Abstract
Background
The joint contribution of genetic and environmental exposures to noncommunicable diseases is not well characterized.
Objectives
We modeled the cumulative effects of common risk alleles and their prevalence variations with classical risk factors.
Methods
We analyzed mathematically and statistically numbers and effect sizes of established risk alleles for coronary artery disease (CAD) and other conditions.
Results
In UK Biobank, risk alleles counts in the lowest (175.4) and highest decile (205.7) of the distribution differed by only 16.9%, which nevertheless increased CAD prevalence 3.4-fold (p < 0.01). Irrespective of the affected gene, a single risk allele multiplied the effects of all others carried by a person, resulting in a 2.9-fold stronger effect size in the top versus the bottom decile (p < 0.01) and an exponential increase in risk (R > 0.94). Classical risk factors shifted effect sizes to the steep upslope of the logarithmic function linking risk allele numbers with CAD prevalence. Similar phenomena were observed in the Estonian Biobank and for risk alleles affecting diabetes mellitus, breast and prostate cancer.
Conclusions
Alleles predisposing to common diseases can be carried safely in large numbers, but few additional ones lead to sharp risk increments. Here, we describe exponential functions by which risk alleles combine interchangeably but multiplicatively with each other and with modifiable risk factors to affect prevalence. Our data suggest that the biological systems underlying these diseases are modulated by hundreds of genes but become only fragile when a narrow window of total risk, irrespective of its genetic or environmental origins, has been passed.
Graphical Abstract

Similar content being viewed by others
Introduction
Most common noncommunicable diseases share a multifactorial etiology, with both exogenous and inherited factors contributing to their manifestation. In recent years, genome-wide association studies (GWAS) have substantially increased our understanding of the genetic component of disease risk. Specifically, hundreds of loci have been identified that all modulate risk of diseases such as coronary artery disease (CAD), breast cancer, prostate cancer, and type 2 diabetes mellitus (T2DM) as well as many other common diseases [1,2,3,4]. These findings have not only enriched the exploration of disease mechanisms but also raised the hope of improving risk prediction by assessment of the individual burden of risk alleles in form of genetic risk scores (GRS) [5,6,7]. However, from a clinical perspective, the conclusions from recent studies on this matter have appeared contradictory. Some found only small incremental benefits using GRS for risk prediction in the overall population whereas others identified individuals in whom a high GRS mirrored the risk of damaging mutations found in monogenic conditions [7,8,9,10,11].
Importantly, risk-conferring alleles are found with a high frequency in a given population. For example, three out of four Western-European ancestry individuals carry at least one risk allele at the 9p21 locus, which increases the odds of CAD by 1.23 [12]. Given the many genome-wide significant loci that have been identified in recent years [13], the total number of risk alleles carried by each person is likely to be very high. It is thus of critical importance to understand how these risk alleles interact. In the absence of empirical data, this interaction has been predicted by mathematical models, in which risk allele counts weighted by their estimated effect size from a GWAS are being combined. Examples are the logarithm of odds (Log) model or the Probit link function. Such widely used models predict the cumulative effects of risk alleles in a logistic function suggesting a sigmoidal relationship between GRS and probability of disease. Here, we conduct a systematic empirical evaluation of linear and multiplicative models to more precisely define risk conferred by common risk alleles [14,15,16,17].
From a clinical point of view, it is even more important—and not well defined yet—In other words, is the cumulative burden of common risk alleles tolerably low putting the population at the flat part of the curve—or beyond a turning point, where a few further multipliers (risk alleles) may cause a steep increase in disease prevalence?
Finally, factors such as smoking, T2DM, or obesity all increase prevalence of CAD and other common diseases. To better understand the principle mechanisms underlying the combinatorial effects of these and other risk factors with the genetic components, we simplified our analysis in that we focused on the bare number of highly significant risk alleles, albeit a genetic score built on millions of variants might be more precise in giving weight to the genetic risk conferred by each percentile of a GRS [7, 18].
Methods
Study participants
The UK Biobank project (UKB; http://www.ukbiobank.ac.uk) is a large prospective cohort study of ~ 500,000 individuals from across the United Kingdom, aged 40–69 years (56.4 ± 8.0) at the recruitment visit between 2006 and 2010 [19]. The flowchart of our analysis is shown in Supplementary Figure S1A. Following informed consent, health-related information was collected for each participant. In addition to self-reported information, dietary and exercise habits, multiple physical, cognitive and biochemical measurements were obtained. After quality control, we included 465,910 European individuals (Supplementary Figure S1B). CAD was defined as fatal or non-fatal myocardial infarction, percutaneous coronary intervention or coronary artery bypass grafting. ICD codes used for definition are listed in Supplementary Table S1. Breast cancer was defined by the primary and secondary ICD-10 diagnosis codes of “C50 Malignant neoplasm of the mammary gland”. Prostate cancer was defined by the primary and secondary ICD-10 diagnosis codes of “C61 Malignant neoplasm of the prostate”.
