Abstract
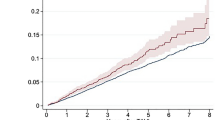
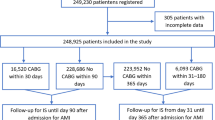
Ischemic stroke is a feared complication associated with transcatheter aortic valve replacement (TAVR). Data on the late risk of ischemic stroke following TAVR are scarce. This study aimed to investigate the early (0–90 days) and late (90 days–5 years) risk of ischemic cerebrovascular events (CVE) in a large, unselected cohort of patients undergoing TAVR and to compare this risk with a matched background population. Therefore, all patients undergoing first-time TAVR in Denmark were matched to a background population (controls) in a 1:4 ratio based on age, sex, atrial fibrillation (AF), and the major stroke risk factors. A total of 2455 TAVR patients were matched with 9820 controls. TAVR was associated with a significantly higher ischemic CVE risk as compared with their controls in the early phase [hazard ratio (HR) 5.35 [95% CI 3.50–8.17]; p < 0.001) but not in the late phase (HR 1.17 [95% CI 0.94–1.46]; p = 0.15). In a predefined stratified analysis, no patient-related factors were associated with this higher CVE risk in the early phase. The cumulative 90-day ischemic CVE risk was the lowest in TAVR-patients with known AF receiving oral anticoagulant (OAC) therapy (1.3% [95% CI 0.6–2.5%] and was two-fold higher in OAC-naïve TAVR-patients (2.4% [95% CI 1.8–3.3%] in patients without AF and 2.5% [95% CI 0.9–5.3%] in patients with AF). In conclusion, TAVR was associated with an increased risk of ischemic CVE in the early phase, but not in the late phase, as compared to their matched controls—OAC therapy reduced this early risk of ischemic CVE by half.





Similar content being viewed by others
References
Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR, PARTNER Trial Investigators et al (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364(23):2187–2198
Adams DH, Popma JJ, Reardon MJ, Yakubov SJ, Coselli JS, Deeb GM, Gleason TG, Buchbinder M, Hermiller J Jr, Kleiman NS, U.S. CoreValve Clinical Investigators et al (2014) Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 370(19):1790–1798
Leon MB, Smith CR, Mack MJ, Makkar RR, Svensson LG, Kodali SK, Thourani VH, Tuzcu EM, Miller DC, Herrmann HC, Investigators PARTNERII et al (2016) Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med 374(17):1609–1620
Reardon MJ, Van Mieghem NM, Popma JJ, Kleiman NS, Søndergaard L, Mumtaz M, Adams DH, Deeb GM, Maini B, Gada H, SURTAVI Investigators et al (2017) Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med 376(14):1321–1331
Thyregod HGH, Ihlemann N, Jørgensen TH, Nissen H, Kjeldsen BJ, Petursson P, Chang Y, Franzen OW, Engstrøm T, Clemmensen P et al (2019) Five-Year Clinical and Echocardiographic Outcomes from the Nordic Aortic Valve Intervention (NOTION) randomized clinical trial in lower surgical risk patients. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.118.036606
Gaede L, Blumenstein J, Kim WK, Liebetrau C, Dörr O, Nef H, Hamm C, Elsässer A, Möllmann H (2017) Trends in aortic valve replacement in Germany in 2015: transcatheter versus isolated surgical aortic valve repair. Clin Res Cardiol 106(6):411–419
Kim WK, Hamm CW (2018) Transcatheter aortic valve implantation in Germany. Clin Res Cardiol 107(Suppl 2):81–87
Kapadia S, Agarwal S, Miller DC, Webb JG, Mack M, Ellis S, Herrmann HC, Pichard AD, Tuzcu EM, Svensson LG et al (2016) Insights into timing, risk factors, and outcomes of stroke and transient ischemic attack after transcatheter aortic valve replacement in the PARTNER trial (Placement of Aortic Transcatheter Valves). Circ Cardiovasc Interv 9(9):e002981
Werner N, Zeymer U, Schneider S, Bauer T, Gerckens U, Linke A, Hamm C, Sievert H, Eggebrecht H, Zahn R, German Transcatheter Aortic Valve Interventions-Registry Investigators (2016) Incidence and clinical impact of stroke complicating transcatheter aortic valve implantation: results from the German TAVI Registry. Catheter Cardiovasc Interv 88(4):644–653
Kapadia SR, Huded CP, Kodali SK, Svensson LG, Tuzcu EM, Baron SJ, Cohen DJ, Miller DC, Thourani VH, Herrmann HC et al (2018) PARTNER Trial Investigators. Stroke after surgical versus transfemoral transcatheter aortic valve replacement in the PARTNER Trial. J Am Coll Cardiol 72(20):2415–2426
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scand J Public Health 39(7 Suppl):30–33
Kildemoes HW, Sorensen HT, Hallas J (2011) The Danish National Prescription Registry. Scand J Public Health 39(7 Suppl):38–41
Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39(7 Suppl):22–25
Schramm TK, Gislason GH, Kober L, Rasmussen S, Rasmussen JN, Abildstrom SZ, Hansen ML, Folke F, Buch P, Madsen M et al (2008) Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: a population study of 3.3 million people. Circulation 117(15):1945–1954
Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, Selmer C, Ahlehoff O, Olsen AM, Gislason GH et al (2011) Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ 342:d124. https://doi.org/10.1136/bmj.d124
