Abstract
Background
Cigarette smoking is a threat to global human health and a leading cause of the cardiovascular disease (CVD) morbidity and mortality. Importantly, sex-specific differences in smoking-induced arterial stiffness, an early key event in the development of atherosclerotic CVD, remain still elusive. Thus, this study sought out to investigate sex-specific associations between smoking and measures of arterial stiffness.
Methods and results
Overall, 15,010 participants (7584 men and 7426 women aged 35–74 years) of the Gutenberg Health Study were examined at baseline during 2007–2012. Smoking status, pack-years of smoking, and years since quitting smoking were assessed by a standardized computer-assisted interview. Arterial stiffness and wave reflection were determined by stiffness index (SI) and augmentation index (AI). In the total sample, 45.8% had never smoked, 34.7% were former smokers, and 19.4% were current smokers. Median cumulative smoking exposure was 22.0 pack-years in current male smokers and 16.0 in current female smokers. In general, multivariable linear regression models adjusted for a comprehensive set of confounders revealed that smoking status, pack-years of smoking, and years since quitting smoking were dose-dependently associated with markers of arterial stiffness. In sex-specific analyses, these associations were overall more pronounced in men and SI was stronger related to the male sex, whereas differences between men and women in the case of AI appeared to be less substantial.
Discussion
The present results indicate that chronic smoking is strongly and dose-dependently associated with increased arterial stiffness in a large population-based cohort regardless of sex but with a stronger association in men.
Similar content being viewed by others
Introduction
Cigarette smoking represents one of the biggest (preventable) threats to public health. It is a leading cause of morbidity, disability, and death worldwide. Approximately every six seconds one person dies due to tobacco and sequelae, accounting for one of five deaths worldwide [1]. In line, a recent report from the World Health Organization (WHO) concluded that tobacco use kills up to half of its users and worldwide more than 8 million people each year, a major part caused by cardiovascular diseases (CVD) [2]. Among the risk factors for CVD, exposure to cigarette smoke is presumably one of the most complex and sparsely understood risk factors, containing more than 4,000 identified chemical compounds with a wide range of toxicity and sizes from atoms to particulate matter [3]. In particular, sex-specific differences in smoking-induced pathophysiological mechanisms remain largely unknown. There is a large body of evidence suggesting that cigarette smoking disturbs vascular endothelial homeostasis by reducing the bioavailability of vascular nitric oxide (NO), mainly via the formation of oxidative stress and inflammatory processes [4]. Since the formation of NO plays a key role for the endothelium to perpetuate its vasodilatory, antithrombotic, anti-inflammatory, and antioxidant functions, this pathological state promotes endothelial dysfunction and atherosclerotic plaque formation, ultimately leading to structural changes in the arterial wall and arterial stiffening [5, 6]. Importantly, arterial stiffness has been shown to be an independent risk factor for CVD and all-cause mortality after adjustment for traditional cardiovascular risk factors [7], in addition to being a more potent CVD risk factor in women than in men [8]. Moreover, the assessment of aortic stiffness in the Framingham Heart Study improved risk prediction for the first cardiovascular event when added to a standard risk factor model [9]. Of note, smoking exposure even at low intensity in teenage years was individually and in combination with alcohol consumption associated with increased arterial stiffness [10, 11]. Notable, current smoking does not only influence the arterial vascular system, but also the venous system with an increased risk for venous thromboembolism [12]. However, substantial sex differences were observed in the development of arterial stiffness, not only in the time course of aging-related arterial stiffness and the associated risk of CVD, but also in the context of CVD risk factors such as smoking, diabetes mellitus, and obesity [13]. Thus, the aim of the present study was to examine the sex-specific associations between smoking and markers of arterial stiffness and wave reflection in a large population-based cohort.
Methods
Study procedure and sample
As described by Wild et al. in detail, the Gutenberg Health Study (GHS) is a population-based, prospective, observational single-center cohort study from Mid-Western Germany, including residents of the City of Mainz and the region Mainz-Bingen [14]. At baseline, 15,010 individuals, aged 35 to 74 years and stratified 1:1 for sex, residence (urban and rural), and decades of age, were examined between April 2007 and April 2012 at the University Medical Center Mainz, Germany. All procedures in the GHS were approved by the ethics committee of the Statutory Physician Board of the State Rhineland-Palatinate, Germany (reference number 837.020.07(5555)) and the local data safety commissioners. The study design was in line with the Declaration of Helsinki and principles outlined in the recommendations for Good Clinical and Epidemiological Practice. Participants were included after written informed consent. The GHS mainly focuses on the analysis of cardiovascular risk factors and improvement of risk stratification. Moreover, determinants of metabolic, ophthalmological, cancer, immune system, and mental diseases are of interest. Participants underwent a range of standardized examinations according to standard operating procedures, including a comprehensive assessment of clinical, laboratory, lifestyle, psychosocial, and environmental parameters. Quality control of all data and screening for completeness according to predefined algorithms and plausibility criteria were performed by a central data management unit.
Smoking variables
A standardized computer-assisted interview was conducted to collect information about smoking history, including smoking status, pack-years of smoking in former and current smokers, and years since quitting in former smokers.
With respect to their smoking status, participants were categorized as non-smokers, former smokers, or current smokers. Current smoking comprised regular or daily smoking (at least 1 cigarette per day, 7 per week, or 1 pack per month) for at least the past 6 months. The group of non-smokers included non-daily and non-regular smokers. Former smokers were those who had a history of smoking (regular or daily smoking) for longer than 6 months and who were no current smokers. To determine the pack-years of smoking, current and former smokers were asked for the year of smoking initiation/cessation and average consumption of cigarettes per day. This was calculated as the average number of cigarettes smoked per day divided by 20 (a pack) and multiplied by the number of years smoked. Pack-years of smoking as a cumulative exposure indicator of smoking burden were used to adequately address both intensity and duration of smoking. Exposure to passive smoke in never and former smokers was defined as being exposed to cigarette smoke at home, workplace, and/or elsewhere (e.g. bars, clubs, restaurants) for at least half an hour per day. Participants were asked not to smoke for at least 8 h prior to the examination to avoid the acute effects of smoking.