Since the diabetes GWAS, which led to identification of most of the genome-wide significant SNPs, included the summary statistics of UK biobank data, we used an independent source—Estonian biobank—for analysis of diabetes. The Estonian Biobank is a population-based cohort of the Estonian Genome Center at the Institute of Genomics of the University of Tartu [20]. Quality control details are found in the Supplementary Methods. We used 90,976 individuals for studying CAD and 91,195 individuals for studying T2DM. T2DM was defined by respective ICD-10 codes “E11 Type 2 Diabetes mellitus”.
None of the study participants was included in the GWAS that led to the identification of the risk alleles. All disease cases were considered for this study either being prevalent at recruitment in UKB or in the Estonian Biobank (fatal and non-fatal) or being registered during follow-up of the cohorts.
Selection of risk variants
CAD, breast cancer, prostate cancer and T2DM were selected to represent common diseases each being affected by risk alleles at more than 100 autosomal loci discovered by GWAS meta-analyses [2, 3, 21]. GWAS summary statistics used for calculation are listed in Supplementary Tables S2–S5 and Figure S1C. Moreover, we calculated the genome-wide polygenic risk score using 6.6 million CAD SNPs [7].
Genetic risk score and subgroups risk calculation
Individuals were grouped simply by the number of risk alleles to obtain their frequency distribution in the population in form of deciles, without giving weight to their respective effect sizes. The lowest decile was used as a reference. Missing genotypes were replaced by the expected value, which is twice the risk allele frequency. As a sensitivity analysis, we also constituted deciles of a weighted genetic risk score (wGRS), which was calculated based on risk variants by summing up the number of risk alleles weighted by the corresponding log odds ratio for the risk allele. All data on the wGRS are shown in the supplement. The analyses investigating the exchangeability of risk allele profiles are described in detail in the Supplementary Methods and Figure S2. The non-lipid CAD SNPs and lipid CAD SNPs were listed in Supplementary Table S6 [1].
Stratification by modifiable risk factors
CAD prevalence was determined in each decile separated for exposure to smoking (ever versus never smokers), obesity (BMI ≥ 30 kg/m2), T2DM, or sedentary lifestyle (< 7.5 MET-h), detailed in the Supplementary Methods. Prediabetes was also classified as diabetes mellitus in this study, if participants indicated by questionnaire to have diabetes. Breast cancer prevalence was determined in each decile separated by obesity and alcohol intake for postmenopausal women. Finally, prostate cancer prevalence was quantified for men with and without a positive family history for prostate cancer and T2DM prevalence was quantified for people with and without obesity.
Analysis of data and statistical methods
We assessed the goodness-of-fit of different statistical models of the relationships between risk allele frequency (x-axis) and prevalence/prevalence per allele (y-axis). We tested the prevalence contribution of risk alleles in extreme groups by estimating the correlation (R) of four competing models: Linear, Log, Probit, and Logistic. Respective plots display prevalence (on the left) and prevalence mediated per single risk allele (on the right) in groups with sample sizes larger than 200 subjects (e.g., Figure 2A, B). Scripts are found in the Supplementary Methods.
Mean values were calculated as arithmetic averages and represented as mean ± standard error. A p value of < 0.05 was considered statistically significant. Trends across deciles were tested by linear regression.
We used R [22] (version 4.0.3) and statistic packages of tidyverse, data.table, varhandle and ggplot2 for statistical calculations. All further details for the methods part could be found in Supplementary Methods.
Results
Risk of CAD in relation to risk allele distribution in UKB
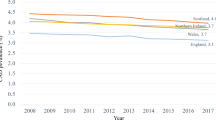
In UKB, 427,360 subjects had phenotypic data regarding CAD, among whom we identified 20,310 cases. All risk alleles studied here were located on the diploid set of autosomal chromosomes such that the theoretical number of risk alleles at the 198 CAD risk loci we studied is between 0 and 396. Given the high frequency of the common risk alleles in the Western population we observed that a person carried an average of 190 CAD risk alleles. The mean number of CAD risk alleles per person was normally distributed (Fig. 1A) and varied between 175.4 and 205.2 in the bottom and top decile of the distribution, corresponding to a CAD prevalence of 2.4 and 8.2 percent, respectively (Table 1). When compared to the first decile, individuals in the tenth decile thus carried on average 29.8 or 16.9 percent more risk alleles whereas disease was 3.4-fold more prevalent (Table 1). An even wider spread in CAD prevalence was observed between the 1st (2.0 percent) and 99th (11.2 percent) percentile of the risk allele frequency distribution, which differed by 39.7 risk alleles (Supplementary Table S7). We used EstBB as an independent validation dataset and the results for CAD were similar to that in UKB (Supplementary Table S7, Table S8).
