Abstract
Aims: The aim of this study was to describe the midterm outcomes in nonagenarians undergoing transcatheter aortic valve implantation (TAVI).
Methods and results: Based on the French administrative hospital discharge database, the study collected information for all consecutive patients with aortic stenosis (AS), and specifically those treated with TAVI between 2010 and 2018. Cox regression was used for the analysis of predictors of events. We compared patients according to their age. Within the studied period, 71,095 patients older than 90 years with AS were identified. After matching on baseline characteristics, TAVI was associated with lower rates of a combined outcome of all-cause death, rehospitalisation for heart failure and stroke (relative risk [RR] 0.58, p<0.001) in comparison with matched nonagenarians with AS treated medically. During follow-up (median 161 days, interquartile range 13-625), the combined outcome occurred more frequently in nonagenarians (RR 1.22, p<0.01) who had a TAVI than in younger patients undergoing this procedure. All-cause death was reported in 17.6% versus 14.5% of nonagenarians, rehospitalisation for heart failure in 21.3% versus 18.2%, and stroke in 3.7% versus 2.9% (p<0.01 for all parameters). We identified the Charlson comorbidity index, heart failure, atrial fibrillation, stroke, vascular disease, cognitive impairment and denutrition as independent predictors of adverse outcomes in nonagenarians undergoing TAVI.
Conclusions: Among nonagenarians with AS, patients treated with TAVI had a lower risk of cardiovascular events than matched patients treated medically. The patients undergoing a TAVI at this age were often highly selected; the procedure was associated with acceptable long-term outcomes.
Introduction
Transcatheter aortic valve implantation (TAVI) is considered the preferred treatment for severe aortic stenosis (AS) in inoperable and high surgical risk patients1. Recent data showed that TAVI is non-inferior to surgery in intermediate- and low-risk patients2. At the other end of the spectrum, the development of TAVI offered a solution for AS treatment in patients often declined for conventional surgery, such as nonagenarians3,4.
Nonagenarians are at higher risk for open heart surgery1,4. When a TAVI indication is considered, life expectancy and future quality of life in particular should be taken into account. However, in current large randomised clinical trials, nonagenarians account for only a small fraction of patients and therefore long-term outcomes remain poorly explored2. The feasibility of TAVI procedures in this cohort has already been reported with limited follow-up5.
The French programme de médicalisation des systèmes d’information (PMSI), a mandatory administrative database, offers the opportunity to assess comprehensive data on all TAVI performed at a nationwide level6. We planned to evaluate the impact of TAVI performed in patients >90 years old with AS and describe clinical outcomes in this population in comparison with younger patients.
Methods
STUDY DESIGN
This longitudinal cohort study was based on the national hospitalisation database covering hospital care from the entire French population. The data for all patients admitted with AS in France were collected from the PMSI database. Each hospitalisation is encoded in a standardised data set, which includes information about the patient (age and sex), pathologies, and procedures. Identified diagnoses are coded according to the International Classification of Diseases, Tenth Revision (ICD-10). All medical procedures are recorded according to the national nomenclature, classification commune des actes médicaux (CCAM). The reliability of PMSI data has already been assessed3,7.
The study was conducted retrospectively and, as patients were not involved in its conduct, there was no impact on their care. Ethical approval was not required, as all data were anonymised. Procedures for data collection and management were approved by the Commission Nationale de l’Informatique et des Libertés, the independent national ethics committee protecting human rights in France, which ensures that all information is kept confidential and anonymous, in compliance with the Declaration of Helsinki (authorisation number 1897139).
STUDY POPULATION
From January 2010 to December 2018, 487,085 adults (age ≥18 years) were hospitalised with a diagnosis of AS. We restricted the analysis to patients admitted after 2010, with at least two years of past events to define comorbidities. For the analysis of TAVI procedures, we included all adults with a single percutaneous procedure (CCAM code: DBLF001). Patients treated with surgical aortic valve replacement (SAVR) and those treated with surgical TAVI were excluded from the analysis (Figure 1). The comparison group of nonagenarians was composed of all patients with AS without a TAVI procedure. We used the Charlson comorbidity index and the claims-based frailty indicator to assess patient clinical status8,9,10. We aimed to compare 1) nonagenarians undergoing TAVI versus matched nonagenarians who had medical treatment, and 2) nonagenarians undergoing TAVI versus other classes of age in patients undergoing percutaneous TAVI (Figure 1). Patients older than 90 years were divided into two groups according to their TAVI status (TAVI procedure or non-TAVI procedure) after exclusion of 128 patients treated with SAVR. Balloon aortic valvuloplasty only was also identified and was not a criterion of exclusion. We divided the whole population of patients with a TAVI procedure into two groups according to age: <90 years old and ≥90 years old.