Assessment of arterial stiffness and wave reflection
Briefly, stiffness index (SI) and augmentation index (AI) were assessed in dark, air-conditioned rooms (room temperature 23 to 25 °C) after at least 5 min of rest in the supine position. All participants were advised to come in a fasted state of at least 8 h. Subjects were particularly advised to refrain from nicotine, caffeine, alcohol, vitamins, and physical activity before measurement. The AI was determined by digital volume plethysmography using an EndoPat 2000 device (Itamar Medical, Caesarea, Israel), which is based on the fingertip measurement of pulsatile volume changes. The AI is automatically calculated by identifying the early (P1) and late systolic peak (P2) with the following formula: (P2 − P1)/P1 × 100. The SI was assessed by digital photoplethysmography (PCA2 device; Carefusion) and used as a measure for systemic arterial stiffness. Briefly, a volume pulse waveform with an early systolic and a second diastolic/reflected peak was recorded by the transmission of infrared light through the finger pulp. The SI was calculated as the subject’s height (meters) divided by the time difference between these 2 peaks (so‐called “peak‐to‐peak time”) in seconds. Both measurements were performed simultaneously according to standard operating procedures with calibration for the device used and detailed quality control. Detailed description of this method has been provided recently [15, 16].
Definitions of further included variables
Prevalent CVD were assessed on basis of medical history or diagnosed during the study visit. Prevalent CVD was defined as the presence of any of the following diseases: coronary artery disease, peripheral artery disease, myocardial infarction, congestive heart failure, stroke, or atrial fibrillation. Medication use was assessed on basis of medical records as well as personal reports and was categorized according to the Anatomical Therapeutic Chemical Classification System [17]. Arterial hypertension was diagnosed by the intake of antihypertensive drugs or a mean systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg at rest (average of 2nd and 3rd standardized measurement after 8 and 11 min of rest). Waist-to-height ratio was calculated as waist circumference in centimeters divided by the body height in centimeters. Heart rate was assessed by the mean of the 2nd and 3rd measurements at rest. Diabetes mellitus was defined by any of the following: diagnosed by a physician, antidiabetic treatment, fasting blood glucose level (overnight fast of at least 8 h) ≥ 126 mg/dL, non-fasting blood glucose level (less than 8 h of fasting) ≥ 200 mg/dL, or HbA1c ≥ 6.5%. Dyslipidemia was present in the case of a physician diagnosis of dyslipidemia, low-density lipoprotein cholesterol/high-density lipoprotein cholesterol ratio > 3.5, or triglycerides ≥ 150 mg/dL. A positive history of myocardial infarction or stroke was recorded in a female first-degree relative ≤ 65 years or in a male first-degree relative ≤ 60 years. Socioeconomic status was assessed in accordance with Lampert et al. by a validated index score (ranging from 3 to 21), providing information about educational background, current occupation, and salary [18]. The categories “beneath” and “above tolerable limit” were used to characterize alcohol consumption (cut-offs were > 24 g per day for men and > 12 g per day for women) [19]. A Patient Health Questionnaire (PHQ-9) score ≥ 10 was used for the caseness of depression [20]. The Short Questionnaire to Assess Health-enhancing physical activity (SQUASH), which comprises questions on multiple activities to calculate an index score (total minutes of activity multiplied by intensity), was used to determine physical activity [21]. Postmenopausal status, intake of oral contraceptives, and hormone replacement therapy in women were assessed by medical records and personal reports.
Statistical analysis
The main analyses were carried out sex-specifically, while the supplemental material provides analyses for the total sample. Study sample characteristics are shown according to sex as absolute and relative frequency for categorical variables and as mean value and standard deviation or median with 25th and 75th percentiles for continuous variables. Linear regression analysis with corresponding beta estimates (β) was used to assess the association between smoking status, pack-years of smoking in former and current smokers, and years since quitting smoking in former smokers with markers of arterial stiffness and wave reflection. Models were adjusted sequentially:
Model 1 (basic model): Adjustment for age (continuous). Linear regressions for the parameter AI were additionally adjusted for height and heart rate (both as continuous variables). In women, further adjustment for postmenopausal status, intake of oral contraceptives, and hormone replacement therapy were done (all binary).
Model 2 (comprehensive model): Further adjustment for arterial hypertension (binary), diabetes mellitus (binary), waist-to-height ratio (continuous), dyslipidemia (binary), family history of myocardial infarction or stroke (binary), socioeconomic status (binary), alcohol consumption above the tolerable limit (binary), depression (binary), physical activity (continuous), passive smoking (binary, when applicable), smoking prior to the examination (binary, when applicable), prevalent CVD (binary, as defined), and medication use (binary for diabetic drugs, antithrombotic agents, antihypertensive drugs, diuretics, beta-blockers, calcium channel blockers, agents acting on the renin–angiotensin–aldosterone system, and lipid modifying agents).
All regression analyses were performed on subjects with complete data for smoking exposure variables and other confounding variables included in the models. To confirm the robustness of the cross-sectional results, we further prospectively (follow-up data obtained from 2012 to 2017) analyzed the association between smoking status and markers of arterial stiffness and wave reflection. Effect estimates are given with 95% confidence intervals (CI) with corresponding p values. Because of the explorative nature of the study, p values should be treated as a continuous measure of the statistical strength of an association, and they are therefore reported exactly. The statistical data analyses were performed using the software R, version 4.1.0 (http://www.r-project.org/).