Histograms showing the distribution of risk alleles counts, which were normally distributed by Kolmogorov–Smirnov test (p values < 0.05), for coronary artery disease (CAD), breast cancer, prostate cancer, and type 2 diabetes mellitus (T2DM) in cases and controls separately. The number of common risk alleles per person were grouped in bins width of 2 risk alleles per person for respective diseases. Each person carried more than one hundred respective risk alleles with, on average, cases carrying 3–4 more than controls. Average numbers are shown for controls in green and for cases in blue boxes
Generalizability to other common diseases
Studying 218,781 women and 205,624 men in UKB, we next determined all cases of validated breast (n = 13,221) and prostate cancer (n = 7832). For both diseases, the 134 published [2, 3] genome-wide significant risk variants were normally distributed (Fig. 1B, C). In the lowest decile of the frequency distribution, the prevalence of breast cancer and prostate cancer were 3.3 percent and 1.6 percent, respectively, with average numbers of risk alleles in these groups being 121.6 (breast cancer) and 110.4 (prostate cancer) (Table 1). Individuals in the top decile carried on average between 20.2 (breast cancer) and 22.4 percent (prostate cancer) more risk alleles whereas the disease prevalence went up by 3.1- and 5.1-fold, respectively (Table 1). In the lowest percentile of the risk allele frequency distribution, a low prevalence of breast cancer (2.3 percent) and prostate cancer (1.0 percent) contrasted with 14.0 and 11.2 percent in the 99th top percentile (Supplementary Table S7).
We carried out the same analyses for T2DM in the Estonian Biobank (301 genome-wide significant risk variants, 91,195 individuals, Fig. 1D). In the lowest decile of the frequency distribution, the prevalence of T2DM was 3.2 percent with the average number of risk alleles per person being 250.9 (Table 1). Individuals in the top decile carried on average 34.2 more risk alleles whereas the disease prevalence went up to 9.3 percent (Table 1). In the 1st percentile of the risk allele frequency distribution, the prevalence of T2DM at 2.1 percent contrasted with 10.4 percent in the 99th percentile (Supplementary Table S7). Respective data for the wGRS are shown in Supplementary Table S8 and Supplementary Figure S3.
Per risk allele prevalence
We next grouped subjects carrying the same number of risk alleles for a disease and determined the respective disease prevalence in these groups. Consistently across all diseases tested, we observed a sharp increase in prevalence with a relatively small increase in the number of risk alleles (Fig. 2A, Supplementary Figure S4). To investigate prevalence instigated per single risk allele we also display prevalence divided by the number of respective risk alleles carried in a person (Fig. 2B, Supplementary Figure S4). Remarkably, any given risk allele in the tenth decile of the risk allele distribution conveyed 2.9-, 2.6-, 4.2-, and 2.5-fold stronger effects on CAD, breast cancer, prostate cancer, and T2DM manifestation, respectively, than the same allele in the first decile (all p ≤ 0.01). since these were similar across deciles (Supplementary Table S8). In Fig. 2, the area shaded in grey represents the majority of subjects in the population, i.e., the second to ninth decile. Respective figures for breast cancer, prostate cancer, T2DM and the respective data on wGRS are shown in Supplementary Figures S5. Figures for independent validation on EstBB for CAD using both numbers of risk alleles and wGRS are shown in Supplementary Figure S4 and S5.
A Disease prevalence in relation to the number of risk alleles. The Y-axis displays the prevalence of coronary artery disease (CAD) in the UKB population. The X-axis displays the cumulative number of risk alleles per person. The correlation (R) between observed and predicted prevalence is given for each of four fitted functions, with its 95% confidence interval. B We divided the prevalence of each disease by the number of risk alleles per person, showing the effect of a single risk allele depending on a person’s overall burden of risk variants. The parts of the population residing between the 2nd and 9th decile of allele count distribution are highlighted in grey. The green and red lines show the fit from the logit and logarithmic functions, respectively
Empirical evaluation of regression models
To better understand how risk alleles interact in mathematical terms, we modeled the relationship between disease prevalence and risk allele counts. Using generalized linear (GLM) regression models, which require specifying a link function, we compared the goodness-of-fit of using a Linear, Logistic (Logit), Probit, and Log link function. The goodness-of-fit of each of these four models was assessed using the correlation between the observed prevalence and the predicted prevalence from the corresponding model (Fig. 2 and Supplementary Figures S4). Consistently, we found that our data best fit non-linear link functions (i.e., Logit, Probit or Log), of which none consistently outperformed the others across different diseases. This finding, likewise, was replicated when we used 6.6 million SNPs [7] to calculate the CAD wGRS in UKB. Expectedly, the discrimination of risk is slightly better, but the principle functions remained to be highly similar to those seen with the 198 top-ranked SNPs. (Supplementary Figure S5K, Supplementary Table S8).
