Abstract
Coronary bifurcation intervention is common but complex. Progress in this field has been made in recent years with considerable contribution from the Asia Pacific (APAC) region. However, the standard of practice varies across the APAC region due to differences in culture, socioeconomic state and healthcare set-up. Practice may also differ from the rest of the world. Hence, a panel of experts was invited to discuss topics relevant to bifurcation intervention in order to make a concerted effort to achieve consensus that is applicable within the region and in line with available evidence.
Introduction
Asia Pacific (APAC) is the most populous region with over 60% of the world population living in 76 Asian and Oceanic countries. The differences in culture, tradition and socioeconomy across the region are vast, with great heterogeneity in healthcare infrastructure, clinical practice and progress in medical knowledge. This provides an excellent platform for mutual support, learning and collaboration in order to improve the standard of health care and facilitate advances in clinical practice and research.
Understanding the challenges of coronary bifurcation intervention1, 22 regional leaders in percutaneous coronary intervention (PCI) met in a two-day forum to discuss regional commonalities in treatment and best practice. This is also a concerted effort to achieve an APAC consensus. Two international experts were invited to share their experience and facilitate the discussion.
Aims
Although the European Bifurcation Club (EBC) consensus documents are comprehensive and applicable to the APAC region, differences between the APAC region and Europe may affect practices (Figure 1). There are also techniques and original data within the region which can complement the EBC consensus. Hence, the panel agreed that an APAC consensus document should be developed. This document is based on the 12th and 13th (left main [LM] intervention) EBC consensus documents2,3 and the 14th EBC consensus document which was only published during the preparation of this manuscript4. Special consideration is given to practices, data and techniques developed within the region.
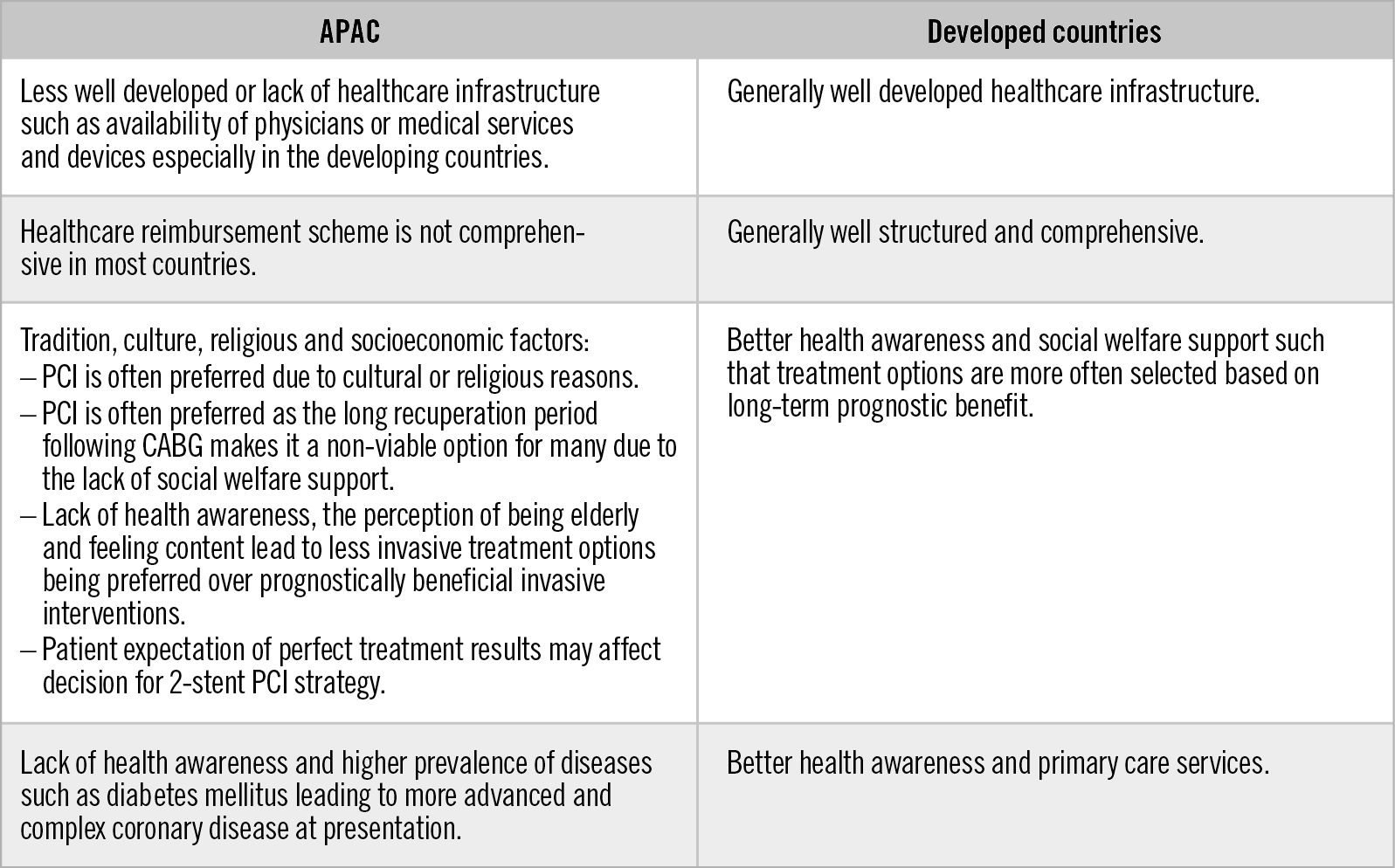
Figure 1. Challenges faced by APAC countries.
This document is intended to be a reference promoting systematic and evidence-based best practice relevant to the APAC region. It serves as a platform to identify challenges, share knowledge and skills, and foster research collaboration. It also aims to facilitate reimbursement for useful adjuvant technologies including intravascular imaging and physiology assessment in countries across the region. The panel intends to hold regular forums with updates to the document.
Special considerations for the Asia Pacific region