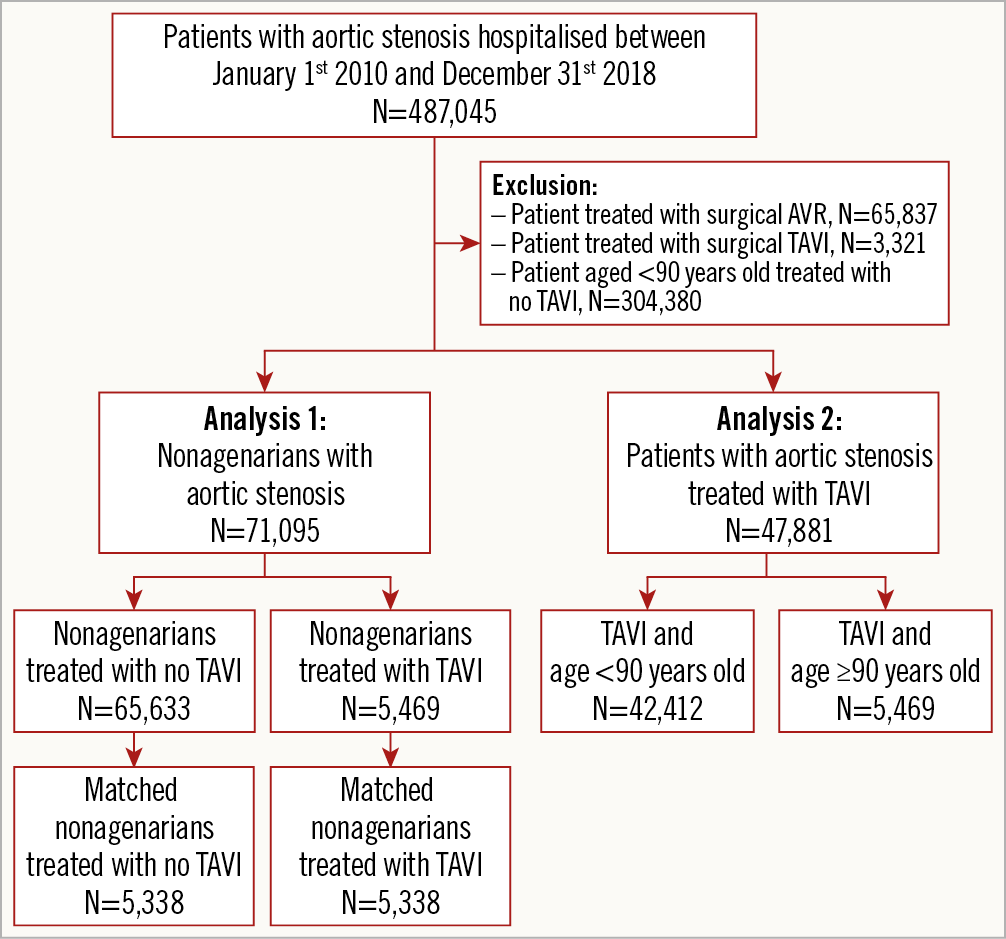
Figure 1. Flow chart of the study population.
OUTCOMES
The endpoints were evaluated with follow-up starting from the date of TAVI implantation until the date of each specific outcome or the date of last news in the absence of the outcome. We evaluated the incidence of all-cause death, cardiovascular death, ischaemic stroke, rehospitalisation for heart failure, and pacemaker implantation in nonagenarians undergoing TAVI versus matched nonagenarians who had medical treatment and versus younger patients undergoing TAVI. All these outcomes were evaluated separately to be consistent with the Valve Academic Research Consortium-2 consensus document. Information on outcomes during follow-up was obtained by analysing the PMSI codes for each patient11. Mode of death (cardiovascular or non-cardiovascular) was identified based on the main diagnosis during hospitalisation resulting in death. Rehospitalisation was considered to be due to heart failure when heart failure was recorded as the first diagnosis. We also evaluated a combined cardiovascular outcome in our analysis, which was a combination of cardiovascular death, rehospitalisation for heart failure, and ischaemic stroke during follow-up.