Relevance of risk allele function
The prevalence of traditional risk factors and use of lipid-lowering medication was only marginally different across the deciles of the GRS (Supplementary Table S9a). Exclusion of variants previously shown to affect lipid levels (n = 28) or blood pressure (n = 14) had no influence on the exponential appearance of the regression curves for increasing numbers of risk allele and CAD prevalence (Supplementary Figure S6, A, B, E, F and Supplementary Table S9, Supplementary Figure S6, C, D, G, H). Likewise, in 10,000 random sets of 99 CAD-associated SNPs (out of the 198 CAD risk variants), we observed highly similar regression curves for CAD prevalence (Supplementary Figure S6, A, B, C, D) with Logit- and Log-based models showing regression coefficients (R) of 0.96 on average, with little variability (Supplementary Figure S6 E, F). These data suggest that the cumulative number of risk alleles rather than specific combinations of risk alleles is the major determinant of genetic risk.
We next restricted the regression analysis to the 28 risk alleles known to affect lipid levels and compared their effects with 28 SNPs, which have similar published odds ratios for CAD but no effects on lipids (Supplementary Table S6). As shown in Fig. 3, the increase in CAD prevalence was similar across the ten deciles of the two groups of risk alleles. When we subdivided individuals within the tenth deciles of the two groups of risk alleles in those who carry low (first decile), medium (second to ninth deciles), or high (tenth decile) numbers of the risk alleles from the other respective group, the effects on disease prevalence remained comparable.
A Prevalence of coronary artery disease in relation to 28 risk alleles affecting lipid levels (red dots) and 28 risk alleles with equal odds ratios but no effects on lipids (blue dots). In the first decile individuals carried on average 18.9 ± 1.3 lipid-related risk alleles and 17.8 ± 1.3 non-lipid-related risk alleles. The respective numbers for the tenth decile were 30.9 ± 1.3 and 28.9 ± 1.3. B CAD prevalence is shown in subgroups of the tenth deciles of lipid and non-lipid SNPs. We subdivided subjects in the tenth decile of lipid-related SNPs in a high, medium, and low number non-lipid-related SNP subgroup. Vice versa, we subdivided the tenth decile of non-lipid-related SNPs according to high, medium and low numbers of lipid-associated variants. Top*, middle*, low* refers to the 10th decile, 2nd to 9th deciles and 1st decile. The effects of lipid-related and non-lipid-related risk alleles are interchangeable with respect to the prevalence of CAD
Environmental risk factors and disease prevalence
We next studied the impact of established risk factors for CAD in UKB; Fig. 4A–D shows data on diabetes as an example. As compared to the first decile of the risk allele distribution, in the tenth decile, we observed that the absolute increases in prevalence related to diabetes, smoking, obesity, sedentary lifestyle, male sex, age ≥ 55 years, average total household income before tax below 18,000, being without cholesterol medication, being without blood pressure medication, and high cholesterol level (> 6.18 mmol/L) were 2.7, 3.0, 3.0, 3.8, 3.4, 2.9, 1.0, 5.4, 2.8, and 1.4-fold higher, respectively (all p < 0.01 for first vs the tenth decile; Fig. 4B and Supplementary Figure S7). In other words, a high genetic risk amplified the absolute prevalence conveyed by the respective risk factor.
Prevalence of CAD in risk allele deciles with and without diabetes (other risk factors are shown in Supplementary Figure S7). A shows the prevalence for CAD in individuals with and without diabetes in UKB. B shows CAD prevalence in low (1st), medium (2nd–9th) and high (10th) deciles of risk allele distribution in the UKB without and with diabetes. The grey bars represent the difference in prevalence related to diabetes in the three genetic subgroups. As can be seen, the effect of diabetes is much larger in subjects with a high burden of risk alleles. C shows disease prevalence across the deciles of risk alleles in subjects with (red line) and without diabetes (blue line). The correlation (R) between observed and predicted prevalence is given for fitted logit functions with their 95% confidence interval. D shows disease prevalence across the deciles of risk alleles in subjects with (red line) and without diabetes (blue line) as a deviation from the average in the respective group. In the diabetes group the increase in risk with increasing numbers of risk alleles is by far steeper (linear regression coefficient: diabetes 0.0058, no diabetes 0.0019). E displays the difference in prevalence between subjects with diabetes and without diabetes across increasing deciles of risk alleles indicating that increasing risk alleles numbers enhance the effect of diabetes. In D and E, the correlation (R) between observed and predicted prevalence is given for a quadratic function, with its 95% confidence interval
Figure 4C shows a much more pronounced change in CAD risk for diabetes as compared to non-diabetic individuals across the deciles of the risk allele distribution, in relation to the average risk in the respective group. Importantly, in subjects exposed to a risk factor, we observed a by far steeper increase in absolute disease risk with increasing numbers of risk alleles than individuals without the respective risk factor (panel D and E in Fig. 4 and Supplementary Figure S7). Respective data for the wGRS—either with 198 significant SNPs or 6.6 million SNPs—are consistent and also shown in the supplement (Supplementary Figure S8 and Supplementary Table S10).