Results
Study sample characteristics
In total, 6863 (45.8%) individuals were never-smokers, while 5201 (34.7%) smoked in former times, and 2911 (19.4%) were current smokers (Supplementary Table S1). As evident in Table 1, men had in general a higher socioeconomic status, lower prevalence of depression, and higher prevalence of alcohol consumption above the tolerable limit compared to women. Men were more likely to be current smokers and had higher cumulative smoking exposure in terms of pack-years. Concerning traditional cardiovascular risk factors and CVD, women expressed an overall favorable risk profile with lower prevalences of arterial hypertension, diabetes mellitus, dyslipidemia, congestive heart failure, coronary artery disease, myocardial infarction, stroke, and peripheral artery disease. Consequently, overall use of medication was higher among men than in women. With regard to markers of arterial stiffness, men had higher SI, whereas women displayed higher AI. There was a steady increase of SI and AI from never-smokers to former and current smokers among men (SI: 8.01 ± 2.28 m/s–8.54 ± 2.34 m/s–8.64 ± 2.31 m/s; AI: 7.50 ± 17.46%–13.40 ± 18.25%–14.73 ± 19.54%) and women (SI: 6.61 ± 1.66 m/s–6.69 ± 1.66 m/s–6.79 ± 1.80 m/s; AI: 22.32 ± 19.97%–23.95 ± 20.01%–27.46 ± 22.74%).
Association between measures of arterial stiffness and smoking exposure
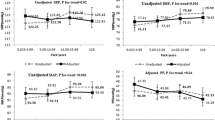
In the total sample, smoking status was independently associated with SI and AI in a dose-dependent manner after comprehensive adjustment (Supplementary Table S2 and Fig. S1). Sex-specific analyses showed in general a comparable pattern with higher effect estimates for men compared to women, while smoking status was not predictive of SI in model 2 after comprehensive adjustment (Table 2). The prospective analyses on the association between smoking status and SI and AI could confirm the cross-sectional results (Table 3).
Likewise, increasing number of pack-years in the current (Supplementary Table S3 and Fig. S2) as well as in former smokers (Supplementary Table S6) was independently associated with SI and AI in a dose-dependent manner in the total sample. The pattern of results found for the impact of heavy smoking in current smokers was similar, showing that effect estimates for SI and AI were more than two-fold increased when comparing < 20 vs. ≥ 20 pack-years (Supplementary Table S4). Sex-specific analyses revealed pack-years of smoking in the current (Table 4) and former smokers (Table 5) as well as heavy smoking (Table 6) to be independently associated with SI and AI in a dose-dependent manner with lower and overall less monotone effect estimates for women than men.
Augmentation index was independently and inversely associated with years since quitting smoking in former smokers and followed a dose-dependent relationship, whereas the independent and invers association with SI resulted in a rather non-linear weaker relationship in the total sample (Supplementary Table S5). This was also observed in the case of the sex-specific analyses, showing that SI was less linearly and weakly related to years since quitting smoking in both men and women with overall stronger effect estimates for men. In the case of AI, a dose-dependent association with years since quitting smoking was observed in men, whereas this association was less monotone and weaker in women (Table 7).
Discussion
In the present study, sex-specific associations between chronic current as well as former cigarette smoking and arterial stiffness quantified by SI and AI were investigated in a large population-based cohort. Regardless of sex, smoking was dose-dependently associated with increased arterial stiffness and wave reflection. Fortunately, an increasing number of years since quitting smoking in former smokers was associated with an improvement in arterial compliance in both sexes. The portion of current smokers and consumed pack-years were higher in men than in women in the present study. In line, women overall revealed a more beneficial cardiovascular risk profile compared to men and were associated with less cardiovascular comorbidities. Arterial stiffness (SI) was higher in men than in women and both AI and SI had a higher correlation to current smoking in men than in women in linear regression. With raising pack-years a higher correlation to arterial stiffness was revealed in both sexes, whereas this effect was stronger in men. In men and women heavy smoking correlated with increased arterial stiffness, but male sex was associated with higher values of AI and SI in heavy smokers compared to the female sex. In line with these findings, the regression of arterial stiffness after quitting smoking was present in both sexes, but AI and SI declined stronger in men than in women. Of interest, prospective analyses revealed an association between current as well as former smoking and SI in men but not in women after further adjustment in linear regression models. AI, in contrast, was associated with current smoking but not with former smoking in both sexes. Altogether, the present study indicates that smoking may constitute an independent risk factor for increased arterial stiffness and wave reflection in both men and women.