STATISTICAL ANALYSIS
Patients were divided into two groups according to their age (<90 years, ≥90 years). Qualitative variables are described using counts and percentages and continuous quantitative variables as means±standard deviation. For baseline characteristics, either chi-square tests or Fisher’s exact tests were performed, as appropriate.
Owing to the non-randomised nature of the study, treatment selection bias and potential confounding were reduced by using propensity score matching to account for significant differences in baseline characteristics when comparison between nonagenarians with or without TAVI was performed. Propensity scores were calculated using logistic regression with TAVI as the dependent variable. The propensity score included variables from baseline characteristics and year of implantation (Supplementary Appendix 1). For each patient treated with TAVI, a propensity score-matched patient with no TAVI was selected (1:1) using the one-to-one nearest neighbour method (with a calliper of 0.001 of the SD of the propensity score on the logit scale) and no replacement. We assessed the distributions of demographic data and comorbidities in the TAVI and no TAVI cohorts with standardised mean differences. A standardised mean difference of 0.05 or less indicated a negligible difference between the means of the two cohorts.
For the outcomes analysis in the matched cohort, the incidence rates (%/year) for each outcome of interest during follow-up were estimated in patients treated with TAVI or no TAVI. The corresponding asymptotic two-sided 95% confidence interval (CI) of the relative risk (RR) was reported. We performed multivariable adjustment to evaluate the association with outcomes and baseline characteristics in nonagenarians using a Cox model. A p-value <0.05 was considered statistically significant. All analyses were performed using Enterprise Guide 7.1 (SAS Institute Inc., Cary, NC, USA) and Stata version 12.0 (StataCorp, College Station, TX, USA).
Results
BASELINE CHARACTERISTICS IN THE OVERALL POPULATION
From January 2010 to December 2018, 487,045 patients with AS were identified in the nationwide database. Among them, 47,881 patients treated with TAVI have been reported (Figure 1).
Nonagenarians with AS accounted for 71,095 patients, corresponding to 65,633 who had no TAVI procedure (four SAVR) and 5,469 who underwent a TAVI (Figure 1). In this age category, patients undergoing a TAVI procedure were characterised by a lower age but more frequently reported cardiovascular risk factors and past medical history. Importantly, patients with TAVI were more often symptomatic with heart failure and previous pulmonary oedema. Among them, there were 1,312 patients in the unmatched non-TAVI cohort (2.0%) and 154 (2.9%) in the matched cohort treated with balloon aortic valvuloplasty.
Within the whole cohort of patients with a TAVI procedure, nonagenarians accounted for 5,469 patients (11.4%) (Table 1). In comparison with younger patients, cardiovascular risk factors as well as history of medical disease were less often reported in nonagenarians. However, atrial fibrillation and history of heart failure were more frequently reported in this group.
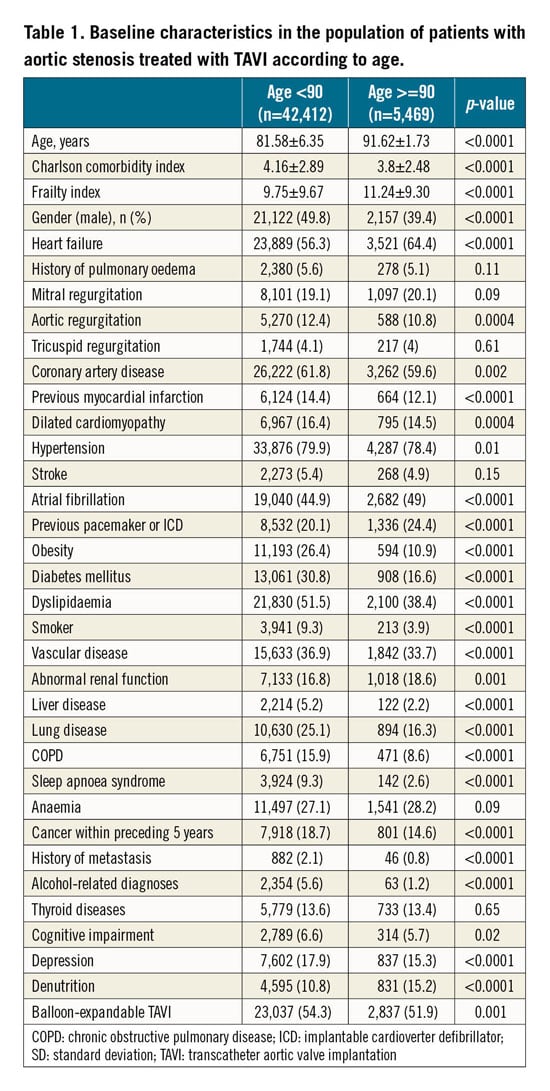
IMPACT OF TAVI IN NONAGENARIANS WITH AS
After matching on baseline characteristics, 5,338 patients were analysed in each arm (Table 2). The c-statistic of the propensity score for the likelihood of being treated with TAVI was 0.806 (95% CI: 0.800-0.813). The Hosmer-Lemeshow goodness of fit test had a p-value of 0.26, suggesting that the model was accurate. Mean follow-up was 395±508 days (median 161, interquartile range 13-625). After propensity matching, nonagenarians who underwent TAVI had a lower incidence of all-cause death, cardiovascular death and rehospitalisation for heart failure (HF) than matched nonagenarians not treated with TAVI (Table 3, Figure 2). Stroke rates were not different between the two cohorts. The combined outcome was significantly less frequent in nonagenarians undergoing a TAVI than in matched nonagenarians not treated with TAVI (Figure 3).
