Abstract
Vα24-invariant natural killer T cells (NKTs) have anti-tumor properties that can be enhanced by chimeric antigen receptors (CARs). Here we report updated interim results from the first-in-human phase 1 evaluation of autologous NKTs co-expressing a GD2-specific CAR with interleukin 15 (IL15) (GD2-CAR.15) in 12 children with neuroblastoma (NB). The primary objectives were safety and determination of maximum tolerated dose (MTD). The anti-tumor activity of GD2-CAR.15 NKTs was assessed as a secondary objective. Immune response evaluation was an additional objective. No dose-limiting toxicities occurred; one patient experienced grade 2 cytokine release syndrome that was resolved by tocilizumab. The MTD was not reached. The objective response rate was 25% (3/12), including two partial responses and one complete response. The frequency of CD62L+NKTs in products correlated with CAR-NKT expansion in patients and was higher in responders (n = 5; objective response or stable disease with reduction in tumor burden) than non-responders (n = 7). BTG1 (BTG anti-proliferation factor 1) expression was upregulated in peripheral GD2-CAR.15 NKTs and is a key driver of hyporesponsiveness in exhausted NKT and T cells. GD2-CAR.15 NKTs with BTG1 knockdown eliminated metastatic NB in a mouse model. We conclude that GD2-CAR.15 NKTs are safe and can mediate objective responses in patients with NB. Additionally, their anti-tumor activity may be enhanced by targeting BTG1. ClinicalTrials.gov registration: NCT03294954.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All requests for raw and analyzed data and materials should be directed to L.S.M. and will be promptly reviewed by the Baylor College of Medicine Licensing Group to verify if the request is subject to any intellectual property or confidentiality obligations. Patient-related data not included in the paper were generated as part of the clinical trial and may be subject to patient confidentiality. Any data and materials that can be shared will be released via a material transfer agreement. All raw data for single-cell sequencing are deposited in the Gene Expression Omnibus under accession number GSE223071. Source data are provided with this paper.
Change history
09 January 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41591-024-02799-w
References
Majzner, R. G. & Mackall, C. L. Clinical lessons learned from the first leg of the CAR T cell journey. Nat. Med. 25, 1341–1355 (2019).
Batra, S. A. et al. Glypican-3-specific CAR T cells coexpressing IL15 and IL21 have superior expansion and antitumor activity against hepatocellular carcinoma. Cancer Immunol. Res. 8, 309–320 (2020).
Mestermann, K. et al. The tyrosine kinase inhibitor dasatinib acts as a pharmacologic on/off switch for CAR T cells. Sci. Transl. Med. 11, eaau5907 (2019).
Liu, E. et al. Use of CAR-transduced natural killer cells in CD19-positive lymphoid tumors. N. Engl. J. Med. 382, 545–553 (2020).
Heczey, A. et al. Invariant NKT cells with chimeric antigen receptor provide a novel platform for safe and effective cancer immunotherapy. Blood 124, 2824–2833 (2014).
Makkouk, A. et al. Off-the-shelf Vδ1 gamma delta T cells engineered with glypican-3 (GPC-3)-specific chimeric antigen receptor (CAR) and soluble IL-15 display robust antitumor efficacy against hepatocellular carcinoma. J. Immunother. Cancer 9, e003441 (2021).
Courtney, A. N., Tian, G. & Metelitsa, L. S. Natural killer T cells and other innate-like T lymphocytes as emerging platforms for allogeneic cancer cell therapy. Blood 141, 869–876 (2022).
Poplack, D. G. & Pizzo, P. A. Principles and Practice of Pediatric Oncology 6th edn (LWW, 2010).
Yu, A. L. et al. Long-term follow-up of a phase III study of ch14.18 (dinutuximab) + cytokine immunotherapy in children with high-risk neuroblastoma: COG study ANBL0032. Clin. Cancer Res. 27, 2179–2189 (2021).
Dotti, G., Gottschalk, S., Savoldo, B. & Brenner, M. K. Design and development of therapies using chimeric antigen receptor-expressing T cells. Immunol. Rev. 257, 107–126 (2014).
Pule, M. A. et al. Virus-specific T cells engineered to coexpress tumor-specific receptors: persistence and antitumor activity in individuals with neuroblastoma. Nat. Med. 14, 1264–1270 (2008).
