Abstract
Background
Myocardial microvascular disease may occur during the disease course of different cardiac as well as systemic disorders. With the present study, we introduce a novel and easy-to-perform cardiovascular magnetic resonance (CMR) parameter named “myocardial transit-time” (MyoTT).
Methods
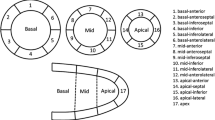
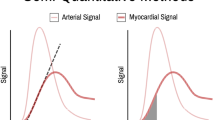
N = 20 patients with known hypertrophic cardiomyopathy (HCM) and N = 20 control patients without relevant cardiac disease underwent dedicated CMR studies on a 1.5-T MR scanner. The CMR protocol comprised cine and late-gadolinium-enhancement (LGE) imaging as well as first-pass perfusion acquisitions at rest for MyoTT measurement. MyoTT was defined as the blood circulation time from the orifice of the coronary arteries to the pooling in the coronary sinus (CS), and accordingly measured as the temporal difference between the appearances of CMR contrast agent in the aortic root and the CS reflecting the transit-time of gadolinium in the myocardial microvasculature.
Results
Patients with HCM had a significantly prolonged MyoTT compared to controls (11.0 (9.1–14.5) s vs. 6.5 (4.8–8.4) s, p < 0.001). This significant difference did not change when the individual heart rate was taken into consideration (MyoTT indexed, p < 0.001). Significant correlations were found between MyoTT and maximal left ventricular (LV) wall thickness (r = 0.771, p < 0.001), MyoTT and presence of LGE (r = 0.760, p < 0.001) as well as MyoTT and LV global longitudinal strain (r = 0.672, p < 0.001). ROC analysis resulted in an area-under-curve (AUC) of 0.90 for MyoTT and showed an optimal sensitivity/specificity cut-off of 7.85 s to differentiate HCM from controls.
Conclusion
“Myocardial transit-time” is a novel and easy-to-perform CMR parameter that allows a quick assessment of the extent of myocardial microvascular disease. This novel CMR parameter may open new vistas in the assessment of microvascular disease—not only in HCM patients. Future studies will show the usefulness and clinical relevance of this novel CMR parameter.
Graphic abstract




Similar content being viewed by others
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 1P:
-
First-pass perfusion
- BW:
-
Body weight
- CAD:
-
Coronary artery disease
- CMD:
-
Coronary microvascular dysfunction
- CMR:
-
Cardiovascular magnetic resonance
- CS:
-
Coronary sinus
- DCM:
-
Dilative cardiomyopathy
- IQR:
-
Interquartile range
- LGE:
-
Late-gadolinium-enhancement
- LV:
-
Left ventricle
- LV-EDV:
-
Left ventricular end-diastolic volume
- LV-EF:
-
Left ventricular ejection fraction
- MBF:
-
Myocardial blood flow
- MPR:
-
Myocardial perfusion reserve
- MyoTT:
-
Myocardial transit-time
- ROI:
-
Region of interest
- VENC:
-
Velocity encoding
References
Taqueti VR, Di Carli MF (2018) Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol 72(21):2625–2641
Wessel TR, Arant CB, McGorray SP, Sharaf BL, Reis SE, Kerensky RA et al (2007) Coronary microvascular reactivity is only partially predicted by atherosclerosis risk factors or coronary artery disease in women evaluated for suspected ischemia: results from the NHLBI Women’s Ischemia Syndrome Evaluation (WISE). Clin Cardiol 30(2):69–74
Crea F, Camici PG, Bairey Merz CN (2014) Coronary microvascular dysfunction: an update. Eur Heart J 35(17):1101–1111
Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT et al (2018) Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J 39(10):840–849
Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG (2003) Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 349(11):1027–1035
Gould KL, Johnson NP (2018) Coronary physiology beyond coronary flow reserve in microvascular angina: JACC state-of-the-art review. J Am Coll Cardiol 72(21):2642–2662
Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J et al (2014) Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 129(24):2518–2527
