Abstract
Aims: The impact of an occluded right coronary artery (RCA) in patients with left main coronary artery disease (LMCAD) undergoing revascularisation is unknown. We compared outcomes for patients with LMCAD randomised to percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) according to the presence of an occluded RCA in the EXCEL trial.
Methods and results: The EXCEL trial randomised 1,905 patients with LMCAD and SYNTAX scores ≤32 to PCI with everolimus-eluting stents versus CABG. Patients were categorised according to whether they had an occluded RCA at baseline, and their outcomes were examined using multivariable Cox proportional hazards regression. The primary endpoint was a composite of death, stroke, or myocardial infarction at three years. Among 1,753 patients with a dominant RCA by core laboratory analysis, the RCA was occluded in 130 (7.4%) at baseline. PCI was attempted in 34 of 65 patients with an occluded RCA (52.3%) and was successful in 27 (79.4% of those attempted; 41.5% of all RCAs recanalised). The RCA was bypassed in 42 of 65 patients with an occluded RCA (64.6%; p=0.0008 versus PCI). The three-year absolute and relative rates of the primary endpoint were similar between PCI and CABG, in patients with or without an occluded RCA (pinteraction=0.92).
Conclusions: In the EXCEL trial, the presence of an occluded RCA at baseline did not confer a worse three-year prognosis in patients undergoing revascularisation for LMCAD and did not affect the relative outcomes of PCI versus CABG in this high-risk patient cohort.
Introduction
Patients with left main (LM) coronary artery disease (CAD) in whom the right coronary artery (RCA) is occluded are at potentially high risk for percutaneous coronary intervention (PCI). Since the RCA is totally occluded, if a significant complication occurs in the left coronary system during the procedure, complete deprivation of blood supply to the entire myocardium may occur. For this reason, coronary artery bypass grafting (CABG) may compare favourably to PCI for LM revascularisation in these high-risk patients. Furthermore, CABG more frequently achieves complete revascularisation than PCI in patients with complex lesions and extensive CAD1, and complete revascularisation has been associated with decreased rates of adverse events, including a lower risk of mortality2,3,4,5,6. The presence of an occluded RCA at baseline, the most challenging lesion subtype to treat successfully with PCI, might therefore differentially impact on the relative rate of short- and long-term clinical outcomes in CABG versus PCI in patients with LMCAD. Conversely, patients with chronic total occlusions often have increased surgical risk due to a higher prevalence of risk factors including older age, chronic kidney disease, and extra-cardiac vascular disease, and may less likely achieve complete revascularisation1,7,8. We sought to assess the relative efficacy of PCI versus CABG on the 30-day and three-year risk of adverse ischaemic events after LM revascularisation for patients with and without an occluded RCA at baseline in the Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL) trial.
Methods
TRIAL DESIGN AND STUDY POPULATION
The study design, protocol, and primary results of the EXCEL trial have been described previously in detail9,10. In brief, EXCEL was a prospective, international, open-label, multicentre trial that randomised 1,905 patients with LMCAD to PCI (n=948) with fluoropolymer-based cobalt-chromium everolimus-eluting stents (XIENCE; Abbott Vascular, Santa Clara, CA, USA) or CABG (n=957). Key inclusion criteria were visually estimated ≥70% diameter stenosis of the LM or 50% to <70% LM stenosis if determined to be haemodynamically significant by means of non-invasive or invasive testing, low or intermediate anatomical CAD complexity (defined by a site-assessed SYNTAX score ≤32), and a consensus among the members of the Heart Team regarding eligibility for revascularisation with either PCI or CABG1. For the present analysis, patients were categorised according to whether they had an occluded dominant RCA at baseline or not. Patients were excluded either because they were missing information regarding the coronary dominance (right or left) or the patency/occlusion of the RCA (i.e., angiogram not available for core laboratory review) or because they had a left dominant coronary circulation.
DEFINITIONS AND ENDPOINTS
The primary endpoint of the EXCEL trial was the rate of a composite of death from any cause, stroke, or myocardial infarction (MI) at three years. The definitions of the component endpoints have been reported previously9. An independent events committee reviewed and adjudicated all primary and major secondary adverse events as well as stent thromboses and symptomatic graft occlusions.