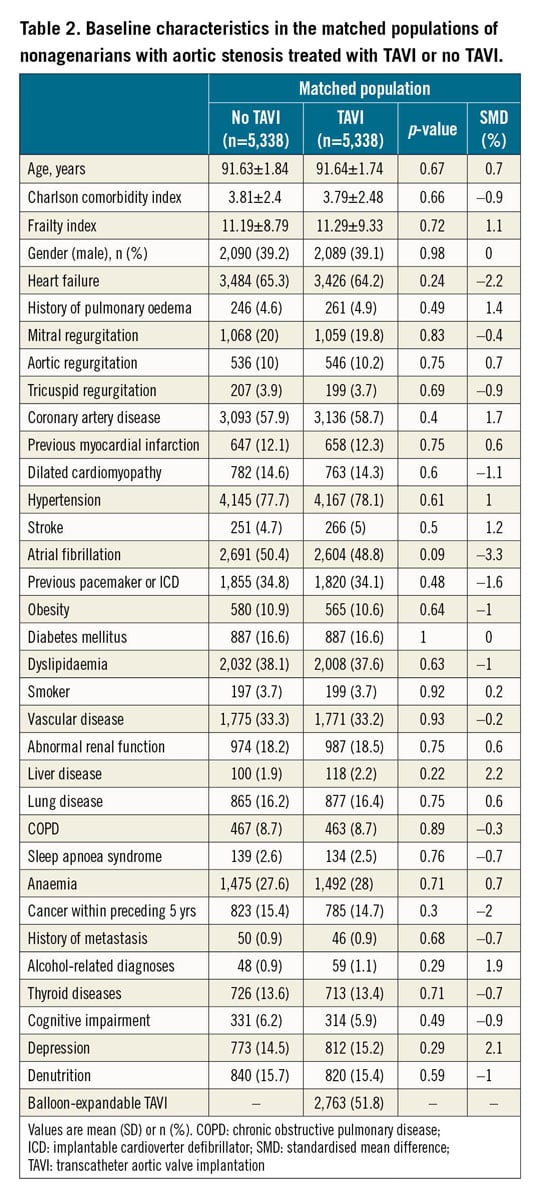
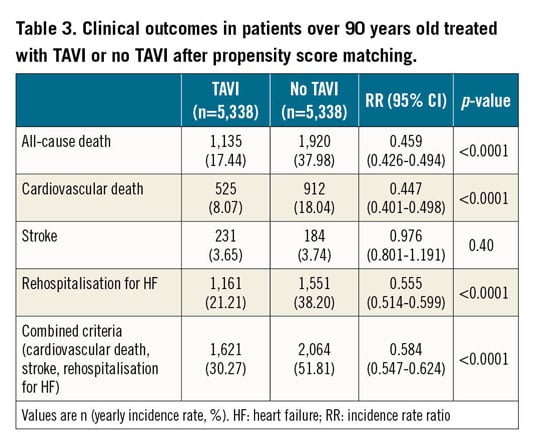
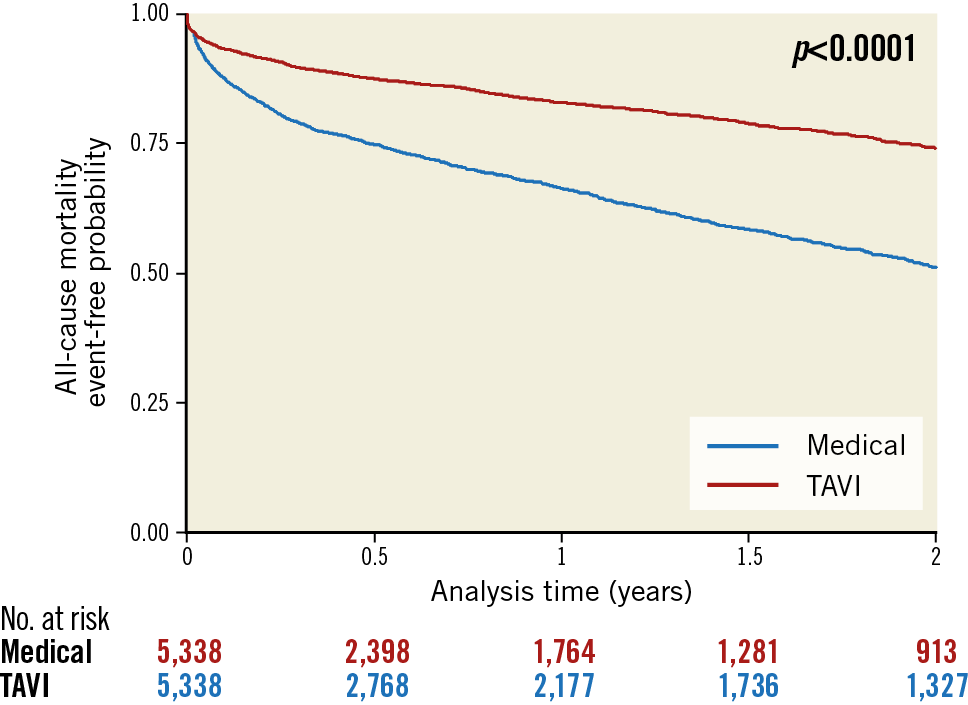
Figure 2. Event-free curves for all-cause mortality during follow-up according to TAVI or