Abstract
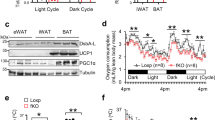
Cachexia represents a fatal energy-wasting syndrome in a large number of patients with cancer that mostly results in a pathological loss of skeletal muscle and adipose tissue. Here we show that tumor cell exposure and tumor growth in mice triggered a futile energy-wasting cycle in cultured white adipocytes and white adipose tissue (WAT), respectively. Although uncoupling protein 1 (Ucp1)-dependent thermogenesis was dispensable for tumor-induced body wasting, WAT from cachectic mice and tumor-cell-supernatant-treated adipocytes were consistently characterized by the simultaneous induction of both lipolytic and lipogenic pathways. Paradoxically, this was accompanied by an inactivated AMP-activated protein kinase (Ampk), which is normally activated in peripheral tissues during states of low cellular energy. Ampk inactivation correlated with its degradation and with upregulation of the Ampk-interacting protein Cidea. Therefore, we developed an Ampk-stabilizing peptide, ACIP, which was able to ameliorate WAT wasting in vitro and in vivo by shielding the Cidea-targeted interaction surface on Ampk. Thus, our data establish the Ucp1-independent remodeling of adipocyte lipid homeostasis as a key event in tumor-induced WAT wasting, and we propose the ACIP-dependent preservation of Ampk integrity in the WAT as a concept in future therapies for cachexia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Fearon, K.C., Glass, D.J. & Guttridge, D.C. Cancer cachexia: mediators, signaling and metabolic pathways. Cell Metab. 16, 153–166 (2012).
Dewys, W.D. et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Am. J. Med. 69, 491–497 (1980).
Mondello, P. et al. Cancer cachexia syndrome: pathogenesis, diagnosis and new therapeutic options. Nutr. Cancer 67, 12–26 (2015).
Theologides, A. Cancer cachexia. Cancer 43 (Suppl.), 2004–2012 (1979).
Jones, A. et al. TSC22D4 is a molecular output of hepatic wasting metabolism. EMBO Mol. Med. 5, 294–308 (2013).
Schäfer, M. et al. Ataxin-10 is part of a cachexokine cocktail triggering cardiac metabolic dysfunction in cancer cachexia. Mol. Metab. 5, 67–78 (2015).
Yu, Y.H. & Ginsberg, H.N. Adipocyte signaling and lipid homeostasis: sequelae of insulin-resistant adipose tissue. Circ. Res. 96, 1042–1052 (2005).
Agustsson, T. et al. Mechanism of increased lipolysis in cancer cachexia. Cancer Res. 67, 5531–5537 (2007).
Batista, M.L. Jr. et al. Adipose-tissue-derived factors as potential biomarkers in cachectic cancer patients. Cytokine 61, 532–539 (2013).
Pausch, T. et al. Cachexia but not obesity worsens the postoperative outcome after pancreatoduodenectomy in pancreatic cancer. Surgery 152, S81–S88 (2012).
Di Sebastiano, K.M. et al. Accelerated muscle and adipose tissue loss may predict survival in pancreatic cancer patients: the relationship with diabetes and anemia. Br. J. Nutr. 109, 302–312 (2013).
Petruzzelli, M. et al. A switch from white to brown fat increases energy expenditure in cancer-associated cachexia. Cell Metab. 20, 433–447 (2014).
Kir, S. et al. Tumor-derived PTH-related protein triggers adipose tissue browning and cancer cachexia. Nature 513, 100–104 (2014).
Xu, L., Zhou, L. & Li, P. CIDE proteins and lipid metabolism. Arterioscler. Thromb. Vasc. Biol. 32, 1094–1098 (2012).
Zhou, Z. et al. Cidea-deficient mice have lean phenotype and are resistant to obesity. Nat. Genet. 35, 49–56 (2003).