The Duke Jeopardy score, which encompasses both the severity of and volume of myocardium subtended by a coronary stenosis, was calculated by dividing the coronary tree into six segments: the left anterior descending (LAD) artery, diagonal branches of the LAD, septal perforating branches, the circumflex artery, obtuse marginal branches, and the posterior descending artery. All segments distal to stenosis of ≥70% were considered at risk. Each such segment was assigned two points. The points were added up for the final score (maximum 12 points)11,12.
STATISTICAL ANALYSIS
Comparison of baseline and procedure characteristics, medical history, and clinical events was conducted using the χ2 test or Fisher’s exact test for binary variables, t-test or Wilcoxon rank-sum test for continuous variables, and log-rank test for time-to-event variables. Adjusted comparisons of the outcomes of PCI versus CABG were conducted in patients with and without an occluded RCA using multivariable Cox proportional hazards regression. Covariates included in the adjusted model based on historical prognostic relevance were age, sex, diabetes mellitus, body mass index, hypertension, chronic obstructive pulmonary disease, smoking status, chronic kidney disease (creatinine clearance ≤60 mL/min), peripheral vascular disease, prior cerebrovascular accident or transient ischaemic attack, recent MI (within one week from the randomisation), distal LM disease (bifurcation or trifurcation), left ventricular ejection fraction (LVEF), baseline SYNTAX score (core laboratory assessed), and randomisation (PCI versus CABG). All analyses were performed in the intention-to-treat population. All p-values are two-tailed, and p<0.05 was considered statistically significant for all analysis.
Results
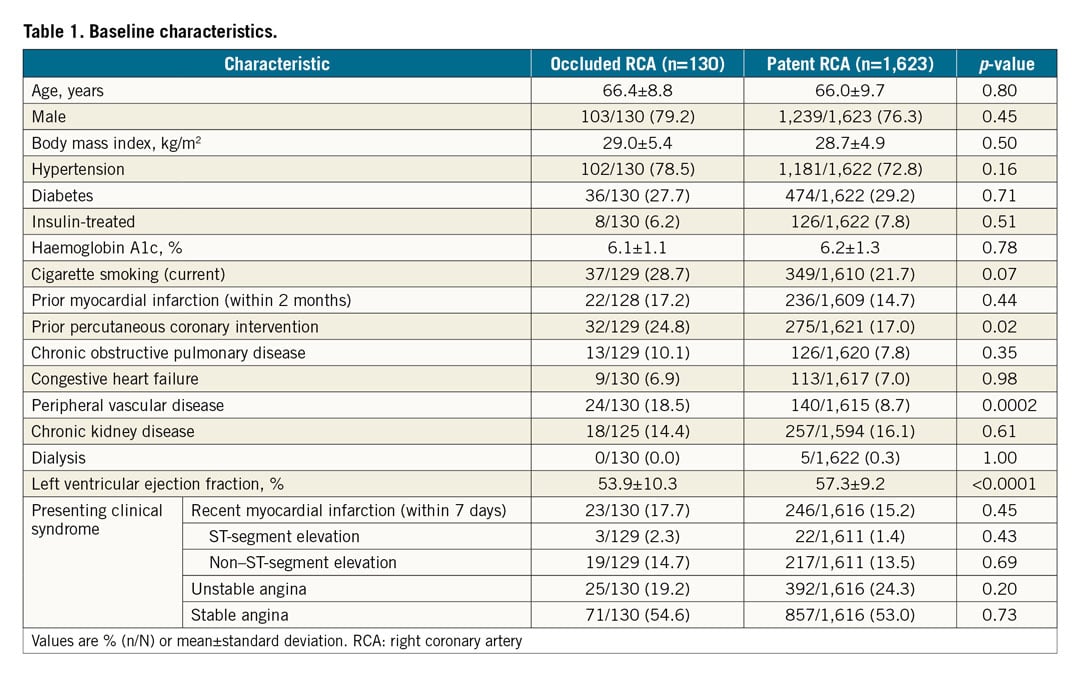
Among the 1,905 patients with LMCAD who were enrolled in the EXCEL trial, 1,753 patients with a dominant RCA had known RCA status (occluded or patent) at baseline and comprised the present analysis population. Among these 1,753 patients, an occluded RCA at baseline was present in 130 patients (7.4%). Baseline characteristics of patients with and without an occluded RCA are presented in Table 1. Patients with an occluded RCA more frequently had peripheral vascular disease, prior PCI, and lower LVEF at baseline. The severity and extent of CAD as reflected by the mean SYNTAX score were significantly higher in patients with an occluded RCA (Supplementary Table 1). Planned staged procedures were more common in patients with an occluded RCA assigned to PCI. The number of treated non-LM vessels and lesions, as well as the number of stents implanted in non-LM vessels, was higher among patients with versus without an occluded RCA. Radiation dose was also higher among patients with an occluded RCA, while the amount of total contrast injected was comparable between patients with and without an occluded RCA. There were no significant differences in baseline characteristics between patients treated with PCI or with CABG in those with or without an occluded RCA.