no TAVI in nonagenarians with AS.
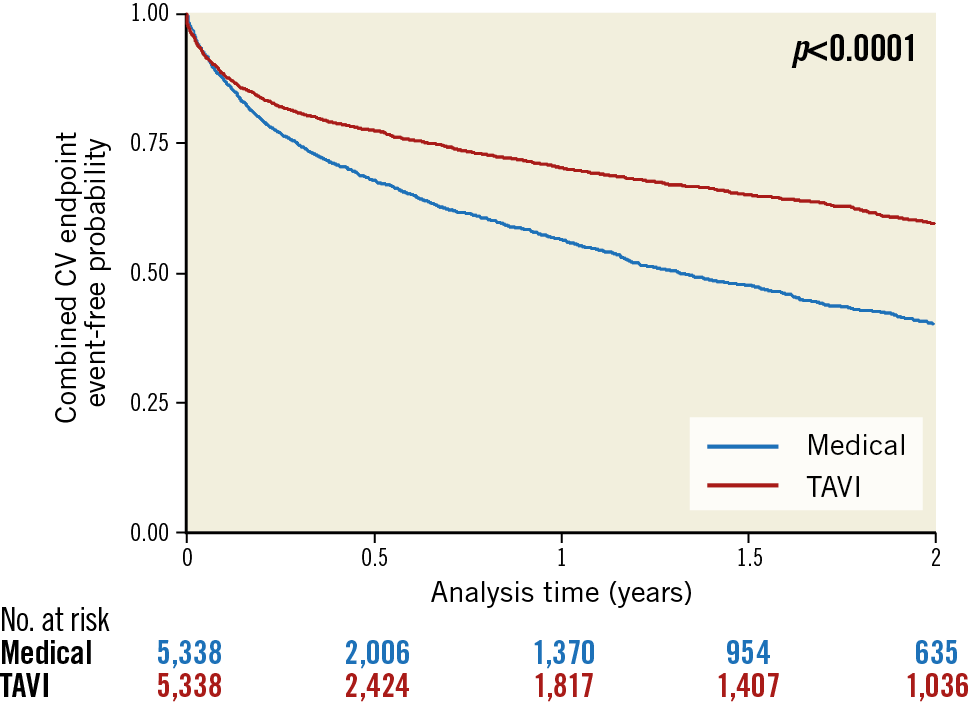
Figure 3. Event-free curves for the combined cardiovascular endpoint during follow-up according to TAVI or no TAVI in nonagenarians with AS.