Laurencikiene, J. et al. Evidence for an important role of CIDEA in human cancer cachexia. Cancer Res. 68, 9247–9254 (2008).
Blum, D. et al. Cancer cachexia: a systematic literature review of items and domains associated with involuntary weight loss in cancer. Crit. Rev. Oncol. Hematol. 80, 114–144 (2011).
Hardie, D.G., Ross, F.A. & Hawley, S.A. AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat. Rev. Mol. Cell Biol. 13, 251–262 (2012).
Dzamko, N. et al. AMPK-β1 deletion reduces appetite, preventing obesity and hepatic insulin resistance. J. Biol. Chem. 285, 115–122 (2010).
Gaidhu, M.P., Bikopoulos, G. & Ceddia, R.B. Chronic AICAR-induced AMP-kinase activation regulates adipocyte lipolysis in a time-dependent and fat-depot-specific manner in rats. Am. J. Physiol. Cell Physiol. 303, C1192–C1197 (2012).
Gaidhu, M.P. et al. Prolonged AICAR-induced AMP kinase activation promotes energy dissipation in white adipocytes: novel mechanisms integrating HSL and ATGL. J. Lipid Res. 50, 704–715 (2009).
Anthony, N.M., Gaidhu, M.P. & Ceddia, R.B. Regulation of visceral and subcutaneous adipocyte lipolysis by acute AICAR-induced AMPK activation. Obesity (Silver Spring) 17, 1312–1317 (2009).
Boon, H. et al. Intravenous AICAR administration reduces hepatic glucose output and inhibits whole-body lipolysis in type 2 diabetic patients. Diabetologia 51, 1893–1900 (2008).
Bourron, O. et al. Biguanides and thiazolidinediones inhibit stimulated lipolysis in human adipocytes through activation of AMP-activated protein kinase. Diabetologia 53, 768–778 (2010).
Fearon, K. et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 12, 489–495 (2011).
Tanaka, Y. et al. Experimental cancer cachexia induced by transplantable colon 26 adenocarcinoma in mice. Cancer Res. 50, 2290–2295 (1990).
Sherry, B.A. et al. Anticachectin and tumor necrosis factor–α antibodies attenuate development of cachexia in tumor models. FASEB J. 3, 1956–1962 (1989).
Nowakowska, M., Pospiech, K., Lewandowska, U., Piastowska-Ciesielska, A.W. & Bednarek, A.K. Diverse effect of WWOX overexpression in HT29 and SW480 colon cancer cell lines. Tumour Biol. 35, 9291–9301 (2014).
Rosenberg, S.A., Spiess, P. & Lafreniere, R. A new approach to the adoptive immunotherapy of cancer with tumor-infiltrating lymphocytes. Science 233, 1318–1321 (1986).
Rydén, M. et al. Lipolysis—not inflammation, cell death or lipogenesis—is involved in adipose tissue loss in cancer cachexia. Cancer 113, 1695–1704 (2008).
Daval, M. et al. Antilipolytic action of AMP-activated protein kinase in rodent adipocytes. J. Biol. Chem. 280, 25250–25257 (2005).
Fullerton, M.D. et al. Single phosphorylation sites in Acc1 and Acc2 regulate lipid homeostasis and the insulin-sensitizing effects of metformin. Nat. Med. 19, 1649–1654 (2013).
Sullivan, J.E. et al. Inhibition of lipolysis and lipogenesis in isolated rat adipocytes with AICAR, a cell-permeable activator of AMP-activated protein kinase. FEBS Lett. 353, 33–36 (1994).
Djouder, N. et al. PKA phosphorylates and inactivates AMPK-α to promote efficient lipolysis. EMBO J. 29, 469–481 (2010).
Berriel Diaz, M. et al. Nuclear receptor cofactor receptor–interacting protein 140 controls hepatic triglyceride metabolism during wasting in mice. Hepatology 48, 782–791 (2008).