To our knowledge, this is the first assessment of the sex-specific association between current and former cigarette smoking and arterial stiffness measured by SI and AI in a large population-based cohort. In accordance with the literature [22, 23], in the present study the prevalence of smoking was higher in men than in women. Until now, only a little amount of literature exists on possible sex differences regarding arterial stiffness due to smoking. In many available studies, the explanatory power is largely hampered by small numbers of study participants. In line with the results of the present study, an investigation of 147 smokers by Mozos et al. revealed a higher cumulative smoking exposure (pack-years) and an unbeneficial cardiovascular risk profile in men compared to women. The authors also found that an elevation of arterial stiffness required less exposure to cigarette smoke in women compared to men [24], which goes along with the results of the present study. Besides these findings, arterial stiffness increase was associated with smoking intensity (pack-years) in the overall sample, but no further sex differences regarding arterial stiffness and smoking were detected. Contrary to the findings of Mozos et al. [24], in the present study heavy smokers revealed higher values of arterial stiffness in both sexes, but in men a worse effect on SI and AI was seen compared to women, the results of the present study revealed lower arterial stiffening in women compared to men. In a Japanese study on more than 6,500 healthy subjects, in whom AI was measured, wave reflection was higher in women than in men, although the interaction of blood pressure and smoking with arterial stiffness was observed only in men. The authors concluded that smoking/hypertension interaction might be more detrimental regarding arterial stiffness in men compared to women [25]. In contrast to AI, aortic stiffness was shown to be higher in female smokers than in male smokers [24, 26], indicating varying stiffness patterns of the vascular system in men and women due to smoking exposure [13]. In the present study, smoking affected arterial stiffness in men more intense than in women, whereas conversely smoking cessation had a more beneficial effect on arterial stiffness in males than in females. Until now, the effect of smoking cessation on arterial stiffness is barely investigated. While most existing studies revealed an improvement of arterial stiffness after quitting smoking [27,28,29] and this positive effect was even seen with nicotine replacement therapy [30], a study from the Netherlands found no decrease in arterial wall thickness and stiffness after two years of smoking cessation [31]. However, this and most of the previous studies only comprised small study samples. In contrast, the present study represents the largest study sample so far, investigating the effect of smoking cessation on arterial stiffness in a sex-specific manner. In the present study, a dose-dependent association between smoking and arterial stiffness was demonstrated and smoking cessation resulted in an improvement in arterial elasticity in both sexes. Scarce prospective data exist on the effect of smoking on arterial stiffness. Tomiyama et al. found a dose-dependent correlation between cigarette smoking and accelerated arterial stiffness in Japanese adults within a five to six years follow-up [32]. These results are in line with our findings. Beyond, in the present study—to our knowledge for the first time—the sex-specific prospective effect of smoking on arterial stiffness was assessed: current and former smoking were associated with higher SI in men but not in women, whereas AI correlated with current smoking but not with former smoking in both sexes.
Arterial stiffness represents a hallmark of aging and is related to premature vascular aging. It is induced by several cardiometabolic disorders like diabetes mellitus and arterial hypertension. By this, several differences in clinical impact between men and women were demonstrated [13]. While the incidence of CVD is relatively low in premenopausal women, the risk to develop CVD increases considerably after menopause [33]. In the literature, increasing evidence demonstrates an independent association between arterial stiffness cardiovascular disease and mortality, whereas this association was almost doubled in women compared to men [7, 8, 13]. In this context, women suffer more often from coronary microvascular dysfunction and heart failure with preserved ejection fraction, both representing conditions which are associated with arterial stiffness and drivers of CVD mortality [13, 34,35,36,37]. Also, sex-specific differences in cognitive function due to arterial stiffening were shown [38] and female sex as well as smoking were identified as independent predictors of human vascular smooth muscle cell stiffening [39]. Regarding specific arterial regions, carotid intima-media thickness was found to be increased in smoking men but not in women [40] and acute exposure to passive smoking influenced the arterial pressure waveform in males but not in females [41]. As one main reason for sex-specific differences in arterial stiffness, sex hormones and vascular receptors are in the focus of research efforts. Especially estrogen was identified to be protective against CVD in premenopausal women baring a lower CVD risk compared to men of the same age. However, postmenopausal women develop CVD approximately ten years later than men, what is widely explained by estrogen loss after menopause [13, 42, 43]. Even an alternating arterial stiffness within the menstrual cycle is discussed in regard to the fluctuating levels of estrogen [13, 44, 45]. The use of hormone-based oral contraception is assumed to promote arterial stiffness and CVD due to interference of sex hormone levels [46]. However, the age- and hormone-mediated impact on arterial stiffness is hard to distinguish since age might outmatch possible hormone effects. Nevertheless, an influence of sex hormones on arterial stiffness cannot be excluded and future investigations are required to elucidate hormone-based effects on vessel arterial elasticity [47].
Pathophysiologically, smoking might promote arterial stiffness by affecting multiple mechanisms such as alteration of the lipid and glucose metabolism, induction of inflammation and oxidative stress or impairment of endothelial function [4, 28]. Lipid metabolism is influenced by smoking due to altered catecholamine release and lipoprotein lipase activity, which lead to elevated triglyceride and low-density lipoprotein blood levels as well as reduction of high-density lipoproteins [48]. By this, atherosclerosis is advanced and hence presumably arterial stiffness [28, 49]. Smoking induces insulin resistance [50] and increases the risk for diabetes mellitus [51]. The risk for developing diabetes mellitus was shown to remain high in heavy smokers even after smoking cessation [52]. Both, insulin resistance and diabetes mellitus cause arterial stiffening [28, 53], which has a considerable clinical impact since arterial stiffness was identified as an independent risk factor for mortality in people with diabetes mellitus [54]. Interestingly, recent investigations likewise revealed vice versa arterial stiffness as a risk factor for the development of diabetes mellitus [55, 56]. One of the main underlying mechanisms of arterial stiffness in a diabetic state is represented by nitric oxide dysregulation [53]. In this context, oxidative stress itself is also caused by smoking [57] and leads to arterial stiffness [58] by the production of reactive oxygen species, which leads to a decrease of nitric oxide by inhibition of nitric oxide synthase [59]. Additionally, smoking causes a decrease in endogenous antioxidant levels with consecutive reduced protection from oxidative stress [60]. A procoagulatory state is provoked by an imbalance of the intraplatelet redox state due to reduced bioactivity of platelet-derived nitric oxide [28, 61] and current smoking does not only influence the arterial vascular system, but also the venous system with increased risk for venous thromboembolism [12]. In the context of impaired synthesis of nitric oxide, also endothelial function has shown to be reduced as a consequence of smoking advancing arterial stiffness [4, 28, 62]. Furthermore, smoking induces inflammation by a mismatch of pro- and anti-inflammatory cytokine expression. Inflammation is strongly associated with arterial stiffness and additionally provokes arterial calcification and remodeling [28, 63,64,65]. Arterial stiffness was shown to be higher in people with arterial hypertension, and the risk for arterial hypertension is elevated by smoking. Furthermore, it has been shown that smoking weakens the stiffness-lowering effect of antihypertensive medication. It is supposed that smoking and arterial hypertension affect arterial stiffness by similar mechanisms, mainly by promoting oxidative stress [4, 28, 66,67,68].