Thomson LE, Wei J, Agarwal M, Haft-Baradaran A, Shufelt C, Mehta PK et al (2015) Cardiac magnetic resonance myocardial perfusion reserve index is reduced in women with coronary microvascular dysfunction. A National Heart, Lung, and Blood Institute-sponsored study from the Women’s Ischemia Syndrome Evaluation. Circ Cardiovasc Imaging 8(4):e002481. https://doi.org/10.1161/CIRCIMAGING.114.002481
Dandekar VK, Bauml MA, Ertel AW, Dickens C, Gonzalez RC, Farzaneh-Far A (2014) Assessment of global myocardial perfusion reserve using cardiovascular magnetic resonance of coronary sinus flow at 3 Tesla. J Cardiovasc Magn Reson 16:24. https://doi.org/10.1186/1532-429X-16-24
Panting JR, Gatehouse PD, Yang G-Z, Grothues F, Firmin DN, Collins P et al (2002) Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med 346(25):1948–1953
Vermeltfoort IAC, Bondarenko O, Raijmakers PGHM, Odekerken DAM, Kuijper AFM, Zwijnenburg A et al (2007) Is subendocardial ischaemia present in patients with chest pain and normal coronary angiograms? A cardiovascular MR study. Eur Heart J 28(13):1554–1558
Task Force Members, Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C et al (2013) ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34(38):2949–3003
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA (2011) Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 57(8):891–903
Schuster A, Stahnke VC, Unterberg-Buchwald C, Kowallick JT, Lamata P, Steinmetz M et al (2015) Cardiovascular magnetic resonance feature-tracking assessment of myocardial mechanics: intervendor agreement and considerations regarding reproducibility. Clin Radiol 70(9):989–998
Reis SE, Holubkov R, Conrad Smith AJ, Kelsey SF, Sharaf BL, Reichek N et al (2001) Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J 141(5):735–741
Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U (2012) High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol 59(7):655–662
Hamasaki S, Al Suwaidi J, Higano ST, Miyauchi K, Holmes DR Jr, Lerman A (2000) Attenuated coronary flow reserve and vascular remodeling in patients with hypertension and left ventricular hypertrophy. J Am Coll Cardiol 35(6):1654–1660
Laine H, Raitakari OT, Niinikoski H, Pitkanen OP, Iida H, Viikari J et al (1998) Early impairment of coronary flow reserve in young men with borderline hypertension. J Am Coll Cardiol 32(1):147–153
Brush JE Jr, Cannon RO 3rd, Schenke WH, Bonow RO, Leon MB, Maron BJ et al (1988) Angina due to coronary microvascular disease in hypertensive patients without left ventricular hypertrophy. N Engl J Med 319(20):1302–1307
Rajappan K, Rimoldi OE, Camici PG, Bellenger NG, Pennell DJ, Sheridan DJ (2003) Functional changes in coronary microcirculation after valve replacement in patients with aortic stenosis. Circulation 107(25):3170–3175
Taqueti VR, Shaw LJ, Cook NR, Murthy VL, Shah NR, Foster CR et al (2017) Excess cardiovascular risk in women relative to men referred for coronary angiography is associated with severely impaired coronary flow reserve, not obstructive disease. Circulation 135(6):566–577
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J et al (2015) Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 131(1):19–27
Gupta A, Taqueti VR, van de Hoef TP, Bajaj NS, Bravo PE, Murthy VL et al (2017) Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation 136(24):2325–2336
Taqueti VR, Everett BM, Murthy VL, Gaber M, Foster CR, Hainer J et al (2015) Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation 131(6):528–535
Maron BJ, Wolfson JK, Epstein SE, Roberts WC (1986) Intramural (“small vessel”) coronary artery disease in hypertrophic cardiomyopathy. J Am Coll Cardiol 8(3):545–557
Gould KL, Lipscomb K (1974) Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol 34(1):48–55
Salerno M, Beller GA (2009) Noninvasive assessment of myocardial perfusion. Circ Cardiovasc Imaging 2(5):412–424
