Abstract
Background
The impact of obesity on the incidence of perioperative myocardial infarction/injury (PMI) and mortality following non-cardiac surgery is not well understood.
Methods
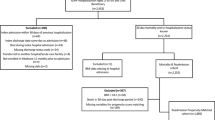
We performed a prospective diagnostic study enrolling consecutive patients undergoing non-cardiac surgery, who were considered at increased cardiovascular risk. All patients were screened for PMI, defined as an absolute increase from preoperative to postoperative sensitive/high-sensitivity cardiac troponin T (hs-cTnT) concentrations. The body mass index (BMI) was classified according to the WHO classification (underweight< 18 kg/m2, normal weight 18–24.9 kg/m2, overweight 25–29.9 kg/m2, obesity class I 30–34.9 kg/m2, obesity class II 35–39.9 kg/m2, obesity class III > 40 kg/m2). The incidence of PMI and all-cause mortality at 365 days, both stratified according to BMI.
Results
We enrolled 4277 patients who had undergone 5413 surgeries. The median BMI was 26 kg/m2 (interquartile range 23–30 kg/m2). Incidence of PMI showed a non-linear relationship with BMI and ranged from 12% (95% CI 9–14%) in obesity class I to 19% (95% CI 17–42%) in the underweight group. This was confirmed in multivariable analysis with obesity class I. showing the lowest risk (adjusted OR 0.64; 95% CI 0.49–0.83) for developing PMI. Mortality at 365 days was lower in all obesity groups compared to patients with normal body weight (e.g., unadjusted OR 0.54 (95% CI 0.39–0.73) and adjusted OR 0.52 (95% CI 0.38–0.71) in obesity class I).
Conclusion
Obesity class I was associated with a lower incidence of PMI, and obesity in general was associated with a lower all-cause mortality at 365 days.




Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- ECG:
-
Electrocardiography
- ESC:
-
European Society of Cardiology
- ESA:
-
European Society of Anesthesiology
- HR:
-
Hazard ratio
- Hs-cTnT:
-
High-sensitivity cardiac troponin T
- IQR:
-
Interquartile range
- s-cTnI:
-
Sensitive cardiac troponin I
- METS:
-
Metabolic equivalent
- OR:
-
Odds ratio
- PMI:
-
Perioperative myocardial injury
- RCRI:
-
Revised Cardiac Risk Index
- TIA:
-
Transient ischemic attack
- TNF-α:
-
Tumor necrosis factor-α
- WHO:
-
World Health Organization
References
Data and statistics. 2019. https://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics. Accessed 27 Jan 2019
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL (2018) Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 319(16):1723–1725. https://doi.org/10.1001/jama.2018.3060
Ortega FB, Lavie CJ, Blair SN (2016) Obesity and cardiovascular disease. Circ Res 118(11):1752–1770. https://doi.org/10.1161/CIRCRESAHA.115.306883
Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD (2003) Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 63(3):793–808. https://doi.org/10.1046/J.1523-1755.2003.00803.X
Buettner HJ, Mueller C, Gick M et al (2007) The impact of obesity on mortality in UA/non-ST-segment elevation myocardial infarction. Eur Heart J 28(14):1694–1701. https://doi.org/10.1093/eurheartj/ehm220
Valentijn TM, Galal W, Tjeertes EKM, Hoeks SE, Verhagen HJ, Stolker RJ (2013) The obesity paradox in the surgical population. Surgeon 11(3):169–176. https://doi.org/10.1016/j.surge.2013.02.003
Puelacher C, Lurati Buse G, Seeberger D et al (2018) Perioperative myocardial injury after noncardiac surgery. Circulation 137(12):1221–1232. https://doi.org/10.1161/CIRCULATIONAHA.117.030114
Devereaux PJ, Biccard BM, Sigamani A et al (2017) Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA 317(16):1642. https://doi.org/10.1001/jama.2017.4360
Thygesen K, Alpert JS, Jaffe AS et al (2018) Fourth universal definition of myocardial infarction. Circulation. https://doi.org/10.1161/CIR.0000000000000617
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. PLoS Med 4(10):1623–1627. https://doi.org/10.1371/journal.pmed.0040296
World Health Organization (2000) Obesity: preventing and managing the global epidemic: report of a WHO consultation. World Health Organization, Geneva
Kristensen SD, Knuuti J, Saraste A et al (2014) ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management. Eur J Anaesthesiol 31:517–573. https://doi.org/10.1097/EJA.0000000000000150
Lee TH, Marcantonio ER, Mangione CM et al (1999) Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. https://www.circulationaha.org. Accessed 27 Aug 2018
Reichlin T, Hochholzer W, Bassetti S et al (2009) Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 361(9):858–867. https://doi.org/10.1056/NEJMoa0900428
Twerenbold R, Boeddinghaus J, Nestelberger T et al (2017) Clinical use of high-sensitivity cardiac troponin in patients with suspected myocardial infarction. J Am Coll Cardiol 70(8):996–1012. https://doi.org/10.1016/J.JACC.2017.07.718
Wildi K, Nelles B, Twerenbold R et al (2016) Safety and efficacy of the 0 h/3 h protocol for rapid rule out of myocardial infarction. Am Heart J 181:16–25. https://doi.org/10.1016/J.AHJ.2016.07.013
Kavsak PA, MacRae AR, Yerna M-J, Jaffe AS (2009) Analytic and clinical utility of a next-generation, highly sensitive cardiac troponin i assay for early detection of myocardial injury. Clin Chem 55(3):573–577. https://doi.org/10.1373/clinchem.2008.116020