Among 65 patients with an occluded RCA assigned to PCI, PCI was attempted in 34 patients (52.3%) and was successful in 27 (79.4% of those attempted; 41.5% of all RCAs recanalised). The rates of procedural complications did not differ significantly between patients with occluded versus patent RCA who were treated with PCI except for a higher rate of coronary perforation during the procedure that was not seen at the end of the procedure (Supplementary Table 2). Among 65 patients with an occluded RCA assigned to CABG, the RCA was bypassed in 42 (64.6%). Thus, assuming all bypass grafts were patent post procedure, more occluded RCAs were successfully recanalised by CABG than PCI (64.6% vs 41.5%, p=0.0008).
RESIDUAL SYNTAX AND DUKE JEOPARDY SCORES IN PATIENTS UNDERGOING PCI
As shown in Table 2 and Figure 1, the residual SYNTAX score and delta SYNTAX score (the difference between the baseline and residual [post-PCI] SYNTAX scores) were both higher in patients with versus without an occluded RCA. Complete revascularisation (residual SYNTAX score=0) was less commonly achieved in patients with versus without an occluded RCA (15.6% versus 28.4%, p=0.03). Similarly, the baseline and residual Duke Jeopardy scores were significantly higher in patients with an occluded RCA. A residual Duke Jeopardy score ≥4 was present in 25.4% of patients with an occluded RCA versus 10.3% of patients with a patent RCA (p=0.0003).