Louis, C. U. et al. Antitumor activity and long-term fate of chimeric antigen receptor-positive T cells in patients with neuroblastoma. Blood 118, 6050–6056 (2011).
Heczey, A. et al. CAR T cells administered in combination with lymphodepletion and PD-1 inhibition to patients with neuroblastoma. Mol. Ther. 25, 2214–2224 (2017).
Straathof, K. et al. Antitumor activity without on-target off-tumor toxicity of GD2-chimeric antigen receptor T cells in patients with neuroblastoma. Sci. Transl. Med. 12, eabd6169 (2020).
Kronenberg, M. & Gapin, L. The unconventional lifestyle of NKT cells. Nat. Rev. Immunol. 2, 557–568 (2002).
Metelitsa, L. S. et al. Human NKT cells mediate antitumor cytotoxicity directly by recognizing target cell CD1d with bound ligand or indirectly by producing IL-2 to activate NK cells. J. Immunol. 167, 3114–3122 (2001).
Song, L. et al. Vα24-invariant NKT cells mediate antitumor activity via killing of tumor-associated macrophages. J. Clin. Invest 119, 1524–1536 (2009).
Cortesi, F. et al. Bimodal CD40/Fas-dependent crosstalk between iNKT cells and tumor-associated macrophages impairs prostate cancer progression. Cell Rep. 22, 3006–3020 (2018).
Godfrey, D. I., MacDonald, H. R., Kronenberg, M., Smyth, M. J. & Van Kaer, L. NKT cells: what’s in a name? Nat. Rev. Immunol. 4, 231–237 (2004).
Metelitsa, L. S. et al. Natural killer T cells infiltrate neuroblastomas expressing the chemokine CCL2. J. Exp. Med. 199, 1213–1221 (2004).
Tachibana, T. et al. Increased intratumor Vα24-positive natural killer T cells: a prognostic factor for primary colorectal carcinomas. Clin. Cancer Res. 11, 7322–7327 (2005).
Molling, J. W. et al. Low levels of circulating invariant natural killer T cells predict poor clinical outcome in patients with head and neck squamous cell carcinoma. J. Clin. Oncol. 25, 862–868 (2007).
Motohashi, S., Okamoto, Y., Yoshino, I. & Nakayama, T. Anti-tumor immune responses induced by iNKT cell-based immunotherapy for lung cancer and head and neck cancer. Clin. Immunol. 140, 167–176 (2011).
Exley, M. A. et al. Adoptive transfer of invariant NKT cells as immunotherapy for advanced melanoma: a phase I clinical trial. Clin. Cancer Res. 23, 3510–3519 (2017).
Motohashi, S. et al. A phase I-II study of α-galactosylceramide-pulsed IL-2/GM-CSF-cultured peripheral blood mononuclear cells in patients with advanced and recurrent non-small cell lung cancer. J. Immunol. 182, 2492–2501 (2009).
Yamasaki, K. et al. Induction of NKT cell-specific immune responses in cancer tissues after NKT cell-targeted adoptive immunotherapy. Clin. Immunol. 138, 255–265 (2011).
Exley, M. A. et al. Adoptive transfer of invariant NKT cells as immunotherapy for advanced melanoma: a phase 1 clinical trial. Clin. Cancer Res. 23, 3510–3519 (2017).
Heczey, A. et al. Anti-GD2 CAR-NKT cells in patients with relapsed or refractory neuroblastoma: an interim analysis. Nat. Med. 26, 1686–1690 (2020).
Dudley, M. E. et al. Adoptive cell therapy for patients with metastatic melanoma: evaluation of intensive myeloablative chemoradiation preparative regimens. J. Clin. Oncol. 26, 5233–5239 (2008).
Mody, R. et al. Irinotecan-temozolomide with temsirolimus or dinutuximab in children with refractory or relapsed neuroblastoma (COG ANBL1221): an open-label, randomised, phase 2 trial. Lancet Oncol. 18, 946–957 (2017).
Yu, A. L. et al. Phase I trial of a human-mouse chimeric anti-disialoganglioside monoclonal antibody ch14.18 in patients with refractory neuroblastoma and osteosarcoma. J. Clin. Oncol. 16, 2169–2180 (1998).