The panel discussion was mostly qualitative or based on consensus opinion. In many developing APAC countries, access of patients to health care remains unsatisfactory. The availability of PCI infrastructure including physicians and devices is limited or financially unaffordable. The treatment options for patients would differ from those in the West. Further, many patients would opt for PCI over coronary artery bypass graft surgery regardless of the prognostic implication due to cultural background, religious belief and lack of social welfare support. A Heart Team approach is becoming common practice in many APAC countries to encourage appropriate treatment.
Cardiovascular risk factors are more prevalent within the APAC region but health awareness among the general public and screening for cardiovascular risk factors are lacking. The Western Pacific is home to 37.4% of the world’s diabetics. The age-adjusted prevalence of diabetes mellitus among adults in the Western Pacific and Southern Asia is 8.6% and 10.1%, respectively, compared to 6.8% in Europe5. Alarmingly, half of these diabetics are undiagnosed. Hence, many cardiovascular risk factors only become apparent when the patients present with end-organ complications such as myocardial infarction (MI) or advanced diffuse multivessel coronary artery disease, with the consequence of technically more challenging PCI and less favourable outcome.
The perception of coronary artery calibre for people of Asian descent being smaller than that of Caucasians is unsupported by evidence and should not affect the definition or interventional strategies for coronary bifurcation. Few available studies found that the calibre of the major epicardial coronary artery was related to body surface area but not to ethnic descent6. Coronary artery calibre is also affected by age, dominance of the coronary system, gender, vasomotor tone and left ventricular size or mass6,7. However, smaller 2.0 mm diameter stents are not available in some non-APAC countries, presumably due to commercial or local regulatory reasons, but larger diameter stents are generally available within the APAC region.
Further, recent development of knowledge and techniques in bifurcation intervention within the APAC region, including intravascular imaging, invasive functional assessment, side branch (SB) protection methods and bifurcation stenting strategies, should be given careful consideration as most are relevant to clinical practice and future research.
RECOMMENDATION
The fundamentals of bifurcation PCI in the APAC region, including coronary artery calibre, are similar to the rest of the world with consideration given to more extensive or diffuse disease. The Heart Team approach is essential as the patient’s treatment choice may be determined by factors beyond clinical evidence.