We studied the association between baseline characteristics and outcomes within the nonagenarian cohorts. Older age, Charlson comorbidity index, heart failure, atrial fibrillation, previous stroke, vascular disease, cognitive impairment and denutrition were independent predictors of outcomes in nonagenarians treated with TAVI (Supplementary Table 1). A balloon-expandable TAVI device was associated with a lower incidence of the composite endpoint in this age category.
Clinical outcomes in the matched cohorts by age 90-93, 94-96 and 97-100 are shown in Supplementary Table 2 with no significant interaction in these analyses.
An additional matched analysis comparing SAVR versus TAVI in nonagenarians is provided in Supplementary Appendix 1; similar outcomes were found in the two groups of patients (Supplementary Table 3, Supplementary Table 4, Supplementary Figure 1).
OUTCOMES IN PATIENTS WITH TAVI PROCEDURE ACCORDING TO AGE
Among patients treated with TAVI, the risk of all-cause death during follow-up was higher in nonagenarians than in younger patients (RR 1.22, 95% CI: 1.15-1.30) (Table 4, Figure 4). By comparison, the risk of all-cause death in patients with AS not treated by TAVI (n=370,013) was markedly higher in nonagenarians when compared to their counterparts aged <90 (RR 2.28, 95% CI: 2.25-2.32).
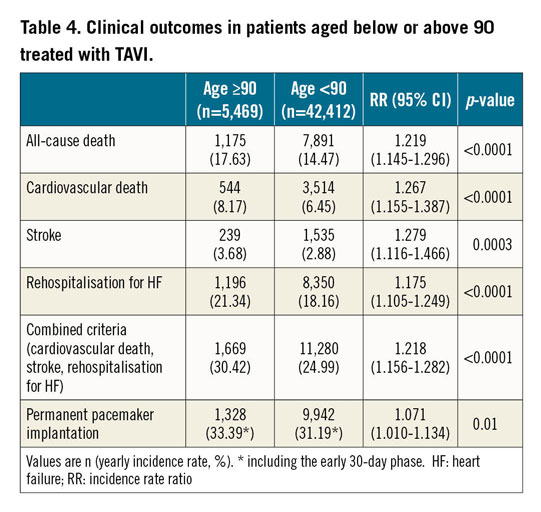
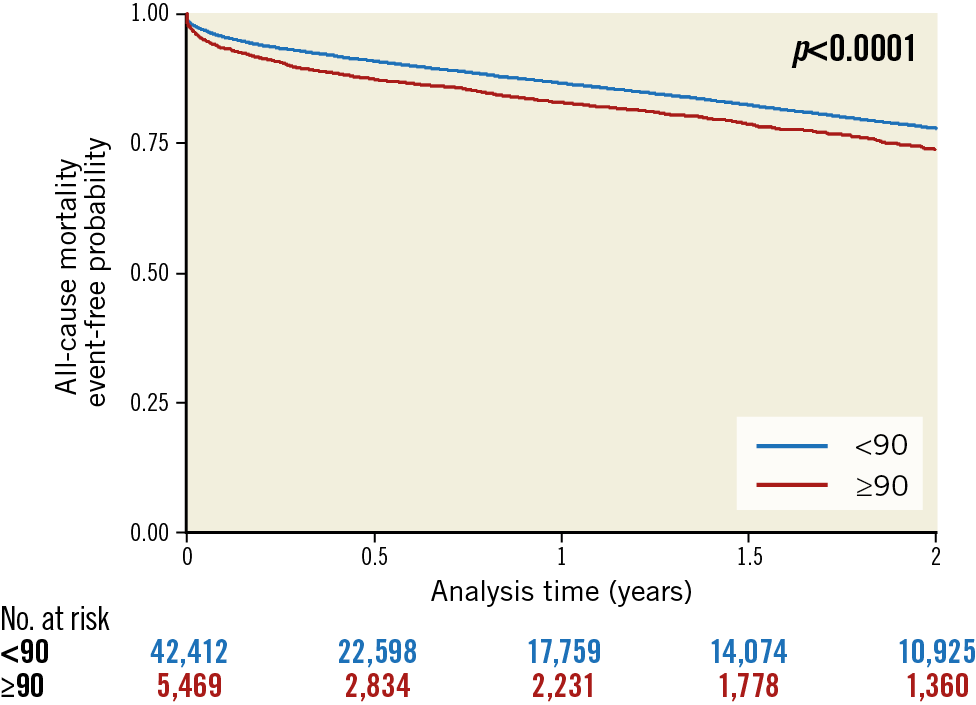
Figure 4. Event-free curves for all-cause mortality during follow-up according to age (above or below 90) in patients treated with TAVI.