Similar data were observed for established risk factors for breast cancer (obesity, alcohol consumption), prostate cancer (positive family history), and T2DM (obesity). The absolute increases in prevalence were 7.6- (obesity-breast cancer), 8.1- (positive family history-prostate cancer) and 1.8-fold higher (obesity-T2DM) in the tenth as compared to the first decile of respective risk allele distribution and the effect of alcohol intake on breast cancer risk was only apparent in women with at least moderate genetic susceptibility (all p < 0.01).
Discussion
By studying how established risk alleles affect the prevalence of common diseases, we report two important findings. First, we observed that respective risk alleles lead to a steep increase in risk for CAD, breast cancer, prostate cancer, or type 2 diabetes mellitus despite only small changes in their overall numbers. Second, all individual risk factors—genetic and environmental—act multiplicatively and interchangeably, and cause disease once a crucial turning point of cumulative risk is being passed. Essentially, irrespective of which biological pathways are being affected by disease loci or the combination of risk alleles with environmental exposures, the only quantity that matters is the total burden of these factors which put a person on a logarithmic curve of increasing risk.
Our findings have implications for the application of polygenic risk scores in predicting risk as well as for the understanding of biological mechanisms leading to the manifestation of the respective diseases. Regarding the first and clinically relevant topic: consistent with the genetic sampling theory, the largely random allocation of chromosomal segments during meiosis results in a normal distribution of common risk alleles. While the range of this distribution increases when more loci are detected to be associated with a trait, it is remarkable to observe overall relatively little variation in the high numbers of risk alleles across a population. This may explain why the predictive value of polygenic risk scores has been considered to be low [8,9,10]. However, looking at the first and tenth decile of the population, we observe an increase of disease prevalence by up to 5.1-fold. Thus, the predictive value of polygenic risk scores seems to be clinically relevant mostly for those at the outer ends of the distribution curve. In fact, given the apparent exponential increase in risk, those who carry high numbers of common risk alleles may have risks comparable to people carrying damaging mutations otherwise found in monogenic conditions [7].
Our observations are best explained by a simple multiplicative model, whereby the effect of each risk allele is proportional to the cumulative burden of all other risk alleles carried in a person. The resulting non-linear function has long been postulated to account for the risk of recurrence of common diseases mediated by multiple genetic risk factors in relatives [23,24,25,26]. Similarly, empirical data on multiple environmental risk factors are consistent with a non-linear relationship between the number of risk factors and prevalence [14]. Consistent with these observations, the standard model to analyze case–control GWAS data is a logistic regression, and genetic risk scores are constructed accordingly [14, 27]. The present data dissect and test these models to unprecedented levels and show a remarkably good fit for multiplicativity and exchangeability of risk factors. Consistent with theoretical studies [28, 29], we could not distinguish between different kinds of similar multiplicative models, i.e., Log, Logit, or Probit.
Regarding the biological mechanisms leading to respective diseases, it is relevant to note that the most common risk alleles have no effects on protein structure but rather small effects on gene regulation. Thus, the diseases studied here seem to be largely driven by alterations of transcriptional activity. In other words, the cumulative number of common risk alleles in the population is in the hundreds, however, at a certain point, a few additional ones appear to destabilize a system of co-regulatory activity in various tissues which ultimately affects risk. Whereas at the low end of the frequency distributions, many risk alleles were tolerated with a lifetime disease prevalence of 2 percent or less, most individuals carried way more than this tolerable number of risk alleles. In summa, these appeared to disturb gene regulation to a degree that ultimately resulted in the high prevalence of CAD, T2DM, breast and prostate cancer, and likely other common diseases, particularly when modifiable risk factors come into play. Our data, therefore, provide empirical evidence for the liability threshold model of disease, whereby the combined effect of multiple risk variants with small effects jointly may create a steep increase in risk once a critical number is being passed [29, 30].