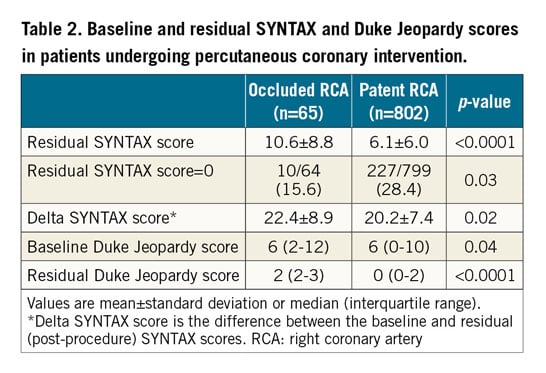
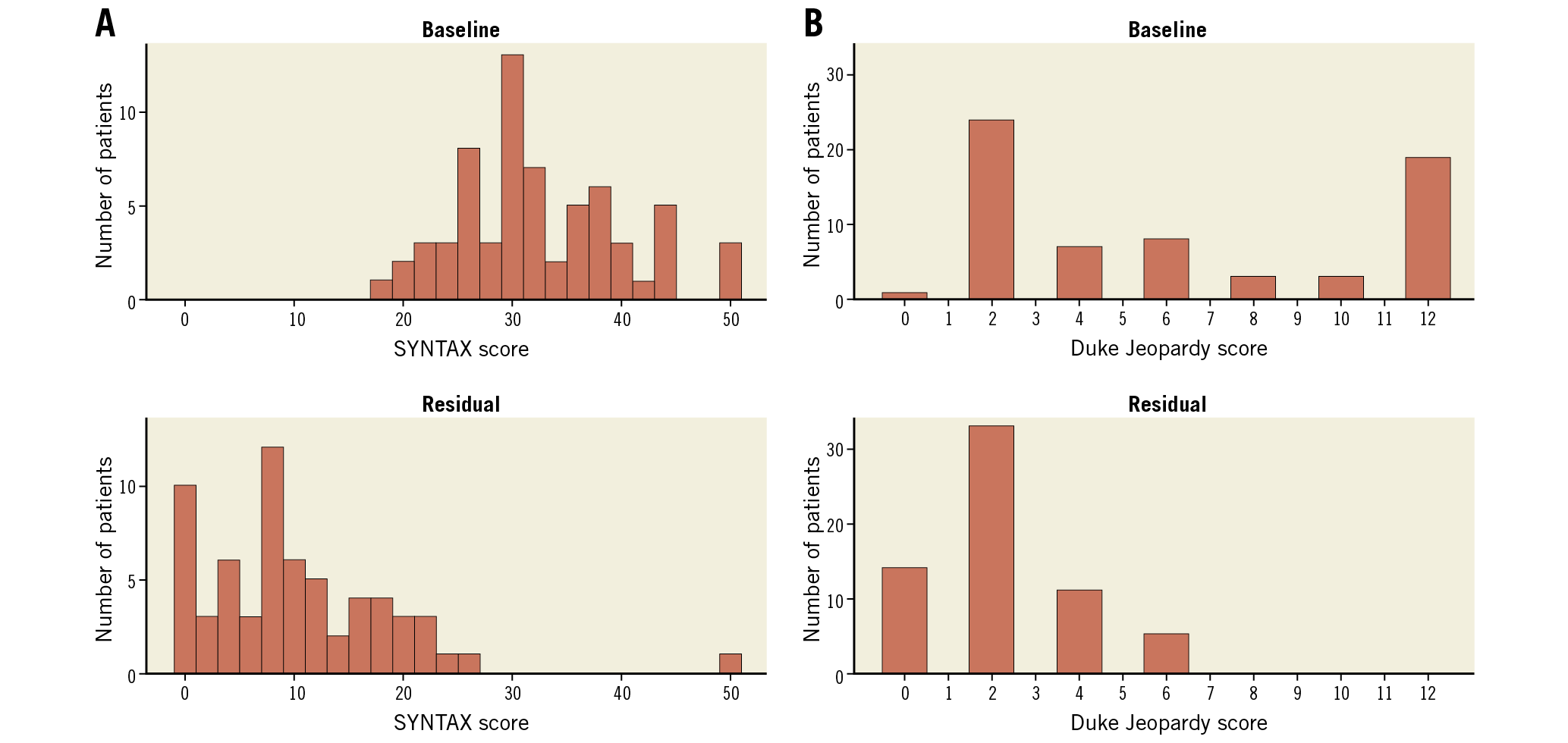
Figure 1. Distribution of SYNTAX score and Duke Jeopardy score in patients with right coronary artery total occlusion who underwent percutaneous coronary intervention. SYNTAX score (A), and Duke Jeopardy score (B) at baseline (top panel) and post procedure (residual) (bottom panel).
CLINICAL OUTCOMES
Thirty-day outcomes did not differ significantly between patients with versus without an occluded RCA at baseline. The three-year rate of the primary composite endpoint of death, stroke, or MI was also similar in those with and without an occluded RCA at baseline (16.4% vs 14.2%; hazard ratio [HR] 1.14, 95% confidence interval [CI]: 0.73-1.78, p=0.58) (Supplementary Table 3). Similarly, the three-year rates of the components of the primary endpoint and ischaemia-driven revascularisation (IDR) were similar in patients with and without an occluded RCA at baseline. The only outcome that differed between the groups was symptomatic graft stenosis or occlusion, which was more common among patients with an occluded RCA at baseline. These results were similar after multivariable adjustment for differences in baseline covariates (Supplementary Table 4).