Strengths and limitations
The present study has several limitations, which should be addressed here. Firstly, the overall generalizability of present findings is mostly limited to middle-aged subjects of European ancestry. Furthermore, again due to the study design no detailed examination of smoking behavior within the GHS was possible and a self‐reported assessment of smoking status might be susceptible to information bias. It is known that studies based on self-report are at risk to underestimate smoking status [69], which also cannot be excluded in the GHS. Also, the standard definition of never smoking used in our and other studies can be seen as critical as it defines never-smokers as the group of non-daily and non-regular smokers and thus not truly reflects never smoking.
This study also has several strengths: The GHS is the largest study to date, assessing the sex‐specific relation of smoking status to arterial stiffness and wave reflection. Another strength consists in the simultaneous assessment of two methods of arterial compliance, which are complementary to each other, thereby providing a more comprehensive evaluation of smoking effects on the vasculature. Taken together, the present study compared the influence of arterial stiffness and wave reflection in men and women in a large and highly standardized population-based European cohort. Differences between men and women could be shown, whereas in both sexes smoking had a vast impact on arterial stiffness and wave reflection.
References
Goldenberg M, Danovitch I, IsHak WW (2014) Quality of life and smoking. Am J Addict 23(6):540–562. https://doi.org/10.1111/j.1521-0391.2014.12148.x
World Health Organization. WHO global report on trends in prevalence of tobacco use 2000–2025, third edition. Geneva; 2019. https://www.who.int/publications-detail/who-global-report-on-trends-in-prevalence-of-tobacco-use-2000-2025-third-edition. Accessed 9 Mar 2020
Messner B, Bernhard D (2014) Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol 34(3):509–515. https://doi.org/10.1161/ATVBAHA.113.300156
Munzel T, Hahad O, Kuntic M, Keaney JF, Deanfield JE, Daiber A (2020) Effects of tobacco cigarettes, e-cigarettes, and waterpipe smoking on endothelial function and clinical outcomes. Eur Heart J 41(41):4057–4070. https://doi.org/10.1093/eurheartj/ehaa460
Munzel T, Sinning C, Post F, Warnholtz A, Schulz E (2008) Pathophysiology, diagnosis and prognostic implications of endothelial dysfunction. Ann Med 40(3):180–196. https://doi.org/10.1080/07853890701854702
Daiber A, Steven S, Weber A, Shuvaev VV, Muzykantov VR, Laher I, Li H, Lamas S, Munzel T (2017) Targeting vascular (endothelial) dysfunction. Br J Pharmacol 174(12):1591–1619. https://doi.org/10.1111/bph.13517
Mitchell GF (2009) Arterial stiffness and wave reflection: biomarkers of cardiovascular risk. Artery Res 3(2):56–64. https://doi.org/10.1016/j.artres.2009.02.002
Regnault V, Thomas F, Safar ME, Osborne-Pellegrin M, Khalil RA, Pannier B, Lacolley P (2012) Sex difference in cardiovascular risk: role of pulse pressure amplification. J Am Coll Cardiol 59(20):1771–1777. https://doi.org/10.1016/j.jacc.2012.01.044
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ (2010) Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 121(4):505–511. https://doi.org/10.1161/CIRCULATIONAHA.109.886655
Charakida M, Georgiopoulos G, Dangardt F, Chiesa ST, Hughes AD, Rapala A, Davey Smith G, Lawlor D, Finer N, Deanfield JE (2019) Early vascular damage from smoking and alcohol in teenage years: the ALSPAC study. Eur Heart J 40(4):345–353. https://doi.org/10.1093/eurheartj/ehy524
Munzel T, Hahad O, Daiber A (2019) Double hazard of smoking and alcohol on vascular function in adolescents. Eur Heart J 40(4):354–356. https://doi.org/10.1093/eurheartj/ehy430
Mahmoodi BK, Cushman M, Anne Naess I, Allison MA, Bos WJ, Braekkan SK, Cannegieter SC, Gansevoort RT, Gona PN, Hammerstrom J, Hansen JB, Heckbert S, Holst AG, Lakoski SG, Lutsey PL, Manson JE, Martin LW, Matsushita K, Meijer K, Overvad K, Prescott E, Puurunen M, Rossouw JE, Sang Y, Severinsen MT, Ten Berg J, Folsom AR, Zakai NA (2017) Association of traditional cardiovascular risk factors with venous thromboembolism: an individual participant data meta-analysis of prospective studies. Circulation 135(1):7–16. https://doi.org/10.1161/CIRCULATIONAHA.116.024507
DuPont JJ, Kenney RM, Patel AR, Jaffe IZ (2019) Sex differences in mechanisms of arterial stiffness. Br J Pharmacol 176(21):4208–4225. https://doi.org/10.1111/bph.14624
Wild PS, Zeller T, Beutel M, Blettner M, Dugi KA, Lackner KJ, Pfeiffer N, Munzel T, Blankenberg S (2012) The Gutenberg health study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 55(6–7):824–829. https://doi.org/10.1007/s00103-012-1502-7