Schaff HV (2011) Transcatheter aortic-valve implantation—at what price? N Engl J Med 364(23):2256–2258
Theut M, Thygesen JB, De Backer O, Søndergaard L (2017) Survival and cause of death after transcatheter aortic valve replacement as compared to an age- and sex-matched background population. EuroIntervention 13(9):e1058–e1066
Rodés-Cabau J, Sacco RL (2018) Neurological complications following aortic valve replacement: TAVR better than SAVR, but room for improvement. J Am Coll Cardiol 72(18):2120–2122
Auffret V, Regueiro A, Del Trigo M, Abdul-Jawad Altisent O, Campelo-Parada F, Chiche O, Puri R, Rodés-Cabau J (2016) Predictors of early cerebrovascular events in patients with aortic stenosis undergoing transcatheter aortic valve replacement. J Am Coll Cardiol. 68(7):673–684
Murdoch D, Fanning JP (2017) Early cerebrovascular events after transcatheter aortic valve replacement: patient- and procedure-specific predictors. J Thorac Dis 9(3):434–437
Makkar RR, Fontana G, Jilaihawi H, Chakravarty T, Kofoed KF, De Backer O, Asch FM, Ruiz CE, Olsen NT, Trento A et al (2015) Possible subclinical leaflet thrombosis in bioprosthetic aortic valves. N Engl J Med 373(21):2015–2024
Chakravarty T, Søndergaard L, Friedman J, De Backer O, Berman D, Kofoed KF, Jilaihawi H, Shiota T, Abramowitz Y, Jørgensen TH, RESOLVE; SAVORY Investigators et al (2017) Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves: an observational study. Lancet 389(10087):2383–2392
Sondergaard L, De Backer O, Kofoed KF, Jilaihawi H, Fuchs A, Chakravarty T, Kashif M, Kazuno Y, Kawamori H, Maeno Y et al (2017) Natural history of subclinical leaflet thrombosis affecting motion in bioprosthetic aortic valves. Eur Heart J 38(28):2201–2207
Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, ESC Scientific Document Group et al (2017) 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 38(36):2739–2791
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P et al (2014) American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63(22):2438–2488
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O'Gara PT et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 135(25):e1159–e1195
Mérie C, Køber L, Skov Olsen P, Andersson C, Gislason G, Skov Jensen J, Torp-Pedersen C (2012) Association of warfarin therapy duration after bioprosthetic aortic valve replacement with risk of mortality, thromboembolic complications, and bleeding. JAMA 308(20):2118–2125
Geis NA, Kiriakou C, Chorianopoulos E, Uhlmann L, Katus HA, Bekeredjian R (2018) NOAC monotherapy in patients with concomitant indications for oral anticoagulation undergoing transcatheter aortic valve implantation. Clin Res Cardiol 107(9):799–806
Sondergaard L, Sigitas C, Chopra M, Bieliauskas G, De Backer O (2017) Leaflet thrombosis after TAVI. Eur Heart J 38(36):2702–2703
Yanagisawa R, Tanaka M, Yashima F, Arai T, Jinzaki M, Shimizu H, Fukuda K, Watanabe Y, Naganuma T, Higashimori A et al (2019) Early and late leaflet thrombosis after transcatheter aortic valve replacement. Circ Cardiovasc Interv 12(2):e007349
Ruile P, Jander N, Blanke P, Schoechlin S, Reinöhl J, Gick M, Rothe J, Langer M, Leipsic J, Buettner HJ, Neumann FJ, Pache G (2017) Course of early subclinical leaflet thrombosis after transcatheter aortic valve implantation with or without oral anticoagulation. Clin Res Cardiol 106(2):85–95
Haussig S, Mangner N, Dwyer MG, Lehmkuhl L, Lücke C, Woitek F, Holzhey DM, Mohr FW, Gutberlet M, Zivadinov R et al (2016) Effect of a cerebral protection device on brain lesions following transcatheter aortic valve implantation in patients with severe aortic stenosis: the CLEAN-TAVI Randomized Clinical Trial. JAMA 316(6):592–601
Kapadia SR, Kodali S, Makkar R, Mehran R, Lazar RM, Zivadinov R, Dwyer MG, Jilaihawi H, Virmani R, Anwaruddin S, Linke A, SENTINEL Trial Investigators et al (2017) Protection against cerebral embolism during transcatheter aortic valve replacement. J Am Coll Cardiol 69(4):367–377
Bagur R, Solo K, Alghofaili S, Nombela-Franco L, Kwok CS, Hayman S, Siemieniuk RA, Foroutan F, Spencer FA, Vandvik PO et al (2017) Cerebral embolic protection devices during transcatheter aortic valve implantation: systematic review and meta-analysis. Stroke 48(5):1306–1315
Mohananey D, Sankaramangalam K, Kumar A, Jobanputra Y, Villablanca P, Krishnaswamy A, Mick S, Svensson LG, Tuzcu EM, Kapadia SR (2018) Safety and efficacy of cerebral protection devices in transcatheter aortic valve replacement: a clinical end-points meta-analysis. Cardiovasc Revasc Med 19(7 Pt A):785–791
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have disclosures regarding this topic
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Backer, O., Butt, J.H., Wong, YH. et al. Early and late risk of ischemic stroke after TAVR as compared to a nationwide background population. Clin Res Cardiol 109, 791–801 (2020). https://doi.org/10.1007/s00392-019-01565-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01565-0