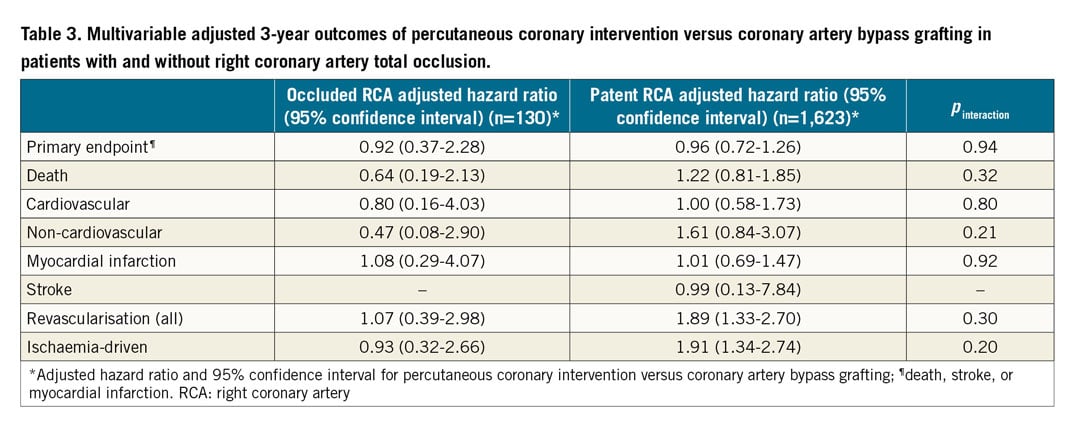
The relative outcomes at 30 days did not differ significantly after PCI versus CABG according to the presence of an occluded RCA except for the rate of clinically significant bleeding (Bleeding Academic Research Consortium [BARC] 3-5 bleeding), which was significantly higher with CABG than with PCI among patients without an occluded RCA but not among patients with an occluded RCA (pinteraction=0.04) (Supplementary Table 5). At three years, no significant differences in the absolute or relative rates of the primary endpoint were observed between the PCI and CABG groups in patients with an occluded RCA (17.2% vs 15.5%; HR 1.07, 95% CI: 0.45-2.51, p=0.88) or without an occluded RCA (14.5% vs 13.9%; HR 1.02, 95% CI: 0.79-1.33, p=0.86) (pinteraction=0.92) (Supplementary Table 6, Figure 2A). Similarly, the relative risks of PCI versus CABG for the individual components of the primary endpoint were consistent in patients with and without an occluded RCA (Figure 2B, Figure 2C). Among patients without an occluded RCA, the three-year rate of IDR was significantly higher after PCI compared with CABG (12.7% vs 6.9%; HR 1.87, 95% CI: 1.34-2.61, p=0.0002), whereas the three-year risk of IDR was similar with PCI and CABG for patients with an occluded RCA (11.1% vs 11.1%; HR 0.93, 95% CI: 0.33-2.66, p=0.90); however, the p-value for interaction was not significant (pinteraction=0.22) (Figure 2D). Among patients with an occluded RCA at baseline, the rates of any RCA revascularisation or RCA graft occlusion at three years were similar with PCI and CABG (4.5% vs 2.4%; HR 1.64, 95% CI: 0.10-26.29, p=0.73). After multivariable adjustment, the risk of IDR remained significantly higher after PCI versus CABG for patients without an occluded RCA but not for those with an occluded RCA (Table 3). Among all 130 patients with an occluded RCA, the three-year rate of the primary endpoint was 17.5% among the 69 patients in whom either RCA PCI was successful or RCA CABG was performed versus 15.0% among the 61 patients in whom RCA PCI was unsuccessful or PCI or CABG was not attempted (p=0.58).