We found no evidence that CAD risk alleles affecting traditional risk factors such as hypercholesterolemia or hypertension, behaved any different from the vast majority of CAD risk alleles, which currently have neither established disease mechanisms nor specific treatments [1]. While this observation implies that the etiology of the diseases is more complex than thought, it also calls for additional strategies to lower the genetic risk of atherosclerosis and its complications. Indeed, the effects of risk alleles that increase lipids could be partially neutralized by a lower number of risk alleles with non-lipid-related effects. Vice versa, a lower count of lipid-related risk alleles was equally effective in lowering the risk of those carrying high numbers of non-lipid-related risk alleles. This is in line—and may explain—previous studies, which observed that LDL-cholesterol lowering is more effective in lowering cardiovascular risk in people with a high as compared to those with a low genetic risk score [31,32,33,34]. In other words, pharmacological neutralization of risk alleles that increase LDL-cholesterol leads to a more pronounced decrease in risk if the person carries overall a high number of risk alleles because cumulatively they increase risk exponentially. Not only is that risk higher in such individuals, but their benefit from therapy also appears to be higher as well, explaining by far lower numbers needed to treat for preventing events in people with a high genetic risk score[31,32,33,34]. Indirectly, the data also add genetic evidence for guidelines on primary prevention that recommend lipid-lowering treatment in subjects having high overall risk despite LDL-cholesterol levels way below the population average [35, 36].
Risk alleles exerted multiplicative effects also with exogenous risk factors, i.e. the more risk alleles a person carried the stronger were the risks associated with smoking, obesity or lack of physical exercise. Vice versa, in people free of risk factors, we observed relatively little differences in disease prevalence across the distribution spectrum of risk alleles. As an example, the increase of absolute CAD prevalence related to the increase in genetic risk between the first and tenth decile of the risk allele distribution was 1.69% in non-smoking, non-obese women whereas it was 21.1% for male smokers with obesity.
Our study has several limitations. Most importantly, we aimed at elucidating the principles on how common risk alleles interact with each other and the prevalence variation with and without traditional risk factors rather than defining their precise weights. Further studies, based on the recent expansion of GWAS, meta-analyses may do this for each percentile of a GRS [37]. Indeed, GRS involving millions of SNPs will result in more precise estimates of genetic risk across the full spectrum found in the population (Supplementary Table S8) [7]. Our data indicate how such refined estimates for each percentile of a GRS can be used for adjustment of the absolute risk—based on individual age, gender, and risk factor profile—a person carries. Indeed, understanding the non-linear relationship on combined genetic and exposure risk factors will help to inform physicians regarding the groups of patients having the largest benefit from preventive treatments [38]. Next, both populations studied here as well as the previous identification of common risk alleles by GWAS have focused on individuals with Western-European descent, such that our findings may only apply to this ancestry group. However, the discovery of variants displaying genome-wide significant associations is still ongoing, such that more variants will be discovered, in particular in currently under-represented ancestry populations [39]. In this sense, our data aim to illustrate genetic principles rather than to offer definite risk estimates across populations. Furthermore, although we show that risk alleles act multiplicatively in diverse diseases, the generalizability to other common diseases and additional environmental risk factors needs to be verified. In addition, although we have shown a strong non-linear model fit between the risk allele burden and prevalence, we could not distinguish model fits between logarithmic, Logistic and Probit models, consistent with theoretical studies [40].
Conclusion
In conclusion, we provide empirical evidence that genetic and non-genetic risk factors combine multiplicatively on prevalence and that they are exchangeable. Our results are consistent with gene–gene interactions and gene–environment relationship on the prevalence and a multiplicative model of liability to common disease, consistent with theoretical models that were proposed well before the GWAS era. Every person carries a large number of risk alleles yet a few more logarithmically increase disease prevalence explaining why the diseases we studied here are so common, a phenomenon that is largely exacerbated by modifiable risk factors. These findings offer a rationale for directing preventive efforts to individuals with a particularly high burden of combined genetic and non-genetic risk [31, 32, 41, 42].