Hicks KA, Tcheng JE, Bozkurt B et al (2015) 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials. Circulation 132(4):302–361. https://doi.org/10.1161/CIR.0000000000000156
Agresti A, Coull BA (1998) Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat 52(2):119–126. https://doi.org/10.1080/00031305.1998.10480550
Bagley SC, White H, Golomb BA (2001) Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol 54(10):979–985. https://doi.org/10.1016/s0895-4356(01)00372-9
Valentijn TM, Galal W, Hoeks SE, van Gestel YR, Verhagen HJ, Stolker RJ (2013) Impact of obesity on postoperative and long-term outcomes in a general surgery population: a retrospective cohort study. World J Surg 37(11):2561–2568. https://doi.org/10.1007/s00268-013-2162-y
Davenport DL, Xenos ES, Hosokawa P, Radford J, Henderson WG, Endean ED (2009) The influence of body mass index obesity status on vascular surgery 30-day morbidity and mortality. J Vasc Surg 49(1):140–147.e1. https://doi.org/10.1016/j.jvs.2008.08.052
Dindo D, Muller MK, Weber M, Clavien P-A (2003) Obesity in general elective surgery. Lancet 361(9374):2032–2035. https://doi.org/10.1016/S0140-6736(03)13640-9
Haslam DW, James WPT (2005) Obesity. Lancet 366(9492):1197–1209. https://doi.org/10.1016/S0140-6736(05)67483-1
Packer M (2018) Epicardial adipose tissue may mediate deleterious effects of obesity and inflammation on the myocardium. J Am Coll Cardiol 71(20):2360–2372. https://doi.org/10.1016/J.JACC.2018.03.509
Hopkins T, Ouchi N, Shibata R, Walsh K (2007) Adiponectin actions in the cardiovascular system. Cardiovasc Res 74(1):11–18. https://doi.org/10.1016/j.cardiores.2006.10.009
Roman M, Monaghan A, Serraino GF et al (2019) Meta-analysis of the influence of lifestyle changes for preoperative weight loss on surgical outcomes. BJS 106(3):181–189. https://doi.org/10.1002/bjs.11001
Devereaux PJ, Duceppe E, Guyatt G et al (2018) Dabigatran in patients with myocardial injury after non-cardiac surgery (MANAGE): an international, randomised, placebo-controlled trial. Lancet 391(10137):2325–2334. https://doi.org/10.1016/S0140-6736(18)30832-8
Suthahar N, Meijers WC, Ho JE et al (2018) Sex-specific associations of obesity and N-terminal pro-B-type natriuretic peptide levels in the general population. Eur J Heart Fail 20(8):1205–1214. https://doi.org/10.1002/ejhf.1209
Acknowledgement
Thomas Wolff: Division of Vascular Surgery, University Hospital Basel, University of Basel, Switzerland; Karin Wildi: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Alessandro Genini: Department of Anaesthesiology, University Hospital Basel, University of Basel, Switzerland; Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Raphael Twerenbold: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Lorraine Sazgary: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Luca Koechlin: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Desiree Wussler: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Tobias Breidthardt: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Dayana Flores: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Stefan Osswald: Cardiovascular Research Institute Basel (CRIB) and Department of Cardiology, University Hospital of Basel, University of Basel, Switzerland; Katharina Rentsch: Department of Laboratory Medicine, University Hospital Basel, University of Basel, Switzerland.
Funding
This study was supported by research grants from the Swiss National Science Foundation, the Swiss Heart Foundation, the Stiftung Für Kardiovaskuläre Forschung Basel, the University of Basel, the University Hospital Basel, Abbott and Roche, Forschungsfond Kantonsspital Aarau.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
Mr. Christian Puelacher PhD, MD has received research support from Roche Diagnostic. Prof. Mueller has received research support from the Swiss National Science Foundation, the Swiss Heart Foundation, the European Union, the Kommission für Technologie & Innovation, the Stiftung für kardiovaskuläre Forschung Basel, the University of Basel, the University Hospital Basel, Abbott, Beckman Coulter, Biomerieux, Brahms, Idorsia, Novartis, Ortho Clinical Diagnostics, Quidel, Roche, Sanofi, Siemens, Singulex, Sphingotec, as well as speaker honoraria/consulting honoraria from Acon, Amgen, Astra Zeneca, Bayer, Biomerieux, Boehringer Ingelheim, BMS, Brahms, Novartis, Roche, Sanofi, Siemens, and Singulex. Dr. Twerenbold has received research support from the Swiss National Science Foundation (P300PB-167803_1), the Swiss Heart Foundation, the Swiss Society of Cardiology, the University Hospital Basel, and the Cardiovascular Research Foundation; and has received speaker honoraria/consulting honoraria from Abbott, Amgen, Brahms, Roche, Siemens, and Singulex. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hidvegi, R., Puelacher, C., Gualandro, D.M. et al. Obesity paradox and perioperative myocardial infarction/injury in non-cardiac surgery. Clin Res Cardiol 109, 1140–1147 (2020). https://doi.org/10.1007/s00392-020-01605-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01605-0