Patient and lesion consideration
Bifurcation intervention strategy should not be based solely on anatomical characteristics. Consideration should be given to patient factors, significance of the SB involved and risk of SB compromise. The patient’s comorbidities, functional status, ability to complete a dual antiplatelet regimen, renal function or occupation and recreational pursuits may affect the decision on bifurcation treatment strategy.
The significance of an SB comprises four aspects - anatomical, physiological, clinical and prognostic. An SB could be considered anatomically important according to its diameter and length. Importantly, there is discordance between the angiographic severity of a stenosis and its functional significance8,9. This could be one limitation of bifurcation intervention trials in which lesion selection was based on anatomical criteria. Whether an SB lesion is physiologically important requires functional assessment by non-invasive imaging and/or invasive evaluation. Further, the clinical relevance of an SB has to be established. The burden of ischaemia or the amount of ischaemic myocardium and completeness of revascularisation should also be taken into consideration.
The approach to a bifurcation intervention should be systematic and the adoption of a complex bifurcation PCI strategy should be weighed against its potential drawbacks. Intravascular imaging would be helpful in better defining the anatomy and evaluating the likelihood of SB compromise. If the risk of SB compromise is high but there are factors precluding a complex treatment strategy, a “keep-it-open” approach can be adopted with a more elaborate SB protection technique, appropriate stent sizing and meticulous approach to main vessel (MV) treatment. If the SB is compromised, bail-out SB intervention should be kept simple and care taken to avoid disruption to the MV stent integrity. In the absence of any factor precluding PCI to a complex bifurcation with high risk of compromising the SB, an elective two-stent approach could be considered (Figure 2).
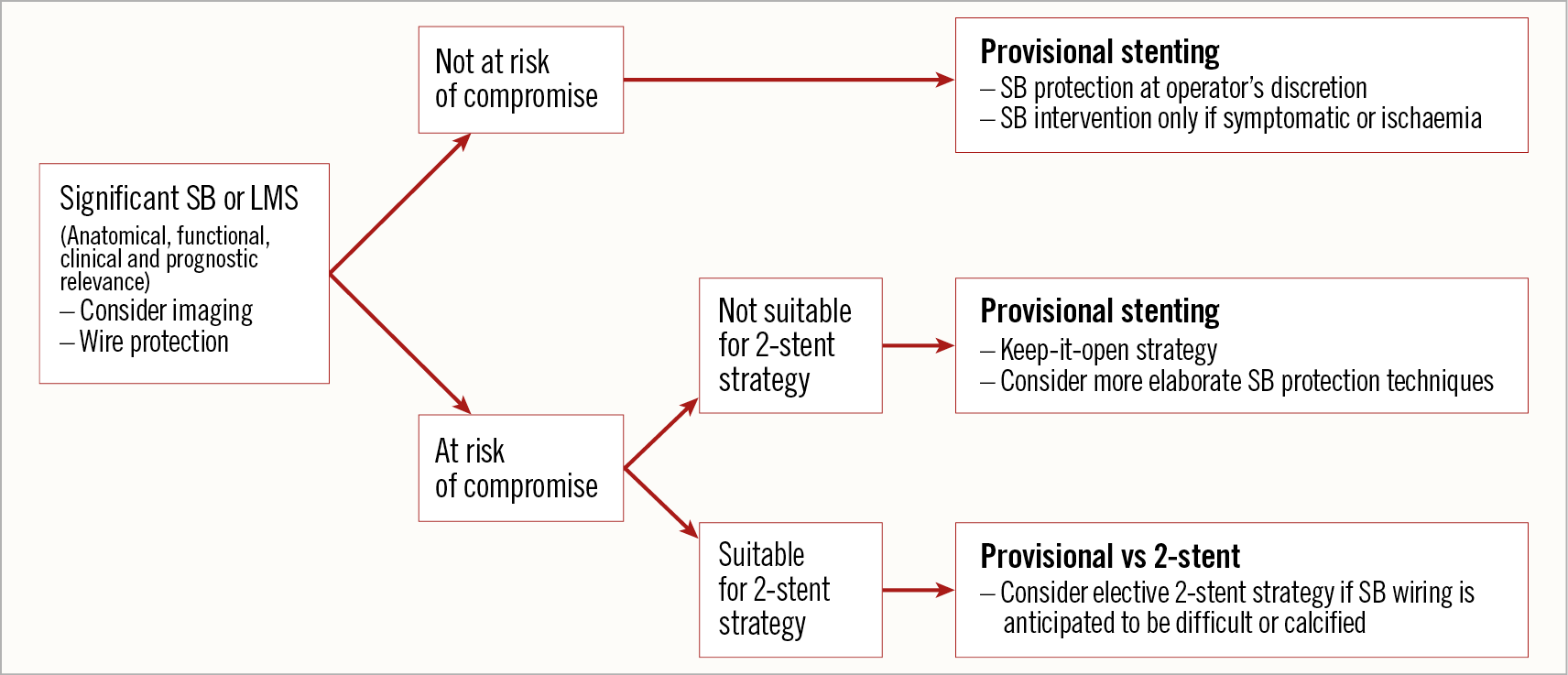
Figure 2. Systematic approach to bifurcation intervention.
RECOMMENDATION
Patient factors should be considered for the holistic approach. Selection of bifurcation strategy should be systematic and the significance of an SB should be based on anatomical, physiological, clinical and prognostic aspects.
Technical and procedural consideration
Most technical and procedural aspects of bifurcation intervention have been well described in the EBC documents2, including LM intervention3 and the use of intravascular imaging10,11. However, there are some areas with data and techniques relevant to the practice within the APAC region.