Abbreviations
- SNP:
-
Single-nucleotide polymorphism
- CHR:
-
Chromosome
- BP:
-
Base pair
- OR:
-
Odds Ratio
- CAD:
-
Coronary artery disease
- T2DM:
-
Type 2 diabetes mellitus
- UKB:
-
UK biobank
- Est BB:
-
Estonian biobank
- wGRS:
-
Weighted genetic risk score
References
Erdmann J, Kessler T, Munoz Venegas L, Schunkert H (2018) A decade of genome-wide association studies for coronary artery disease: the challenges ahead. Cardiovasc Res 114:1241–1257. https://doi.org/10.1093/cvr/cvy084
Michailidou K, Lindström S, Dennis J et al (2017) Association analysis identifies 65 new breast cancer risk loci. Nature 551:92–94. https://doi.org/10.1038/nature24284
Schumacher FR, Al Olama AA, Berndt SI et al (2018) Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nat Genet 50:928–936. https://doi.org/10.1038/s41588-018-0142-8
Mahajan A, Taliun D, Thurner M et al (2018) Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet 50:1505–1513. https://doi.org/10.1038/s41588-018-0241-6
Hughes MF, Saarela O, Stritzke J et al (2012) Genetic markers enhance coronary risk prediction in men: the MORGAM prospective cohorts. PLoS ONE 7:e40922. https://doi.org/10.1371/journal.pone.0040922
Inouye M, Abraham G, Nelson CP et al (2018) Genomic risk prediction of coronary artery disease in 480,000 adults: implications for primary prevention. J Am Coll Cardiol 72:1883–1893. https://doi.org/10.1016/j.jacc.2018.07.079
Khera AV, Chaffin M, Aragam KG et al (2018) Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat Genet 50:1219–1224. https://doi.org/10.1038/s41588-018-0183-z
Goldstein DB (2009) Common genetic variation and human traits. N Engl J Med 360:1696–1698. https://doi.org/10.1056/NEJMp0806284
Mosley JD, Gupta DK, Tan J et al (2020) Predictive accuracy of a polygenic risk score compared with a clinical risk score for incident coronary heart disease. JAMA 323:627–635. https://doi.org/10.1001/jama.2019.21782
Elliott J, Bodinier B, Bond TA et al (2020) Predictive accuracy of a polygenic risk score-enhanced prediction model vs a clinical risk score for coronary artery disease. JAMA 323:636–645. https://doi.org/10.1001/jama.2019.22241
Sun L, Pennells L, Kaptoge S et al (2021) Polygenic risk scores in cardiovascular risk prediction: a cohort study and modelling analyses. PLoS Med 18:e1003498. https://doi.org/10.1371/JOURNAL.PMED.1003498
Samani NJ, Erdmann J, Hall AS et al (2007) Genomewide association analysis of coronary artery disease. N Engl J Med 357:443–453. https://doi.org/10.1056/NEJMOA072366/SUPPL_FILE/NEJMOA072366SA1.PDF
Buniello A, Macarthur JAL, Cerezo M et al (2019) The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res 47:D1005–D1012. https://doi.org/10.1093/nar/gky1120
Wray NR, Lin T, Austin J et al (2020) From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiat 78:101–109. https://doi.org/10.1001/jamapsychiatry.2020.3049
Pal Choudhury P, Brook MN, Hurson AN et al (2021) Comparative validation of the BOADICEA and Tyrer-Cuzick breast cancer risk models incorporating classical risk factors and polygenic risk in a population-based prospective cohort of women of European ancestry. Breast Cancer Res 23:1–5. https://doi.org/10.1186/s13058-021-01399-7
Choudhury PP, Wilcox AN, Brook MN et al (2021) Comparative validation of breast cancer risk prediction models and projections for future risk stratification. J Natl Cancer Inst 112:278–285. https://doi.org/10.1093/JNCI/DJZ113
Hurson AN, Pal Choudhury P, Gao C et al (2021) Prospective evaluation of a breast-cancer risk model integrating classical risk factors and polygenic risk in 15 cohorts from six countries. Int J Epidemiol. https://doi.org/10.1093/ije/dyab036
Aragam KG, Natarajan P (2020) Polygenic scores to assess atherosclerotic cardiovascular disease risk: clinical perspectives and basic implications. Circ Res. https://doi.org/10.1161/CIRCRESAHA.120.315928
Sudlow C, Gallacher J, Allen N et al (2015) UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12:e1001779
Leitsalu L, Haller T, Esko T et al (2015) Cohort profile: Estonian biobank of the Estonian genome center, university of Tartu. Int J Epidemiol 44:1137–1147. https://doi.org/10.1093/ije/dyt268
Nikpay M, Goel A, Won HH et al (2015) A comprehensive 1000 Genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet 47:1121–1130. https://doi.org/10.1038/ng.3396
European Environmental Agency (2020) R: A language and environment for statistical computing. R Found Stat Comput Vienna, Austria 24275
Falconer DS (1965) The inheritance of liability to certain diseases, estimated from the incidence among relatives. Ann Hum Genet 29:51–76. https://doi.org/10.1111/j.1469-1809.1965.tb00500.x
Risch N (1990) Linkage strategies for genetically complex traits. I. Multilocus models. Am J Hum Genet 46:222–228
Smith C (1971) Recurrence risks for multifactorial inheritance. Am J Hum Genet 23:578–588
Schliekelman P, Slatkin M (2002) Multiplex relative risk and estimation of the number of loci underlying an inherited disease. Am J Hum Genet 71:1369–1385. https://doi.org/10.1086/344779