Incidence rates for cardiovascular death, rehospitalisation for heart failure and ischaemic stroke were also higher in nonagenarians versus other patients. Nonagenarians had a higher risk of incidence of the combined endpoint (RR 1.22, 95% CI: 1.16–1.28, p<0.001) (Figure 5). Permanent pacemaker implantation was significantly more frequent in nonagenarians than in others.
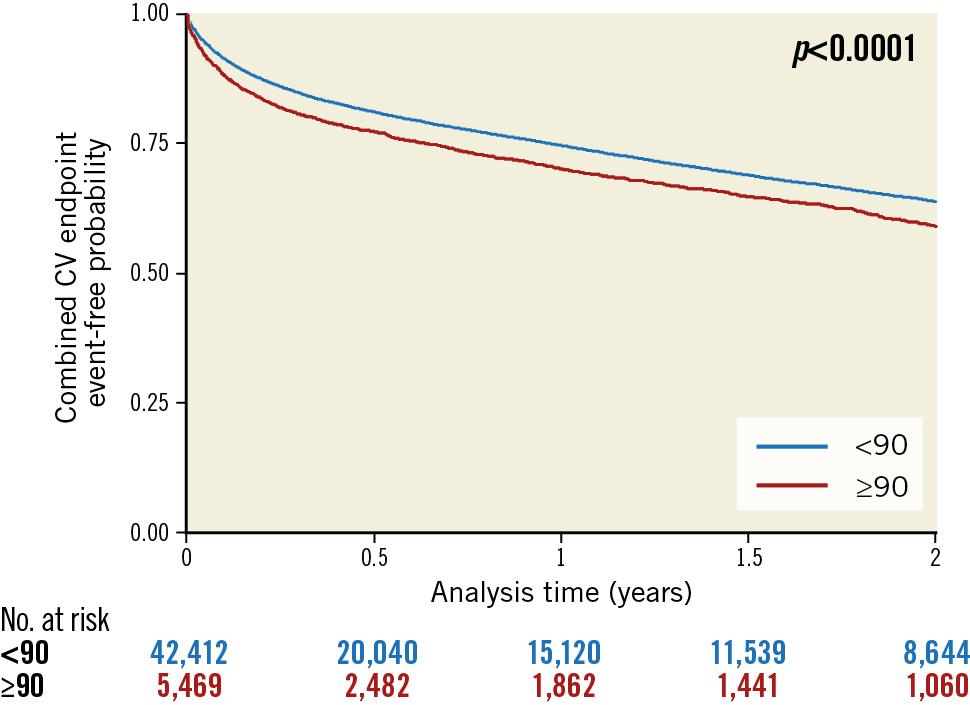
Figure 5. Event-free curves for the combined cardiovascular endpoint during follow-up according to age (above or below 90) in patients treated with TAVI.
Discussion
Our results showed that:
1. TAVI for the treatment of severe AS is associated with relatively good long-term outcomes in patients older than 90 years.
2. After a propensity matching analysis within nonagenarians suffering from AS, a TAVI procedure was associated with better prognosis in comparison with medical treatment.
3. Patients older than 90 years undergoing TAVI are highly selected with a healthier clinical profile compared with younger patients, which could explain their good outcome results.
The nonagenarian population is steadily increasing and is projected to continue growing12. AS incidence is increasing with ageing, and therefore these projections will lead to a rise in the need for AS treatment in the elderly. Decision making for nonagenarians with severe AS is not simple and represents a new challenge for physicians4,13,14,15,16.
Medical therapy and balloon aortic valvuloplasty are not effective long-term treatment strategies for severe AS17. Interestingly, it appears that, since TAVI has been available, balloon valvuloplasty only has been a relatively infrequent treatment for nonagenarians with AS. Data on cardiac surgery in nonagenarians are scarce and show relatively high mortality and morbidity at 30 days, with no long-term follow-up18. Recent data confirmed a relatively low rate of in-hospital mortality19,20. However, age is, by itself, associated with increased surgical mortality scores (EuroSCORE and STS score); therefore, nonagenarians are often considered at high risk for surgery1. Our results indicated that, among nonagenarians, older age was still a predictor of outcomes. Therefore, early intervention in suitable patients with AS seems reasonable.