VASCULAR ACCESS
Most bifurcation lesions can be effectively treated transradially using a 6 Fr guide catheter but, to accommodate more devices, a 7 Fr guide catheter system is feasible in patients within the APAC region. The trend to miniaturise transradial PCI initiated by the Slender Club Japan is gradually extending beyond the APAC region. This has helped to facilitate the distal radial artery approach which is also feasible for patients within the APAC region.
SIDE BRANCH PROTECTION TECHNIQUES
Some SB protection techniques that are more elaborate than the conventional jailed wire technique (JWT) have been developed, because SB occlusion can occur in up to 9% of bifurcation PCI cases despite the JWT, and recanalisation can be unsuccessful12,13. The JWT does not reduce the incidence of SB occlusion, which increases the risk of stent thrombosis (ST) by sixfold and cardiac death by fourfold13. The risk of cardiac death remains higher even after re-establishing blood flow.
Besides techniques such as the jailed balloon technique (JBT) and modified jailed semi-inflated balloon, the modified jailed balloon technique (M-JBT) by Saito et al has a lower eccentricity index than the conventional JBT14. The initial study showed that only a few cases with M-JBT required SB stenting without any SB loss and severe dissection acutely or unexpected intervention after six months.
Although there has been no randomised controlled trial (RCT), these techniques could be considered especially when it is imperative to preserve the patency of a significant SB. Care should be taken to ensure that the stent segment proximal to the SB is well expanded and apposed when using these techniques.
PROVISIONAL STENTING
Provisional stenting is the default strategy for bifurcation intervention2 but some aspects remain unclear, including SB intervention, the effects of evolving drug-eluting stent (DES) technology and newer provisional or two-stent techniques.
TREATMENT OF SB IN PROVISIONAL STENTING
Provisional stenting may cause carina or plaque shift leading to SB ostial stenosis in 10–40% of the cases; however, the treatment remains uncertain due to the discordance between the angiographic appearance and the functional significance of SB disease8,9.
Using balloon inflation to open the stent cell over the SB can cause stent distortion, carina shift into the MV and malapposition of struts opposite the SB ostium. However, unapposed stent struts at the SB ostium are common without SB treatment and might lead to uncovered struts, fibrin deposition, thrombus formation and late ST15. The kissing balloon technique (KBT) can reduce the number of uncovered struts and the incidence of thrombus formation15.