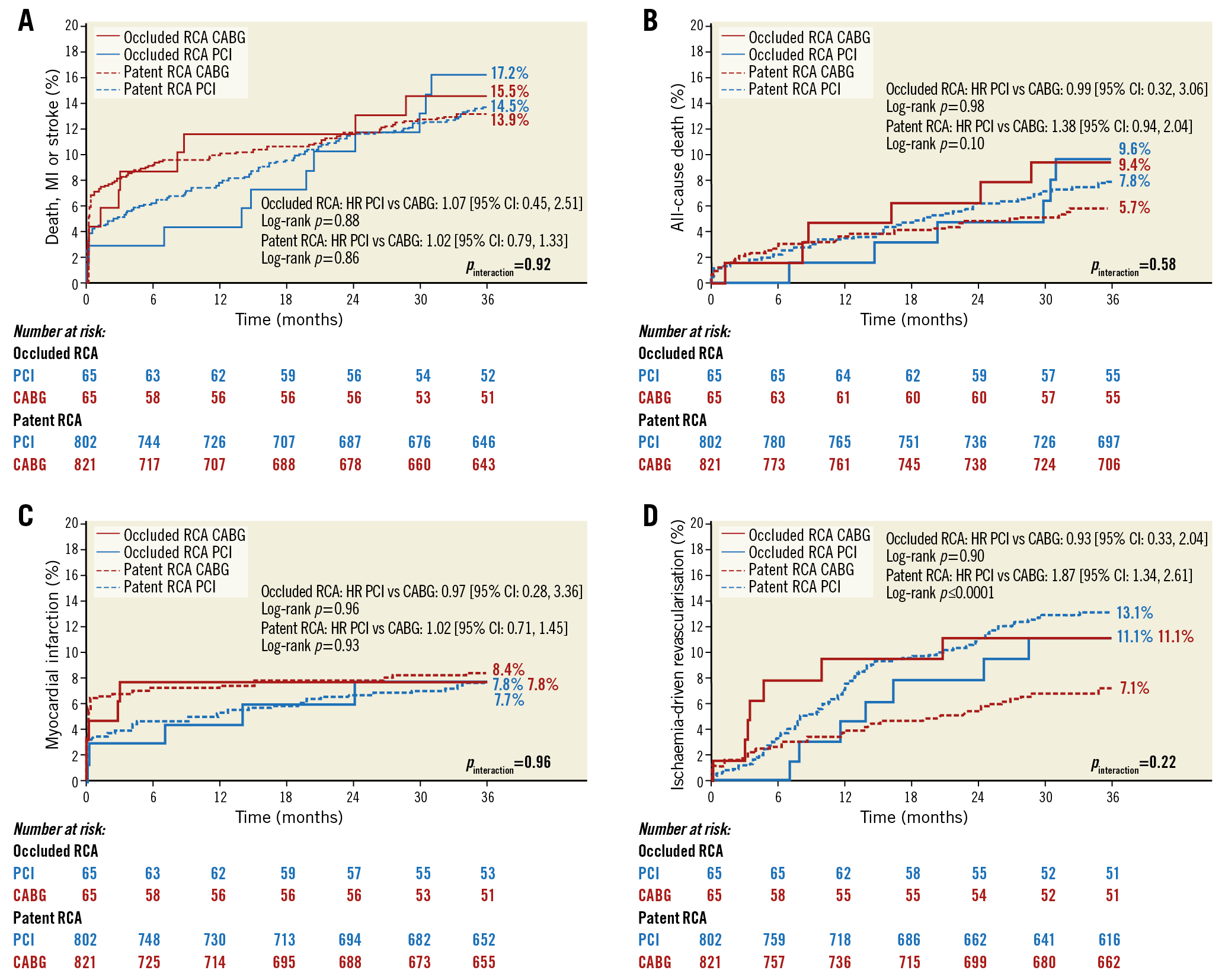
Figure 2. Kaplan-Meier failure rates in patients with versus without right coronary artery total occlusion at baseline according to revascularisation modality. A) Primary endpoint (death, stroke, or myocardial infarction). B) All-cause death. C) Myocardial infarction. D) Ischaemia-driven revascularisation. Pinteraction indicates the p-value for the interaction test comparing the effect of treatment (PCI versus CABG) in patients with and without RCA total occlusion. CABG: coronary artery bypass grafting; CI: confidence interval; HR: hazard ratio; PCI: percutaneous coronary intervention; RCA: right coronary artery
Discussion
To the best of our knowledge, the present analysis from the EXCEL trial is the first to examine the outcomes of LM revascularisation with PCI versus CABG according to the presence of an occluded RCA at baseline. The major findings are that (i) the presence of an occluded RCA was not independently associated with a higher 30-day or three-year risk of the primary composite endpoint of death, stroke, or MI, or any its components, and (ii) the short- and long-term outcomes after PCI versus CABG were consistent for patients with and without an occluded RCA at baseline. The moderate success rate of revascularisation by PCI (79.4%) implies that most of the RCA occlusions were chronic. It is noteworthy that, although total occlusions of the RCA were successfully revascularised more frequently with CABG than PCI, the total proportion of occluded RCA vessels revascularised after both procedures was relatively low and similar to that observed from the SYNTAX trial era13.