TAVI emerged as a suitable alternative for efficient treatment of AS in high-risk or inoperable patients21. With the availability of TAVI, a dramatic increase in aortic valve replacement was observed in this age category (+583%)3. In 2015, SAVR performed after 85 years of age represented 20% of all AVRs, the great majority of which were TAVIs3. TAVI could be performed in those patients with acceptable short-term morbidity and mortality5,19. The CENTER collaboration showed a twofold higher 30-day mortality following TAVI in nonagenarians versus younger patients22. Our results confirm the relatively good prognosis associated with TAVI procedures in nonagenarians. A higher risk of death for nonagenarians undergoing TAVI was still observed in the long term in comparison with younger patients but was less marked than 30-day rates in the CENTER analysis. This highlights that TAVI may impact positively on the prognosis of AS patients. Therefore, screening for TAVI suitability could be offered even in the very elderly.
Identification of elderly patients who are most likely to benefit from a TAVI procedure remains challenging. Nonagenarians are often frail with significant medical and orthopaedic conditions that could mitigate the benefit of TAVI4. A proportion of patients has little or no benefit after TAVI, which has been associated with comorbidities and frailty status23. Frailty has been associated with worse survival in AS patients undergoing TAVI and strongly correlated with procedural complications in those who have SAVR23,24. In our cohort, the frailty index was slightly higher in nonagenarians but the Charlson comorbidity score was lower when compared with younger patients. This illustrates a very high selection of indications for TAVI in nonagenarians. It is likely that the TAVI procedures were often motivated by symptoms (HF in most patients), but nonagenarians undergoing TAVI were usually at low risk independently of age, and free of several comorbidities seen in younger patients. The healthier clinical profile in nonagenarians undergoing TAVI compared with younger patients has been reported previously in a smaller series of patients24. We identified specifically in nonagenarians that older age, Charlson comorbidity index, heart failure, previous myocardial infarction, atrial fibrillation, previous stroke, vascular disease, cognitive impairment and denutrition were strong predictors of adverse events following a TAVI. Therefore, specific scales could be developed to evaluate the predicted risk for TAVI procedure in nonagenarians, integrating medical history and the Charlson comorbidity index. A better identification and meticulous evaluation of patients who would gain the optimal benefit of a TAVI procedure may still be needed, both for an optimal management of each individual patient and for a global perspective in light of limited healthcare resources.
Limitations
The present study was based on administrative data, with the limitations inherent to such a methodology. However, the scale of the database minimises bias related to coding errors and, as coding of complications is linked to reimbursement and regularly controlled, it is expected to be of good quality. Our analysis was restricted to the variables present in the database. We were also not able to calculate surgical risk scores such as the EuroSCORE or the STS score. Therefore, the Charlson and frailty indices were used as surrogate predictors of mortality10. The Charlson score is based on coding at hospital discharge by physicians with varied expertise in this area. The frailty score was also evaluated to estimate a patient’s status and risk of death after intervention10. Our large population of patients admitted for a TAVI procedure probably represents a heterogeneous group of patients admitted with various kinds of illness and severity, which may have affected prognosis. The non-randomised design of the analysis leaves a risk of residual confounding factors. Definite conclusions for comparisons between groups may not be fully appropriate even though multivariable matching was performed, as it cannot fully eradicate the possible confounding variables between these groups. Finally, quality of life assessment was not possible from our database, and we cannot confirm that the high selection of nonagenarians undergoing TAVI and the good clinical outcomes have translated into improved quality of life in this cohort, although this seems likely.
Conclusion
TAVI is associated with reasonable long-term outcomes in nonagenarians and therefore they may be considered for AS treatment. Better identification of TAVI candidates within nonagenarians is critical to improve outcomes further. However, age alone should not be a discriminatory factor when screening elderly patients with AS.
|
Impact on daily practice We observed that TAVI was associated with better prognosis in nonagenarians with AS in comparison with medical therapy. We identified older age, Charlson comorbidity index, heart failure, previous myocardial infarction, atrial fibrillation, previous stroke, vascular disease, cognitive impairment and denutrition as predictors of events after a TAVI in nonagenarians. |
Conflict of interest statement
C. Sainte Etienne reports honoraria from Abbott and Biotronik. L. Fauchier is a consultant or speaker for Bayer, BMS/Pfizer, Boehringer Ingelheim, Medtronic and Novartis. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.