Although an SB fractional flow reserve (FFR) <0.75 or myocardial ischaemia is more common in provisional stenting without KBT, the incidence of significant ischaemia >10% of left ventricular myocardium is not more frequent, and routine KBT does not improve clinical outcome16. SB treatment with KBT and stenting or routine KBT in non-diseased SB could lead to a higher incidence of target lesion failure (TLF) in the MV17,18. KBT can increase the incidence of MV restenosis by threefold19 due to elliptical deformation of the stent, oversizing of the proximal stent segment that increases wall stress with intimal hyperplasia or edge dissection, increased strut malapposition proximal to the KBT segment and disruption of strut configuration and polymer coatings.
The proximal optimisation technique (POT)2,3 can correct stent deformation, eccentricity and malapposition following KBT but not abolish stent overexpansion or reverse stent edge dissection. POT does not require high-pressure balloon inflation but it is essential to achieve appropriate stent expansion and apposition2. Hence, a semi-compliant balloon with a larger expansion range is preferred over a non-compliant balloon20.
Re-POT can optimise the result of provisional stenting by reducing SB ostium strut obstruction and global strut malapposition whilst maintaining stent circular geometry without arterial overstretch21. Re-POT is effective and technically less demanding, with early experience showing satisfactory short-term outcomes.
RECOMMENDATION
More elaborate SB protection strategies can be considered to preserve vessel patency in provisional stenting. SB treatment and KBT should be performed only when clinically important SB is functionally compromised following provisional stenting.
PROVISIONAL VERSUS TWO-STENT STRATEGY
Older RCTs that favour a provisional versus a two-stent strategy involved mainly the first-generation DES using crush, T-stenting or culotte techniques. The two-stent strategy has a higher rate of major adverse cardiovascular events (MACE) but medium-term events were related mainly to periprocedural MI22.
The Nordic-Baltic Bifurcation Study IV reported at EuroPCR 2015 showed that provisional stenting trended to have a higher MACE rate than a two-stent strategy, especially with first-generation DES. A Korean patient-level pooled analysis found a higher three-year MACE rate with a two-stent strategy than provisional stenting only among those who received first-generation DES23. The EBC TWO study also found similar outcomes between the provisional T-stenting and culotte techniques using a Biolimus-eluting stent24.
The DKCRUSH-II trial, which involved patients with true bifurcation lesions (Medina 1,1,1 and 0,1,1) across seven APAC countries, found similar one-year composite cardiac death, MI and target vessel revascularisation (TVR) rates between provisional stenting and the double-kissing crush (DK crush) technique25. Importantly, DK crush had sustained lower restenosis and TVR rates over five years26. Further, DKCRUSH-V found that DK crush had a lower one-year TLF rate than provisional stenting in true LM bifurcation lesions27. Another RCT comparing DK crush, culotte or T-stenting also found higher short-term restenosis and MACE rates with provisional stenting28.
Therefore, a two-stent strategy, especially with the DK crush technique and current-generation DES, may confer a similar outcome to provisional stenting when optimally performed.
TECHNIQUES IN TWO-STENT STRATEGY
The two-stent strategy is thought to be more commonly adopted across the APAC region. Among the panel, only 39% adopt a two-stent strategy in <10% of their bifurcation cases. The remaining perform a two-stent strategy in 11 to 50% of their bifurcation cases. In the COBIS II registry, a two-stent strategy was adopted in 20.8% of non-LM and 40.3% of LM cases29.
The DK crush technique devised by Dr Chen30 is the first two-stent technique proven to show superior clinical outcomes. The DKCRUSH-1 trial31 found lower MACE with the DK crush than with the classic crush technique. Although DK crush was technically more demanding, KBT was successfully performed in all of the cases, which might explain its improved efficacy. DK crush can also be performed regardless of the bifurcation angle.
The DKCRUSH-III trial32 exclusively involved unprotected true distal LM bifurcation lesions using second-generation everolimus or sirolimus DES. The occurrence of SB in-stent restenosis at eight months was less frequent with DK crush than with culotte, and involved mainly the ostium of the left circumflex artery (LCx). The 12-month MACE rate was also higher in the culotte group.