Yu, A. L. et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N. Engl. J. Med. 363, 1324–1334 (2010).
Park, J. R. et al. Revisions to the International Neuroblastoma Response Criteria: a consensus statement from the National Cancer Institute Clinical Trials Planning Meeting. J. Clin. Oncol. 35, 2580–2587 (2017).
Liu, D. et al. IL-15 protects NKT cells from inhibition by tumor-associated macrophages and enhances antimetastatic activity. J. Clin. Invest. 122, 2221–2233 (2012).
Klebanoff, C. A. et al. Central memory self/tumor-reactive CD8+ T cells confer superior antitumor immunity compared with effector memory T cells. Proc. Natl Acad. Sci. USA 102, 9571–9576 (2005).
Graef, P. et al. Serial transfer of single-cell-derived immunocompetence reveals stemness of CD8+ central memory T cells. Immunity 41, 116–126 (2014).
Gattinoni, L. et al. Acquisition of full effector function in vitro paradoxically impairs the in vivo antitumor efficacy of adoptively transferred CD8+ T cells. J. Clin. Invest. 115, 1616–1626 (2005).
Tian, G. et al. CD62L+ NKT cells have prolonged persistence and antitumor activity in vivo. J. Clin. Invest. 126, 2341–2355 (2016).
Decarolis, B. et al. Iodine-123 metaiodobenzylguanidine scintigraphy scoring allows prediction of outcome in patients with stage 4 neuroblastoma: results of the Cologne Interscore Comparison Study. J. Clin. Oncol. 31, 944–951 (2013).
Ngai, H. et al. IL-21 selectively protects CD62L+ NKT cells and enhances their effector functions for adoptive immunotherapy. J. Immunol. 201, 2141–2153 (2018).
Ngai, H. et al. LEF1 drives a central memory program and supports antitumor activity of natural killer T cells. Cancer Immunol. Res. 11, 171–183 (2023).
Schober, S. L. et al. Expression of the transcription factor lung Krüppel-like factor is regulated by cytokines and correlates with survival of memory T cells in vitro and in vivo. J. Immunol. 163, 3662–3667 (1999).
Hwang, S. S. et al. mRNA destabilization by BTG1 and BTG2 maintains T cell quiescence. Science 367, 1255–1260 (2020).
Del Bufalo, F. et al. GD2-CART01 for relapsed or refractory high-risk neuroblastoma. N. Engl. J. Med. 388, 1284–1295 (2023).
Maude, S. L. et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N. Engl. J. Med. 378, 439–448 (2018).
Gattinoni, L. et al. A human memory T cell subset with stem cell-like properties. Nat. Med. 17, 1290–1297 (2011).
Xu, Y. et al. Closely related T-memory stem cells correlate with in vivo expansion of CAR.CD19-T cells and are preserved by IL-7 and IL-15. Blood 123, 3750–3759 (2014).
Giles, J. R. et al. Shared and distinct biological circuits in effector, memory and exhausted CD8+ T cells revealed by temporal single-cell transcriptomics and epigenetics. Nat. Immunol. 23, 1600–1613 (2022).
Long, A. H. et al. 4-1BB costimulation ameliorates T cell exhaustion induced by tonic signaling of chimeric antigen receptors. Nat. Med. 21, 581–590 (2015).
Weber, E. W. et al. Transient rest restores functionality in exhausted CAR-T cells through epigenetic remodeling. Science 372, eaba1786 (2021).
Good, C. R. et al. An NK-like CAR T cell transition in CAR T cell dysfunction. Cell 184, 6081–6100(2021).
John, L. B. et al. Anti-PD-1 antibody therapy potently enhances the eradication of established tumors by gene-modified T cells. Clin. Cancer Res. 19, 5636–5646 (2013).
Keshelava, N. et al. Histone deacetylase 1 gene expression and sensitization of multidrug-resistant neuroblastoma cell lines to cytotoxic agents by depsipeptide. J. Natl Cancer Inst. 99, 1107–1119 (2007).
Xu, X. et al. NKT cells coexpressing a GD2-specific chimeric antigen receptor and IL15 show enhanced in vivo persistence and antitumor activity against neuroblastoma. Clin. Cancer Res. 25, 7126–7138 (2019).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat. Methods 16, 1289–1296 (2019).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573–3587 (2021).