Panova-Noeva M, Arnold N, Hermanns MI, Prochaska JH, Schulz A, Spronk HM, Binder H, Pfeiffer N, Beutel M, Blankenberg S, Zeller T, Lotz J, Munzel T, Lackner KJ, Ten Cate H, Wild PS (2017) Mean platelet volume and arterial stiffness—clinical relationship and common genetic variability. Sci Rep 7:40229. https://doi.org/10.1038/srep40229
Arnold N, Deiseroth A, Hahad O, Diestelmeier S, Schulz A, Daubenbuchel A, Gori T, Binder H, Pfeiffer N, Prochaska J, Beutel M, Lackner KJ, Munzel T, Wild PS (2021) Domains of physical activity in relation to stiffness index in the general population. J Am Heart Assoc 10(16):e020930. https://doi.org/10.1161/JAHA.121.020930
World Health Organization. Collaborating Centre for Drug Statistics Methodology. https://www.whocc.no/atc/structure_and_principles/. Accessed 5 Mar 2020
Lampert T, Kroll LE, Muters S, Stolzenberg H (2013) Measurement of the socioeconomic status within the German Health Update 2009 (GEDA). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 56(1):131–143. https://doi.org/10.1007/s00103-012-1583-3
Burger M, Mensink G (2003) Bundesgesundheitssurvey: Alkohol—Konsumverhalten in Deutschland. Robert Koch-Institut (RKI), Berlin
Lowe B, Grafe K, Zipfel S, Witte S, Loerch B, Herzog W (2004) Diagnosing ICD-10 depressive episodes: superior criterion validity of the Patient Health Questionnaire. Psychother Psychosom 73(6):386–390. https://doi.org/10.1159/000080393
Campbell N, Gaston A, Gray C, Rush E, Maddison R, Prapavessis H (2016) The Short Questionnaire to Assess Health-Enhancing (SQUASH) physical activity in adolescents: a validation using doubly labeled water. J Phys Act Health 13(2):154–158. https://doi.org/10.1123/jpah.2015-0031
Collaborators GBDT (2017) Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet 389(10082):1885–1906. https://doi.org/10.1016/S0140-6736(17)30819-X
Higgins ST, Kurti AN, Redner R, White TJ, Gaalema DE, Roberts ME, Doogan NJ, Tidey JW, Miller ME, Stanton CA, Henningfield JE, Atwood GS (2015) A literature review on prevalence of gender differences and intersections with other vulnerabilities to tobacco use in the United States, 2004–2014. Prev Med 80:89–100. https://doi.org/10.1016/j.ypmed.2015.06.009
Mozos I, Maidana JP, Stoian D, Stehlik M (2017) Gender differences of arterial stiffness and arterial age in smokers. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph14060565
Tomiyama H, Yamazaki M, Sagawa Y, Teraoka K, Shirota T, Miyawaki Y, Yamashina A (2009) Synergistic effect of smoking and blood pressure on augmentation index in men, but not in women. Hypertension Res 32(2):122–126. https://doi.org/10.1038/hr.2008.20
Sonesson B, Ahlgren AR, Lazer L, Lanne T (1997) Does long-term smoking affect aortic stiffness more in women than in men? Clin Physiol 17(5):439–447. https://doi.org/10.1046/j.1365-2281.1997.04848.x
Saz-Lara A, Martinez-Vizcaino V, Sequi-Dominguez I, Alvarez-Bueno C, Notario-Pacheco B, Cavero-Redondo I (2021) The effect of smoking and smoking cessation on arterial stiffness: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. https://doi.org/10.1093/eurjcn/zvab102
Doonan RJ, Hausvater A, Scallan C, Mikhailidis DP, Pilote L, Daskalopoulou SS (2010) The effect of smoking on arterial stiffness. Hypertension Res 33(5):398–410. https://doi.org/10.1038/hr.2010.25
Lee GB, Shim JS, Kim HC (2020) Dose-response association between smoking cessation and arterial stiffness: the Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) Cohort. Korean Circ J 50(4):361–369. https://doi.org/10.4070/kcj.2019.0270
Xue C, Chen QZ, Bian L, Yin ZF, Xu ZJ, Zhang AL, Xie YS, Zhang HL, Du R, Wang CQ (2019) Effects of smoking cessation with nicotine replacement therapy on vascular endothelial function, arterial stiffness, and inflammation response in healthy smokers. Angiology 70(8):719–725. https://doi.org/10.1177/0003319719853458
van den Berkmortel FW, Wollersheim H, van Langen H, Smilde TJ, den Arend J, Thien T (2004) Two years of smoking cessation does not reduce arterial wall thickness and stiffness. Neth J Med 62(7):235–241
Tomiyama H, Hashimoto H, Tanaka H, Matsumoto C, Odaira M, Yamada J, Yoshida M, Shiina K, Nagata M, Yamashina A (2010) Continuous smoking and progression of arterial stiffening: a prospective study. J Am Coll Cardiol 55(18):1979–1987. https://doi.org/10.1016/j.jacc.2009.12.042
Coutinho T (2014) Arterial stiffness and its clinical implications in women. Can J Cardiol 30(7):756–764. https://doi.org/10.1016/j.cjca.2014.03.020
Beale AL, Meyer P, Marwick TH, Lam CSP, Kaye DM (2018) Sex differences in cardiovascular pathophysiology: why women are overrepresented in heart failure with preserved ejection fraction. Circulation 138(2):198–205. https://doi.org/10.1161/CIRCULATIONAHA.118.034271
Coutinho T, Yam Y, Chow BJW, Dwivedi G, Inacio J (2017) Sex differences in associations of arterial compliance with coronary artery plaque and calcification burden. J Am Heart Assoc. https://doi.org/10.1161/JAHA.117.006079