Although more and longer-term data are needed, it may be reasonable to consider DK crush as the preferred two-stent technique. Some experts have recommended sticking with the technique most familiar to the operator as this is most likely to achieve an optimal result. It is important to note that proximal cell crossing is required for the classic or DK crush technique. It is also imperative to optimise two-stent techniques with KBT followed by POT2.
ELECTIVE TWO-STENT STRATEGY
An elective two-stent strategy may be needed to secure the SB in complex bifurcation lesions2. A few clinical13, angiographic12,13,33,34 and intravascular imaging35,36 features associated with SB compromise have been described (Figure 3). Risk prediction models such as DEFINITION34, RESOLVE12 and baseline V-RESOLVE33 have also been validated and can guide the interventional strategy.
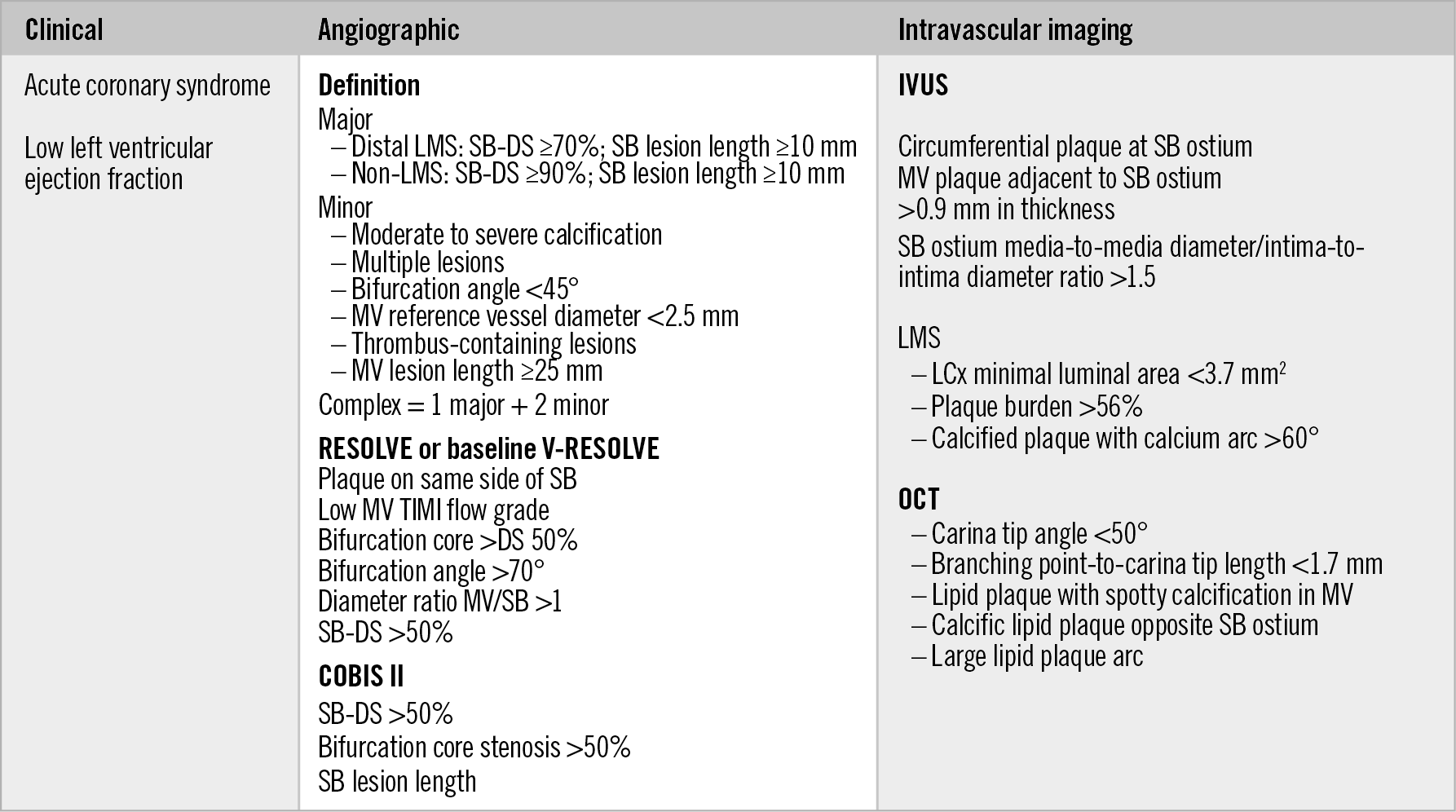
Figure 3. Features associated with SB compromise.