Theoretically, the presence of an occluded RCA could influence short- and long-term outcomes after PCI versus CABG in several ways. Short-term results might be affected by increased procedural risks associated with an occluded RCA, either directly or due to associated comorbidities. The presence of an occluded RCA may further impact on long-term results differently after PCI versus CABG. First, the PCI retrograde approach to the occluded RCA14 is inherently more complex and potentially risky in patients with LMCAD, even if attempted after LM stenting. Nevertheless, the 79.4% success rate of PCI of the occluded RCA was reasonable, considering that the residual Duke Jeopardy score was ≤2 in approximately 75% of patients. Second, right ventricular dysfunction is more common in patients with versus without an occluded RCA, especially when the occlusion is located proximally in the RCA with poorly developed coronary collaterals15. In this regard, right ventricular function might further deteriorate during CABG due to ischaemic stress16,17,18, increasing the procedural risk. However, in the current study no clear advantage was found for either PCI or CABG in the treatment of LMCAD in patients with an occluded RCA at baseline.
Interestingly, the lower rate of repeat revascularisation observed with CABG compared with PCI in the main EXCEL trial analysis9 was not seen in patients with an occluded RCA, who had similar rates of IDR with PCI and CABG. The adjusted HR (PCI versus CABG) for IDR was 0.93 (95% CI: 0.32-2.66) in patients with an occluded RCA compared with 1.91 (95% CI: 1.34-2.74) in patients without an occluded RCA, although this interaction did not reach statistical significance. Occluded vessels are often diffusely atherosclerotic and heavily calcified, potentially reducing long-term graft patency19. The presence of coronary occlusion (especially long lesions >40 mm) has been shown to be an independent predictor of post-CABG graft failure20,21. RCA occlusions in particular have been reported to have a higher risk of graft failure than patients with LAD or circumflex artery occlusions20,22. The particularly high risk of graft failure after CABG of RCA occlusions may be related to the relatively high use of vein grafts for their treatment20. After revascularisation of a chronic occlusion, graft patency may be further compromised by competitive flow through collaterals23,24,25, which may remain patent even after successful bypass26. The collateral network distal to the occluded RCA may be particularly robust after LM revascularisation and create competitive flow with the graft23,24. Thus, the advantage of CABG in reducing IDR may be less evident in patients with an occluded RCA. However, as the number of patients with an occluded RCA who were treated with CABG was modest and routine angiographic follow-up was not performed, these observations should be considered exploratory.
The differences observed in clinically significant bleeding between PCI and CABG in patients with but not without an occluded RCA (pinteraction=0.04 for BARC 3-5) might be a chance finding as a result of multiplicity. This contention is supported by the lack of interaction between the treatment arm and the presence of an occluded RCA regarding bleeding according to Thrombolysis In Myocardial Infarction (TIMI) criteria.