Acknowledgements
The authors are grateful to M. Brenner, H. Heslop and personnel of the cGMP facility at the Center for Cell and Gene Therapy for manufacturing CAR-NKTs, including A. Jacques, J. Sritabal-Ramirez, H. Hu, K. Matzar and R. Al Hussien. We also thank K. Kukreja of the Interventional Radiology section and P. Srivaths, director of the Pheresis Service, of Texas Children’s Hospital, as well as staff of the Flow Cytometry Core Laboratory of the Texas Children’s Cancer and Hematology Center and the Single Cell Genomics Core at Baylor College of Medicine, for excellent technical assistance. This work was supported by grants or contracts from Alex’s Lemonade Stand Foundation for Childhood Cancer, St. Baldrick’s Foundation, the American Cancer Society (to L.S.M. and A.H.) and Athenex, Inc. We thank the Cancer Prevention and Research Institute of Texas (CPRIT) for support under grant no. RP180785.
Author information
Authors and Affiliations
Contributions
A.H. and L.S.M. designed the clinical trial. A.H. wrote the clinical protocol and was the principal investigator of the clinical trial. G.D., L.S.M., A.H., X.X. and G.T. developed the CAR construct selected for the trial and tested it in NKT cells. A.H., A.C.S. and B.D.W. performed pre-therapy and post-therapy patient clinical evaluation. H.Z. and B.M. generated CAR-NKT cell products in the cGMP facility. A.N.C., C.M.A., N.G., S.G.T. and P.R. processed clinical samples and performed flow cytometry, qPCR and Luminex. X.X. performed serial tumor challenge assay. A.M., M.S., C.X., C.S. and D.K.W. performed and analyzed scRNA-seq. C.Z. analyzed bulk RNA-seq. X.X., G.A.B., M.S.W., T.D. and Y.L. tested in vitro BTG1 function in NKT and T cells. X.X. and L.G. performed therapeutic experiments in mice. B.G. and T.W. provided regulatory and statistical support for the clinical trial. The manuscript was written by A.H. and L.S.M. and edited by E.J.D.P. All authors discussed and interpreted results.
Corresponding authors
Ethics declarations
Competing interests
A.H., A.N.C., G.T., X.X, G.D. and L.S.M. are co-inventors on pending patent applications that relate to the use of NKTs in cancer immunotherapy, including those that have been licensed by Baylor College of Medicine to Athenex, Inc. for commercial development. Athenex, Inc. provided research support for this project (to L.S.M.) via a sponsored research agreement with Baylor College of Medicine. G.A.B., L.G., C.M.A., N.G., P.R., M.S.W., Y.L., C.Z., T.D., E.J.D.P., A.C.S., H.Z., B.M., S.G.T., B.G., T.W., B.D.W., A.M., M.S., C.X., C.S. and D.K.W. declare no competing financial interests.
Peer review
Peer review information
Nature Medicine thanks Joseph Fraietta, Beibei Guo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Saheli Sadanand, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Consort flow diagram summarizing enrollment on the GINAKIT2 study.
Enrollment is conducted in two phases: procurement (manufacturing of the cell product) and treatment (infusion of the cell product). The study is a single arm, Phase 1 clinical trial and patients were enrolled on a first come/first served basis. Received allocated intervention on DL1: 3, DL2: 3, DL3: 3 and DL4 4 patients.
Extended Data Fig. 2 Serum cytokine and chemokine levels in patients infused with GD2-CAR.15 NKTs.
A. Mean fold change (FC) compared to baseline (day −4) of 38 evaluated cytokines and chemokines in patient peripheral blood samples collected at indicated timepoints quantified by Luminex. B. Absolute values (pg/mL) of IL1, IL6 and TNFbeta over four weeks in all patients.
Extended Data Fig. 3 Frequency and severity of adverse events following first and second GD2-CAR.15 NKT infusions.
Toxicity parameters were assessed and graded according to the Common Terminology Criteria for Adverse Events version 4 from the start of lymphodepletion (day −4) until four weeks after each infusion (day 28). n = 4 patients. Data presented as mean +/− SD.
Extended Data Fig. 4 Antitumor response in patient 12.