Gdowski MA, Murthy VL, Doering M, Monroy-Gonzalez AG, Slart R, Brown DL (2020) Association of isolated coronary microvascular dysfunction with mortality and major adverse cardiac events: a systematic review and meta-analysis of aggregate data. J Am Heart Assoc 9(9):e014954. https://doi.org/10.1161/JAHA.119.014954
Schocken DD, Arrieta MI, Leaverton PE, Ross EA (1992) Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 20(2):301–306. https://doi.org/10.1016/0735-1097(92)90094-4
Sabra D, Intzandt B, Desjardins-Crepeau L, Langeard A, Steele CJ, Frouin F, Hoge RD, Bherer L, Gauthier CJ (2021) Sex moderations in the relationship between aortic stiffness, cognition, and cerebrovascular reactivity in healthy older adults. PLoS ONE 16(9):e0257815. https://doi.org/10.1371/journal.pone.0257815
Dinardo CL, Santos HC, Vaquero AR, Martelini AR, Dallan LA, Alencar AM, Krieger JE, Pereira AC (2015) Smoking and female sex: independent predictors of human vascular smooth muscle cells stiffening. PLoS ONE 10(12):e0145062. https://doi.org/10.1371/journal.pone.0145062
Gariepy J, Denarie N, Chironi G, Salomon J, Levenson J, Simon A (2000) Gender difference in the influence of smoking on arterial wall thickness. Atherosclerosis 153(1):139–145. https://doi.org/10.1016/s0021-9150(00)00382-8
Mahmud A, Feely J (2004) Effects of passive smoking on blood pressure and aortic pressure waveform in healthy young adults–influence of gender. Br J Clin Pharmacol 57(1):37–43. https://doi.org/10.1046/j.1365-2125.2003.01958.x
Mendelsohn ME, Karas RH (1999) The protective effects of estrogen on the cardiovascular system. N Engl J Med 340(23):1801–1811. https://doi.org/10.1056/NEJM199906103402306
Mendelsohn ME, Karas RH (2005) Molecular and cellular basis of cardiovascular gender differences. Science 308(5728):1583–1587. https://doi.org/10.1126/science.1112062
Robb AO, Mills NL, Din JN, Smith IB, Paterson F, Newby DE, Denison FC (2009) Influence of the menstrual cycle, pregnancy, and preeclampsia on arterial stiffness. Hypertension 53(6):952–958. https://doi.org/10.1161/HYPERTENSIONAHA.109.130898
Adkisson EJ, Casey DP, Beck DT, Gurovich AN, Martin JS, Braith RW (2010) Central, peripheral and resistance arterial reactivity: fluctuates during the phases of the menstrual cycle. Exp Biol Med 235(1):111–118. https://doi.org/10.1258/ebm.2009.009186
Seeland U, Demuth I, Regitz-Zagrosek V, Steinhagen-Thiessen E, Konig M (2020) Sex differences in arterial wave reflection and the role of exogenous and endogenous sex hormones: results of the Berlin Aging Study II. J Hypertens 38(6):1040–1046. https://doi.org/10.1097/HJH.0000000000002386
Laakkonen EK, Karppinen JE, Lehti S, Lee E, Pesonen E, Juppi HK, Kujala UM, Haapala EA, Aukee P, Laukkanen JA, Ihalainen JK (2021) Associations of sex hormones and hormonal status with arterial stiffness in a female sample from reproductive years to menopause. Front Endocrinol 12:765916. https://doi.org/10.3389/fendo.2021.765916
Chelland Campbell S, Moffatt RJ, Stamford BA (2008) Smoking and smoking cessation—the relationship between cardiovascular disease and lipoprotein metabolism: a review. Atherosclerosis 201(2):225–235. https://doi.org/10.1016/j.atherosclerosis.2008.04.046
Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX (1997) Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol 146(6):483–494. https://doi.org/10.1093/oxfordjournals.aje.a009302
Seet RC, Loke WM, Khoo CM, Chew SE, Chong WL, Quek AM, Lim EC, Halliwell B (2012) Acute effects of cigarette smoking on insulin resistance and arterial stiffness in young adults. Atherosclerosis 224(1):195–200. https://doi.org/10.1016/j.atherosclerosis.2012.06.060
Chang SA (2012) Smoking and type 2 diabetes mellitus. Diabetes Metab J 36(6):399–403. https://doi.org/10.4093/dmj.2012.36.6.399
Park SE, Seo MH, Cho JH, Kwon H, Kim YH, Han KD, Jung JH, Park YG, Rhee EJ, Lee WY (2021) Dose-dependent effect of smoking on risk of diabetes remains after smoking cessation: a nationwide population-based cohort study in Korea. Diabetes Metab J 45(4):539–546. https://doi.org/10.4093/dmj.2020.0061
Prenner SB, Chirinos JA (2015) Arterial stiffness in diabetes mellitus. Atherosclerosis 238(2):370–379. https://doi.org/10.1016/j.atherosclerosis.2014.12.023
Kim JM, Kim SS, Kim IJ, Kim JH, Kim BH, Kim MK, Lee SH, Lee CW, Kim MC, Ahn JH, Kim J, Relationship between Cardiovascular d, Brachial-ankle Pulse Wave Velocity in Patients with Type 2 Diabetes Study G (2020) Arterial stiffness is an independent predictor for risk of mortality in patients with type 2 diabetes mellitus: the REBOUND study. Cardiovasc Diabetol 19(1):143. https://doi.org/10.1186/s12933-020-01120-6
Zheng M, Zhang X, Chen S, Song Y, Zhao Q, Gao X, Wu S (2020) Arterial stiffness preceding diabetes: a longitudinal study. Circ Res 127(12):1491–1498. https://doi.org/10.1161/CIRCRESAHA.120.317950