Limitations
The present study is a post hoc analysis and thus hypothesis-generating. The EXCEL trial was not powered to detect differences between patients with versus without an occluded RCA regarding the efficacy of PCI versus CABG. The overall number of patients with an occluded RCA was relatively small and results should thus be interpreted with caution. Even though EXCEL collected information on most cardiovascular risk factors and covariate differences were accounted for in multivariable models, we cannot rule out the presence of unmeasured confounders. Our findings are applicable to the specific patient population enrolled in EXCEL; their generalisability to a broader group of patients with versus without RCA chronic total occlusion (CTO) undergoing LM revascularisation requires external validation. The occluded RCA PCI success rate in the present study of 79.4% of those attempted (41.5% of all RCA vessels) represents the outcomes from a large group of skilled operators participating in EXCEL. Real-world success rates may be higher or lower depending on the expertise of the individual operator. Similarly, only 64.6% of occluded RCAs were grafted during CABG, possibly reflecting poor distal targets or lack of viable myocardium. Moreover, not all grafts are patent early and in the intermediate term after CABG, and restenosis after RCA PCI may certainly occur. Thus, because of absent routine follow-up angiography, the long-term absolute and relative RCA patency rates after both revascularisation modalities are unknown. No significant difference in the present study was noted in the three-year rate of the primary outcome measure in patients in whom an occluded RCA was versus was not successfully revascularised; however, the present analysis was underpowered in this regard to draw definitive conclusions. Finally, routine angiographic follow-up was not performed, and thus the rates of restenosis and graft occlusion were not ascertained.
Conclusions
In the EXCEL trial, the outcomes of PCI versus CABG for LMCAD were consistent for the primary endpoint of three-year death, stroke, or MI in patients with and without an occluded RCA at baseline. The increased need for repeat intervention during three-year follow-up after PCI with everolimus-eluting stents compared with CABG was confined to patients without an occluded RCA at baseline.
|
Impact on daily practice The presence of right coronary artery (RCA) total occlusion was not associated with an increased 30-day or three-year risk of adverse clinical outcomes after left main coronary artery (LM) revascularisation. The relative risk associated with percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG) regarding the composite of death, myocardial infarction, or stroke was similar for patients with and without an occluded RCA. The risk of ischaemia-driven revascularisation was lower after CABG compared with PCI in patients without but not in those with an occluded RCA, although there was no statistical interaction between an occluded RCA and treatment modality. In conclusion, the presence of an occluded RCA at baseline did not appear to affect outcomes adversely after LM revascularisation by PCI or CABG. |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Funding
The EXCEL trial was sponsored and funded by Abbott Vascular (Santa Clara, CA, USA).
Conflict of interest statement
D. Karmpaliotis has received honoraria from Abbott Vascular, Boston Scientific, and Abiomed, and holds equity in Saranas and Soundbyte. J.D. Puskas reports other from Medtronic, outside the submitted work. D.E. Kandzari has received grants and personal fees from Medtronic, Boston Scientific and Biotronik, and personal fees from Cardinal Health, outside the submitted work. A.P. Banning is partially funded by the NHS NIHR Biomedical Research Centre, Oxford. M.C. Morice is CEO of CERC. P.W. Serruys has received personal fees from Abbott Laboratories, AstraZeneca, Biotronik, Cardialysis, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital & Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St. Jude Medical, Qualimed, and Xeltis, outside the submitted work. A.P. Kappetein has received compensation to his institution for enrolment of patients in the trial from Abbott Vascular, and is an employee of Medtronic. G.W. Stone has received grants from Cardiovascular Research Foundation, during the conduct of the study, personal fees from Terumo, Amaranth, Medical Development Technologies, Shockwave, VALFIX, TherOx, Reva, Vascular Dynamics, Robocath, HeartFlow, Gore, Ablative Solutions, Matrizyme, Miracor, Neovasc, Vwave, Abiomed, Claret, Backbeat, and Sirtex, personal fees and other from Ancora, and Qool Therapeutics, and other from Cagent, Applied Therapeutics, Caliber, BioStar family of funds, MedFocus family of funds, and SpectraWave, outside the submitted work, and Columbia University, his employer, has received royalties from Abbott for sale of the MitraClip. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.