Knaapen P, Lubberink M (2008) Cardiac positron emission tomography: myocardial perfusion and metabolism in clinical practice. Clin Res Cardiol 97(11):791–796. https://doi.org/10.1007/s00392-008-0662-9
Maddahi J, Packard RR (2014) Cardiac PET perfusion tracers: current status and future directions. Semin Nucl Med 44(5):333–343
Crea F, Lanza GA, Camici PG (2014) Coronary microvascular dysfunction. Springer, Milan
Koskenvuo JW, Sakuma H, Niemi P, Toikka JO, Knuuti J, Laine H et al (2001) Global myocardial blood flow and global flow reserve measurements by MRI and PET are comparable. J Magn Reson Imaging 13(3):361–366
Bietenbeck M, Florian A, Shomanova Z, Meier C, Yilmaz A (2018) Reduced global myocardial perfusion reserve in DCM and HCM patients assessed by CMR-based velocity-encoded coronary sinus flow measurements and first-pass perfusion imaging. Clin Res Cardiol 107(11):1062–1070. https://doi.org/10.1007/s00392-018-1279-2
Lanza GA, Crea F (2010) Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation 121(21):2317–2325
Authors/Task Force m, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F et al (2014) 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 35(39):2733–2779
Collier P, Phelan D, Klein A (2017) A test in context: myocardial strain measured by speckle-tracking echocardiography. J Am Coll Cardiol 69(8):1043–1056
Tower-Rader A, Mohananey D, To A, Lever HM, Popovic ZB, Desai MY (2018) Prognostic value of global longitudinal strain in hypertrophic cardiomyopathy: a systematic review of existing literature. JACC Cardiovasc Imaging pii: S1936-878X(18)30671-5. https://doi.org/10.1016/j.jcmg.2018.07.016
Orwat S, Kempny A, Diller GP, Bauerschmitz P, Bunck A, Maintz D et al (2014) Cardiac magnetic resonance feature tracking: a novel method to assess myocardial strain. Comparison with echocardiographic speckle tracking in healthy volunteers and in patients with left ventricular hypertrophy. Kardiol Pol 72(4):363–371
Stewart GN (1893) Researches on the circulation time in organs and on the influences which affect it: parts I–III. J Physiol 15(1–2):1–89
Bernstein H, Skelton RBT, Gold H, Irving DW, Corday E (1962) Myocardial transit time: a new technic for evaluating coronary circulation I. Effect of systemic blood pressure. Am J Cardiol 9(5):777–782
Haridasan V, Nandan D, Raju D, Rajesh GN, Sajeev CG, Vinayakumar D et al (2013) Coronary sinus filling time: a novel method to assess microcirculatory function in patients with angina and normal coronaries. Indian Heart J 65(2):142–146
Kadermuneer P, Vinod GV, Haridasan V, Rajesh G, Sajeev CG, Bastion C et al (2015) Prognostic significance of coronary sinus filling time in patients with angina and normal coronaries at one year follow up. Indian Heart J 67(3):245–249
Author information
Authors and Affiliations
Contributions
GC participated in the CMR exams, carried out the data and statistical analysis, and wrote the initial draft version of the manuscript. MB participated in the CMR exams, carried out the data and statistical analysis, and wrote some paragraphs of the initial draft version of the manuscript. AF, CM, and DC participated in the CMR exams and in the analysis of the CMR data. HR critically reviewed the manuscript. AY supervised the study, critically reviewed the manuscript and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics approval and consent to participate
The study protocol complies with the Declaration of Helsinki. Written informed consent was obtained from every patient.
Rights and permissions
About this article
Cite this article
Chatzantonis, G., Bietenbeck, M., Florian, A. et al. “Myocardial transit-time” (MyoTT): a novel and easy-to-perform CMR parameter to assess microvascular disease. Clin Res Cardiol 109, 488–497 (2020). https://doi.org/10.1007/s00392-019-01530-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-019-01530-x