma and matched recurrences.
a, EPHA2 protein expression in primary paediatric ependymoma and matched recurrences. b, HER2 protein expression in primary paediatric ependymoma and matched recurrences. c, IL13Rα2 protein expression in primary paediatric ependymoma and matched recurrences. d, EPHA2 protein expression in primary paediatric medulloblastoma. Top panel displays SHH medulloblastoma, bottom panel displays Group 4 medulloblastoma. e, HER2 protein expression in primary paediatric medulloblastoma. Top panel displays SHH medulloblastoma, bottom panel displays Group 4 medulloblastoma. f, IL13Rα2 protein expression in primary paediatric medulloblastoma. Top panel displays SHH medulloblastoma, bottom panel displays Group 4 medulloblastoma. Scale bar represents 80 μM. Data represents 3 biological replicates.
Extended Data Fig. 7 In vivo potency trial, experimental scheme.
Medulloblastoma cells (Med114FH or Med411FH) expressing eGFP-firefly luciferase (PDX-GFP-Luc) were xenografted into the cerebellum of NSG mice. BLI was performed to determine tumour engraftment, at which point a single dose of EPHA2 CAR T cells, TRI CAR T cells or non-transduced T cells, were delivered at dose range of 2.5×106, 5×106 or 10×106 a, intraventricularly by the lateral ventricle or b, IV by the tail vein. Tumour burden was monitored weekly by bioluminescence (BLI) until 8 weeks post-therapy, or humane endpoint. At endpoint, a terminal cardiac puncture was performed for complete blood collection, CSF removed from the cisterna magna, and CNS harvested.
Extended Data Fig. 8 In vivo potency trial endpoints of Med114FH PDXs treated with EPHA2 CAR T cells.
Bioluminescence (BLI) and endpoint Hematoxylin-eosin (H&E) staining analysis of NSG mice xenografted with luciferase-expressing Med114FH, infused a, via the lateral ventricle or b, IV with EPHA2 CAR T cells at dose range of 2.5×106, 5.0×106 and 10×106 as indicated (colour map for all images indicates radiance, min = 5×104, max = 5×106). Each column represents one mouse, each row represents the indicated time point and subsequent final BLI. Results representative of 2 independent replicates. c, Measurement of tumour burden over time expressed as Total Flux (photons/s) following one round of lateral ventricle versus IV EPHA2 CAR T cell therapy. ***P < 0.0005, **P < 0.005, *P < 0.05, by two-sided ANOVA followed by Tukey post hoc test, n = 3 EPHA2 CAR T cells delivered intrathecally, n = 3 EPHA2 CARs T cells delivered IV for each dose range, centre lines show the mean ± SEM performed in triplicate. Infusion of 2.5×106 EPHA2: Day 0 IV vs LV P = 0.807, Day 30 IV vs LV P = 0.00009, Day 60 IV vs LV P = 0.07; 5.0×106 EPHA2: Day 0 IV vs LV P = 0.03, Day 30 IV vs LV P = 0.00007, Day 60 IV vs LV P = 0.001; 10×106 EPHA2: Day 0 IV vs LV P = 0.003, Day 30 IV vs LV P = 0.00007, Day 60 IV vs LV P = 0.000015.
Extended Data Fig. 9 In vivo potency trial endpoints of Med411FH PDXs treated with EPHA2 CAR T cells.
Bioluminescence (BLI) and endpoint Hematoxylin-eosin (H&E) staining analysis of NSG mice xenografted with luciferase-expressing Med411FH, infused a, via the lateral ventricle or b, IV with EPHA2 CAR T cells at dose range of 2.5×106, 5.0×106 and 10×106 as indicated (colour map for all images indicates radiance, min = 5×104, max = 5×106). Each column represents one mouse, each row represents the indicated time point and subsequent final BLI. Results representative of 2 independent replicates. c, Measurement of tumour burden over time expressed as Total Flux (photons/s) following one round of lateral ventricle versus IV EPHA2 CAR T cell therapy. ***P < 0.0005, **P < 0.005, *P < 0.05, by ANOVA followed by Tukey post hoc test, n = 3 EPHA2 CAR T cells delivered intrathecally, n = 3 EPHA2 CARs T cells delivered IV for each dose range, centre lines show the mean ± SEM performed in triplicate. Infusion of 2.5×106 EPHA2: Day 0 IV vs LV P = 0.7, Day 30 IV vs LV P = 0.0004; 5.0×106 EPHA2: Day 0 IV vs LV P = 0.03, Day 30 IV vs LV P = 0.00009; 10×106 EPHA2: Day 0 IV vs LV P = 0.6, Day 30 IV vs LV P = 0.029.
Extended Data Fig. 10 Activation of CAR T cells - in vivo potency trial.
a, Heatmap of the normalized Z-scores of Human cytokines associated with T cell activation and augmentation, present in the blood circulation and CSF of NSG mice, in response to 2.5×106, 5.0×106 and 10×106 EPHA2 CAR T cells, TRI CAR T cells, or non-transduced T cells; delivered intraventricularly via the lateral ventricle, or IV via the tail vein. N = 36 EPHA2 (n = 16 blood and 16 CSF independent animal samples; n = 9 lateral ventricle and 9 intravenous CARs or T-cell infusions; n = 3 2.5×106, 3 5.0×106 and 3 10×106 CAR T-cell or non-transduced T-cell infusions., Samples were harvested 8 weeks post therapy, or at humane endpoint. b, IHC analysis of EPHA2 CAR T cell accumulation in mice treated within the associated in vivo potency trial, as indicated by CD3-positive protein expression. Top panel denotes mice infused IV with a dose range of 2.5×106, 5.0×106 and 10×106 EPHA2 CAR T cells, the bottom panel denotes mice infused intraventricularly via the lateral ventricle with a dose range of 2.5×106, 5.0×106 and 10×106 EPHA2 CAR T cells. Red arrows indicate EPHA2 T cell infiltration. Results representative of 2 independent replicates. c, IHC analysis of EPHA2 CAR T cell accumulation from archival FFPE samples of trial treated mice. The top panel denotes mice infused with non-transduced T cells, the bottom panel indicates mice treated with EPHA2 CAR T cells either intravenously (left), intraventricularly by the lateral ventricle (LV) (middle) or LV combined with Azacytidine (right) with a dose range of 5.0×106. Results representative of 2 independent replicates, red arrows indicate EPHA2 T cell infiltration.
Supplementary information
Supplementary Information
Supplementary Figures 1–15 and Supplementary Table 1.
Rights and permissions
About this article
Cite this article
Donovan, L.K., Delaidelli, A., Joseph, S.K. et al. Locoregional delivery of CAR T cells to the cerebrospinal fluid for treatment of metastatic medulloblastoma and ependymoma. Nat Med 26, 720–731 (2020). https://doi.org/10.1038/s41591-020-0827-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-0827-2
This article is cited by
-
Eph receptors and ephrins in cancer progression
Nature Reviews Cancer (2024)
-
Deciphering and advancing CAR T-cell therapy with single-cell sequencing technologies
Molecular Cancer (2023)
-
Chimeric antigen receptor T cells targeting cell surface GRP78 efficiently kill glioblastoma and cancer stem cells
Journal of Translational Medicine (2023)
-
CAR immune cells: design principles, resistance and the next generation
Nature (2023)
-
Overcoming on-target, off-tumour toxicity of CAR T cell therapy for solid tumours
Nature Reviews Clinical Oncology (2023)