Kapoor PM, Mavaddat N, Choudhury PP et al (2021) Combined associations of a polygenic risk score and classical risk factors with breast cancer risk. J Natl Cancer Inst 113:329–337. https://doi.org/10.1093/jnci/djaa056
Wray NR, Goddard ME (2010) Multi-locus models of genetic risk of disease. Genome Med 2:1–13. https://doi.org/10.1186/gm131
Slatkin M (2008) Exchangeable models of complex inherited diseases. Genetics 179:2253–2261. https://doi.org/10.1534/genetics.107.077719
Visscher PM, Wray NR (2016) Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered 80:165–170. https://doi.org/10.1159/000446931
Mega JL, Stitziel NO, Smith JG et al (2015) Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet 385:2264–2271. https://doi.org/10.1016/S0140-6736(14)61730-X
Natarajan P, Young R, Stitziel NO et al (2017) Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation 135:2091–2101. https://doi.org/10.1161/CIRCULATIONAHA.116.024436
Marston NA, Kamanu FK, Nordio F et al (2020) Predicting benefit from evolocumab therapy in patients with atherosclerotic disease using a genetic risk score. Circulation 141:616–623. https://doi.org/10.1161/CIRCULATIONAHA.119.043805
Damask A, Steg PG, Schwartz GG et al (2020) Patients with high genome-wide polygenic risk scores for coronary artery disease may receive greater clinical benefit from alirocumab treatment in the ODYSSEY OUTCOMES Trial. Circulation 141:624–636. https://doi.org/10.1161/CIRCULATIONAHA.119.044434
Arnett DK, Blumenthal RS, Albert MA et al (2019) 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140:596–646. https://doi.org/10.1161/CIR.0000000000000678
Mach F, Baigent C, Catapano AL et al (2020) 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 41:111–188. https://doi.org/10.1093/eurheartj/ehz455
Chen Z, Schunkert H (2021) Genetics of coronary artery disease in the post-GWAS era. J Intern Med. https://doi.org/10.1111/joim.13362
Torkamani A, Wineinger NE, Topol EJ (2018) The personal and clinical utility of polygenic risk scores. Nat Rev Genet 19:581–590. https://doi.org/10.1038/s41576-018-0018-x
Tcheandjieu C, Zhu X, Hilliard AT et al (2022) Large-scale genome-wide association study of coronary artery disease in genetically diverse populations. Nat Med.https://doi.org/10.1038/s41591-022-01891-3
Wray NR, Yang J, Goddard ME, Visscher PM (2010) The genetic interpretation of area under the ROC curve in genomic profiling. PLoS Genet 6:e1000864. https://doi.org/10.1371/journal.pgen.1000864
Graham SE, Clarke SL, Wu KH et al (2021) The power of genetic diversity in genome-wide association studies of lipids. Nature 600:675–679.https://doi.org/10.1038/s41586-021-04064-3
Khera AV, Emdin CA, Drake I et al (2016) Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med 375:2349–2358. https://doi.org/10.1056/NEJMoa1605086
Acknowledgements
We thank the participants and investigators of the GWAS explored in this analysis.
Funding
Open Access funding enabled and organized by Projekt DEAL. The author’s work was funded by the German Federal Ministry of Education and Research (BMBF) within the framework of ERA-NET on Cardiovascular Disease (Druggable-MI-genes: 01KL1802), within the scheme of target validation (BlockCAD: 16GW0198K), and within the framework of the e:Med research and funding concept (AbCD-Net: 01ZX1706C). As a Co-applicant of the British Heart Foundation (BHF)/German Centre of Cardiovascular Research (DZHK)-collaboration (DZHK-BHF: 81X2600522) and the Leducq Foundation for Cardiovascular Research (PlaqOmics: 18CVD02), we gratefully acknowledge their funding. Additional support has been received from the German Research Foundation (DFG) as part of the Sonderforschungsbereich SFB 1123 (B02) and the Sonderforschungsbereich SFB TRR 267 (B05). Furthermore, we kindly acknowledge the support of the Bavarian State Ministry of Health and Care who funded this work with DigiMed Bayern (Grant No: DMB-1805-0001) within its Masterplan “Bayern Digital II” and of the German Federal Ministry of Economics and Energy in its scheme of ModulMax (Grant No: ZF4590201BA8). CPN and NJS are supported by the British Heart Foundation and NJS is an emeritus NIHR Senior Investigator. L.Y. and P.M.V acknowledge funding from the Australian National Health and Medical Research Council (1113400) and the Australian Research Council (FL180100072, DE200100425).
Author information
Authors and Affiliations
Contributions
HS, PMV, AM and NJS conceived and designed the project, guided manuscript preparation. LY, SP, FB, CPN, LZ, LL, RM, KL and TK performed simulations and analyzed data. LY, JE and BMM performed the statistical analysis. All authors participated in manuscript drafting, and all authors reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare(s) that there is no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pang, S., Yengo, L., Nelson, C.P. et al. Genetic and modifiable risk factors combine multiplicatively in common disease. Clin Res Cardiol 112, 247–257 (2023). https://doi.org/10.1007/s00392-022-02081-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-022-02081-4