An elective two-stent strategy could be considered in SBs that are functionally significant, clinically relevant and prognostically important. A thoughtful approach should be adopted in the planning and execution of the treatment strategy (Figure 2).
RECOMMENDATION
An elective two-stent strategy could be adopted in selected true bifurcation cases where the DK crush technique can be considered, although the physician’s familiarity with a certain technique should also be taken into consideration.
FFR IN BIFURCATION LESIONS
Functional assessment of the SB following MV stenting can be affected by vessel wall oedema, haematoma, thrombus or plaque shift which can remodel with time2. Tracking of a pressure wire through MV stent struts can be unsuccessful in 10% of cases, although this can be improved by KBT37. The SB can also be dissected by the pressure wire and, although not recommended, some avoid pressure wire tracking by placing it in the SB, as in the JWT.
There is discordance between the angiographic appearance and the functional significance of SB disease. Following provisional stenting, only 27% of SBs with stenosis of >75% have an FFR <0.75; none of the SBs with stenosis <75% was functionally significant9. In contrast, approximately 13% of jailed SBs with angiographically insignificant stenosis have an FFR <0.8038. The DKCRUSH-VI study showed that an FFR-guided strategy reduced the need for SB stenting and had similar clinical outcome to angiography-guided treatment following provisional stenting37.
Clinical outcome can be affected by the burden of ischaemia and not only by functional abnormality as demonstrated by FFR. In left anterior descending artery (LAD)/diagonal bifurcation intervention, diagonal artery occlusion leads to less angina, fewer electrocardiographic changes and less arrhythmogenic potential than LAD occlusion39. A recent study has established that 97% of LM SBs but only 21% of non-LM SBs supply myocardium with percentage fractional myocardial mass (%FMM) ≥10%40. The SBs that supply myocardium with %FMM ≥10% can be identified by vessel length ≥73 mm. Further, an LCx FFR of ≤0.80 following LM provisional stenting was found to be associated with higher rates of five-year TLF41.
Hence, functional assessment of the SB should include the presence of ischaemia, ischaemic burden, and perhaps anatomic burden. In the absence of definitive prognostic benefit from SB intervention, a more conservative FFR of ≤0.75 is considered by some to be a reasonable treatment threshold. Recent data suggest that the non-hyperaemic pressure ratio can be used to assess SB stenosis; however, further studies are needed for their prognostic validation.
INTRACORONARY IMAGING
Intravascular ultrasound (IVUS)11 and optical coherence tomography (OCT)10 have been well appraised by the EBC to optimise bifurcation PCI.
IVUS-guided bifurcation intervention reduces MACE in unprotected LM or bifurcation intervention for up to seven years42,43. RCTs on OCT-guided bifurcation intervention are ongoing. The OPINION trial included a large proportion of bifurcation lesions and found that OCT-guided PCI conferred similar one-year outcome to IVUS-guided PCI. The result might be further optimised by three-dimensional OCT10.
The use of intravascular imaging is often limited by cost, especially in the APAC region. Regional consensus can facilitate and align the practice and reimbursement criteria especially for complex PCI including bifurcation intervention.
RECOMMENDATION
Intravascular imaging should be advocated and functional assessment can be considered in both LM and non-LM bifurcation intervention.
LEFT MAIN STEM (LM) BIFURCATION
The EBC consensus documents provide comprehensive guidance for optimal LM intervention2,3. Intravascular imaging is mandatory to ensure optimal outcome. During functional assessment, consideration should be given to downstream lesions; a significant lesion in one branch could spuriously increase the FFR in the other.