Pre- and post-GD2-CAR NKT infusion images from MIBG scans. Planar images (top row) and fused SPECT-CT images (bottom row) show pelvic bone metastasis (red circle) visible prior to infusion (left column) and complete resolution after infusion (right column). Note: MIBG-avid regions in the middle of the image correspond to bladder with urine containing MIBG.
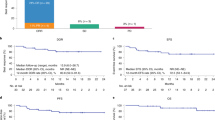
Extended Data Fig. 5 Long-term expansion and persistence of GD2-CAR.15 NKTs in patients with relapsed or refractory neuroblastoma.
A. Peripheral blood (PB) samples were collected at indicated timepoints and the CAR transgene was detected by quantitative PCR. Patients 10 and 12 were reinfused at approximately week 8 (W8); patients 2 and 11 were reinfused at approximately three months (M3). B. AUC of peripheral blood CAR-NKT absolute numbers in four patients receiving repeat infusions. Two-tailed paired T test.
Extended Data Fig. 6 BTG1 expression is elevated in exhausted CAR-NKTs.
A. Cytotoxicity of CAR-NKTs from patient pre-infusion products against CHLA255 NB cells over the course of five repeat co-culture cycles. B. UMAP projections of gene expression profiles measured by scRNAseq from pre-infusion products (IP) and CAR-NKTs following five-cycle repeat co-culture with tumor cells (5RcC). C. UMAP projection of gene expression in CAR-NKTs from pre-infusion products (IP), post-5RcC (5RcC), and isolated from peripheral blood (PB) post-infusion. D, E. Volcano plots showing differentially expressed genes in pre-infusion products versus peripheral blood CAR-NKTs (D) and versus post-5RcC CAR-NKTs (E).
Extended Data Fig. 7 Overexpression (OE) of BTG1 reduces global RNA expression and proliferative capacity in NKTs.
A. Total RNAseq reads from BTG1-OE and control NKTs. Red and blue lines indicate fold change from nuclear or mitochondrial transcripts, respectively. B. Volcano plot showing differentially expressed genes in BTG1-OE NKTs versus control NKTs. Blue vertical lines correspond to two-fold change on log2 scale; green dashed and solid lines represent p < 0.05 and <0.01, respectively. C. Pathway enrichment analysis showing gene expression programs enriched in BTG1-OE NKTs. Fisher’s exact test was used to calculate the probability of observing overlap between the input gene set and the pathway or gene set database by chance. P-values were adjusted for multiple testing using the Benjamini-Hochberg method to control for false discovery rate. D. Fold expansion of BTG1-OE vs control NKTs, n = 6 donors, two-tailed paired T test. E, F. Survival of NKTs stimulated with anti-CD3/CD28 monoclonal antibodies and evaluated with annexin V and fixable viability dye e780 on day 3, n = 4 (E) and CellTrace Violet dilution measured on day 5, n = 3 (F), (E-F data presented as mean +/− SD: two-tailed paired T test).
Supplementary information
Supplementary Information
Supplementary Figs. 1–11 with legends.
Supplementary Tables 1
Supplementary Tables 1–7 in combined workbook with multiple tabs.
Supplementary Data 1
Source data for Supplementary Figs. 1, 3–5 and 7–10.
Supplementary Note
Protocol
Source data
Source Data Fig. 1
Statistical source data.
Source Data Extended Data Fig./Table 3
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heczey, A., Xu, X., Courtney, A.N. et al. Anti-GD2 CAR-NKT cells in relapsed or refractory neuroblastoma: updated phase 1 trial interim results. Nat Med 29, 1379–1388 (2023). https://doi.org/10.1038/s41591-023-02363-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-023-02363-y
This article is cited by
-
Identification of cancer-specific cell surface targets for CAR-T cell therapy
Inflammation and Regeneration (2024)
-
Immunoengineering can overcome the glycocalyx armour of cancer cells
Nature Materials (2024)
-
Approval of DFMO for high-risk neuroblastoma patients demonstrates a step of success to target MYC pathway
British Journal of Cancer (2024)
-
IL-12 reprograms CAR-expressing natural killer T cells to long-lived Th1-polarized cells with potent antitumor activity
Nature Communications (2024)
-
Reprogramming T cell differentiation and exhaustion in CAR-T cell therapy
Journal of Hematology & Oncology (2023)