Das, S.K. et al. Adipose triglyceride lipase contributes to cancer-associated cachexia. Science 333, 233–238 (2011).
Thureson-Klein, A., Lagercrantz, H. & Barnard, T. Chemical sympathectomy of interscapular brown adipose tissue. Acta Physiol. Scand. 98, 8–18 (1976).
Kuraguchi, M. et al. Adenomatous polyposis coli (APC) is required for normal development of skin and thymus. PLoS Genet. 2, e146 (2006).
Tschöp, M.H. et al. A guide to analysis of mouse energy metabolism. Nat. Methods 9, 57–63 (2011).
Vegiopoulos, A. et al. Cyclooxygenase-2 controls energy homeostasis in mice by de novo recruitment of brown adipocytes. Science 328, 1158–1161 (2010).
Enerbäck, S. et al. Mice lacking mitochondrial uncoupling protein are cold-sensitive but not obese. Nature 387, 90–94 (1997).
Qi, J. et al. Downregulation of AMP-activated protein kinase by Cidea-mediated ubiquitination and degradation in brown adipose tissue. EMBO J. 27, 1537–1548 (2008).
Nordström, E.A. et al. A human-specific role of cell-death-inducing DFFA (DNA fragmentation factor–α)-like effector A (CIDEA) in adipocyte lipolysis and obesity. Diabetes 54, 1726–1734 (2005).
Kumar, N.B. et al. Cancer cachexia: traditional therapies and novel molecular-mechanism-based approaches to treatment. Curr. Treat. Options Oncol. 11, 107–117 (2010).
Lainscak, M., Filippatos, G.S., Gheorghiade, M., Fonarow, G.C. & Anker, S.D. Cachexia: common, deadly, with an urgent need for precise definition and new therapies. Am. J. Cardiol. 101 11A, 8E–10E (2008).
Jatoi, A. et al. A placebo-controlled, double-blind trial of infliximab for cancer-associated weight loss in elderly and/or poor performance non-small-cell lung cancer patients (N01C9). Lung Cancer 68, 234–239 (2010).
Tsoli, M. et al. Depletion of white adipose tissue in cancer cachexia syndrome is associated with inflammatory signaling and disrupted circadian regulation. PLoS One 9, e92966 (2014).
de Vos-Geelen, J., Fearon, K.C. & Schols, A.M. The energy balance in cancer cachexia revisited. Curr. Opin. Clin. Nutr. Metab. Care 17, 509–514 (2014).
Gauthier, M.S. et al. AMP-activated protein kinase is activated as a consequence of lipolysis in the adipocyte: potential mechanism and physiological relevance. J. Biol. Chem. 283, 16514–16524 (2008).
Vaughan, M. The production and release of glycerol by adipose tissue incubated in vitro. J. Biol. Chem. 237, 3354–3358 (1962).
Klein, S. & Wolfe, R.R. Whole-body lipolysis and triglyceride–fatty acid cycling in cachectic patients with esophageal cancer. J. Clin. Invest. 86, 1403–1408 (1990).
Tsoli, M., Swarbrick, M.M. & Robertson, G.R. Lipolytic and thermogenic depletion of adipose tissue in cancer cachexia. Semin. Cell Dev. Biol. 54, 68–81 (2016).
Wang, Z. et al. Homocysteine suppresses lipolysis in adipocytes by activating the AMPK pathway. Am. J. Physiol. Endocrinol. Metab. 301, E703–E712 (2011).
Deminice, R. et al. Creatine supplementation prevents hyperhomocysteinemia, oxidative stress and cancer-induced cachexia progression in Walker-256 tumor-bearing rats. Amino Acids http://dx.doi.org/10.1007/s00726-016-2172-9 (2016).
Diao, L. et al. Alternative mechanism for white adipose tissue lipolysis after thermal injury. Mol. Med. 21, 959 (2015).
Steinberg, G.R. et al. Tumor-necrosis-factor-α-induced skeletal muscle insulin resistance involves suppression of AMP kinase signaling. Cell Metab. 4, 465–474 (2006).