Most distal LM lesions are true bifurcation lesions since distal LM plaque extends into the LAD and LCx in 90% and 66% of the cases, respectively44. Only 9% of LAD and 17% of LCx ostial lesions are without LM involvement. The discrepancy between the diameter of the LM and that of the LAD or LCx is often substantial and will influence the stent choice. Resistance of the stent to compression is also important in order to minimise guide catheter-related stent deformity. Following LM PCI, restenosis is more likely to occur at the LCx ostium, especially with two-stent techniques, and remains susceptible to recurrence even after repeat intervention27,32. Importantly, almost all LAD and LCx supply blood to the myocardium with %FMM ≥10%, which can be prognostically relevant40.
Since KBT in provisional stenting does not alter the clinical outcome16, it is only recommended for selected cases3. Compared to provisional stenting or culotte, DK crush has a lower MACE rate27,32. However, physicians’ familiarity with stenting techniques and ensuring an optimal minimal stent area are paramount for better outcome.
Physicians in the APAC region may be faced with more patients with LM disease opting for PCI. Selection of patients should be based on current clinical evidence and a multidisciplinary Heart Team approach. The new risk stratification score II (NERS II), incorporating clinical and anatomical variables, is more sensitive and specific than the SYNTAX score in predicting MACE, which may help to guide patient selection45.
RECOMMENDATION
A Heart Team approach guided by clinical criteria should be adopted when counselling patients for LM disease treatment. Intravascular imaging should be mandated during PCI while the DK crush technique could be considered for true bifurcation lesions.
STENT CHOICE CONSIDERATIONS
There are differences in biomechanical properties and performance among the different stent platforms depending on the stenting technique but their impact on clinical outcome is uncertain. Although most metallic platforms can be expanded within a predefined threshold in cases where there is a large discrepancy in the vessel size proximal and distal to the SB, their structure, durability and polymer integrity for bifurcation lesions are unknown. In addition, dedicated bifurcation stent technologies are also evolving.
Present and future
In understanding the challenges within the APAC region, the current consensus focuses on areas relevant to regional practices. The Heart Team approach to patient management and counselling using established criteria is advocated, especially when tradition or cultural beliefs are in conflict with evidence-based practice. Challenging and complex bifurcation lesions should be approached systematically by establishing the significance of the SB and its risk of being compromised based on known factors, with consideration given to protection techniques and, in some cases, an elective two-stent strategy.
Much research is needed in most of the areas discussed. Development of standardised and robust lesion classification that would influence clinical outcome and allow selection of the bifurcation treatment technique will help to guide treatment and facilitate research. Intravascular imaging criteria to define optimal bifurcation intervention are also lacking. The optimal dual antiplatelet regimen after bifurcation intervention remains uncertain. A region-wide survey would help to identify the differences among the countries and focus effort relevant to individual countries and within the APAC region.
Conclusions
Although the sentiment and clinical practice within the APAC region for bifurcation intervention are largely similar to the rest of the world, there remain differences due to culture, socioeconomy and healthcare provision. Consideration should be given to the anatomical, functional, clinical and prognostic relevance of the lesion, adopting a systematically thought-through interventional strategy. Clinical data, expertise and research efforts within the APAC region could contribute to progress in bifurcation intervention. This first concerted effort sets the scene for continuing development of future regional consensus, building the network for research collaboration and establishing partnership beyond the APAC region.
Acknowledgements
The panel is grateful to Abbott Vascular (Singapore) for sponsoring the forum.
Conflict of interest statement
S.A. Harding has acted as proctor for Boston Scientific, Medtronic and Abbott Vascular and received speaker honoraria from Boston Scientific, Medtronic, Abbott Vascular, Asahi Intecc and Medtronic. N. Jepson has received speaker honoraria from Abbott Vascular, Volcano and Philips and acts as a proctor for Abbott Vascular and Philips. G. Guagliumi has received honoraria for proctoring and speaking from Boston Scientific, and Abbott Vascular. S. Uemura has received speaker honoraria from Abbott Vascular Japan and Terumo. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.