Hahad O, Wild PS, Prochaska JH, Schulz A, Hermanns I, Lackner KJ, Pfeiffer N, Schmidtmann I, Beutel M, Gori T, Deanfield JE, Munzel T (2019) Endothelial function assessed by digital volume plethysmography predicts the development and progression of type 2 diabetes mellitus. J Am Heart Assoc 8(20):e012509. https://doi.org/10.1161/JAHA.119.012509
Kuntic M, Oelze M, Steven S, Kroller-Schon S, Stamm P, Kalinovic S, Frenis K, Vujacic-Mirski K, Bayo Jimenez MT, Kvandova M, Filippou K, Al Zuabi A, Bruckl V, Hahad O, Daub S, Varveri F, Gori T, Huesmann R, Hoffmann T, Schmidt FP, Keaney JF, Daiber A, Munzel T (2020) Short-term e-cigarette vapour exposure causes vascular oxidative stress and dysfunction: evidence for a close connection to brain damage and a key role of the phagocytic NADPH oxidase (NOX-2). Eur Heart J 41(26):2472–2483. https://doi.org/10.1093/eurheartj/ehz772
Rahman MM, Laher I (2007) Structural and functional alteration of blood vessels caused by cigarette smoking: an overview of molecular mechanisms. Curr Vasc Pharmacol 5(4):276–292. https://doi.org/10.2174/157016107782023406
Peluffo G, Calcerrada P, Piacenza L, Pizzano N, Radi R (2009) Superoxide-mediated inactivation of nitric oxide and peroxynitrite formation by tobacco smoke in vascular endothelium: studies in cultured cells and smokers. Am J Physiol Heart Circ Physiol 296(6):H1781-1792. https://doi.org/10.1152/ajpheart.00930.2008
Barnoya J, Glantz SA (2005) Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation 111(20):2684–2698. https://doi.org/10.1161/CIRCULATIONAHA.104.492215
Takajo Y, Ikeda H, Haramaki N, Murohara T, Imaizumi T (2001) Augmented oxidative stress of platelets in chronic smokers. Mechanisms of impaired platelet-derived nitric oxide bioactivity and augmented platelet aggregability. J Am Coll Cardiol 38(5):1320–1327. https://doi.org/10.1016/s0735-1097(01)01583-2
Hahad O, Arnold N, Prochaska JH, Panova-Noeva M, Schulz A, Lackner KJ, Pfeiffer N, Schmidtmann I, Michal M, Beutel M, Wild PS, Keaney JF Jr, Daiber A, Munzel T (2021) Cigarette smoking is related to endothelial dysfunction of resistance, but not conduit arteries in the general population-results from the gutenberg health study. Front Cardiovasc Med 8:674622. https://doi.org/10.3389/fcvm.2021.674622
Arnson Y, Shoenfeld Y, Amital H (2010) Effects of tobacco smoke on immunity, inflammation and autoimmunity. J Autoimmun 34(3):J258-265. https://doi.org/10.1016/j.jaut.2009.12.003
Kals J, Kampus P, Kals M, Pulges A, Teesalu R, Zilmer K, Kullisaar T, Salum T, Eha J, Zilmer M (2008) Inflammation and oxidative stress are associated differently with endothelial function and arterial stiffness in healthy subjects and in patients with atherosclerosis. Scand J Clin Lab Invest 68(7):594–601. https://doi.org/10.1080/00365510801930626
Boutouyrie P, Laurent S, Briet M (2008) Importance of arterial stiffness as cardiovascular risk factor for future development of new type of drugs. Fundam Clin Pharmacol 22(3):241–246. https://doi.org/10.1111/j.1472-8206.2008.00584.x
Minami J, Ishimitsu T, Ohrui M, Matsuoka H (2009) Association of smoking with aortic wave reflection and central systolic pressure and metabolic syndrome in normotensive Japanese men. Am J Hypertens 22(6):617–623. https://doi.org/10.1038/ajh.2009.62
Pardell H, Rodicio JL (2005) High blood pressure, smoking and cardiovascular risk. J Hypertens 23(1):219–221. https://doi.org/10.1097/00004872-200501000-00037
McEniery CM, Wilkinson IB, Avolio AP (2007) Age, hypertension and arterial function. Clin Exp Pharmacol Physiol 34(7):665–671. https://doi.org/10.1111/j.1440-1681.2007.04657.x
Connor Gorber S, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M (2009) The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tobacco Res 11(1):12–24. https://doi.org/10.1093/ntr/ntn010
Acknowledgements
The Gutenberg Health Study is funded through the government of Rhineland-Palatinate (“Stiftung Rheinland-Pfalz für Innovation”, contract AZ 961-386261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg-University of Mainz, and its contract with Boehringer Ingelheim and PHILIPS Medical Systems, including an unrestricted grant for the Gutenberg Health Study and by the Foundation Heart of Mainz. T.M. and P.S.W. are PI`s of the German Center for Cardiovascular Research (DZHK), partner site Rhine-Main, Mainz, Germany. J.H.P. and P.S.W. are funded by the Federal Ministry of Education and Research (BMBF 01EO1503). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The author declares that they have no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hahad, O., Schmitt, V.H., Arnold, N. et al. Chronic cigarette smoking is associated with increased arterial stiffness in men and women: evidence from a large population-based cohort. Clin Res Cardiol 112, 270–284 (2023). https://doi.org/10.1007/s00392-022-02092-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-022-02092-1