Livak, K.J. & Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCt method. Methods 25, 402–408 (2001).
Rodeheffer, M.S., Birsoy, K. & Friedman, J.M. Identification of white adipocyte progenitor cells in vivo. Cell 135, 240–249 (2008).
Rohm, M. et al. Transcriptional cofactor TBLR1 controls lipid mobilization in white adipose tissue. Cell Metab. 17, 575–585 (2013).
Jelenik, T. et al. AMP-activated protein kinase–α2 subunit is required for the preservation of hepatic insulin sensitivity by 'n – 3' polyunsaturated fatty acids. Diabetes 59, 2737–2746 (2010).
Hardie, D.G., Salt, I.P. & Davies, S.P. Analysis of the role of the AMP-activated protein kinase in the response to cellular stress. Methods Mol. Biol. 99, 63–74 (2000).
Dahlman, I. & Arner, P. Genetics of adipose tissue biology. Prog. Mol. Biol. Transl. Sci. 94, 39–74 (2010).
Kannt, A. et al. Association of nicotinamide-N-methyltransferase mRNA expression in human adipose tissue and the plasma concentration of its product, 1-methylnicotinamide, with insulin resistance. Diabetologia 58, 799–808 (2015).
Acknowledgements
We would like to thank K. Müller-Decker, K. Friedrich, D. Sohn, F. Ilmberger, Y. Feuchter, B. Meissburger, M. Kirilov, A. Vegiopoulos, P. Flachs, J. Hansikova, N. Petrovic and M. Christian for helpful discussions and experimental support and D.G. Hardie (University of Dundee) for Ampk-α1-specific and Ampk-α2-specific sheep antibodies. We particularly thank T. Schafmeier for comments on the manuscript. This work was supported by grants from the Swedish Cancer Fund (P.A.), the Deutsche Forschungsgemeinschaft grant He3260/8-1 (S.H.), the European Foundation for the Study of Diabetes (S.H.), the EU FP7 project DIABAT (HEALTH-F2-2011-278373; S.H.), the DKFZ–Bayer Cooperation Program (S.H.), the HGF Cross Program Topic 'Metabolic Dysfunction' (S.H.) and the HGF 'ICEMED' Program (S.H.).
Author information
Authors and Affiliations
Contributions
M.Rohm, M.S., V.L., B.E.Ü., K.N., C.A., O.H., T.P.S., A.Z., D.M., N.S.P., M.Ryden, A.K., I.D., P.A., N.P., B.C., E.-Z.A., B.E.K., G.R.S., P.J., J.K., C.W., M.B. and M.B.D. performed experiments and generated experimental tools; and S.H. designed and directed the research and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7 and Supplementary Table 1 (PDF 1072 kb)
Rights and permissions
About this article
Cite this article
Rohm, M., Schäfer, M., Laurent, V. et al. An AMP-activated protein kinase–stabilizing peptide ameliorates adipose tissue wasting in cancer cachexia in mice. Nat Med 22, 1120–1130 (2016). https://doi.org/10.1038/nm.4171
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4171
This article is cited by
-
Obesity and prostate cancer — microenvironmental roles of adipose tissue
Nature Reviews Urology (2023)
-
Blocking ActRIIB and restoring appetite reverses cachexia and improves survival in mice with lung cancer
Nature Communications (2022)
-
White adipose tissue-derived factors and prostate cancer progression: mechanisms and targets for interventions
Cancer and Metastasis Reviews (2022)
-
Obesity and cancer—extracellular matrix, angiogenesis, and adrenergic signaling as unusual suspects linking the two diseases
Cancer and Metastasis Reviews (2022)
-
The long noncoding RNA MALAT1 modulates adipose loss in cancer-associated cachexia by suppressing adipogenesis through PPAR-γ
Nutrition & Metabolism (2021)