Abstract
Objective
To develop a validated clinical prognostic model to determine the risk of atrial fibrillation after cardiac surgery as part of the PARADISE project (NIHR131227).
Methods
Prospective cohort study with linked electronic health records from a cohort of 5.6 million people in the United Kingdom Clinical Practice Research Datalink from 1998 to 2016. For model development, we considered a priori candidate predictors including demographics, medical history, medications, and clinical biomarkers. We evaluated associations between covariates and the AF incidence at the end of follow-up using logistic regression with the least absolute shrinkage and selection operator. The model was validated internally with the bootstrap method; subsequent performance was examined by discrimination quantified with the c-statistic and calibration assessed by calibration plots. The study follows TRIPOD guidelines.
Results
Between 1998 and 2016, 33,464 patients received cardiac surgery among the 5,601,803 eligible individuals. The final model included 13-predictors at baseline: age, year of index surgery, elevated CHA2DS2-VASc score, congestive heart failure, hypertension, acute coronary syndromes, mitral valve disease, ventricular tachycardia, valve surgery, receiving two combined procedures (e.g., valve replacement + coronary artery bypass grafting), or three combined procedures in the index procedure, statin use, and ethnicity other than white or black (statins and ethnicity were protective). This model had an optimism-corrected C-statistic of 0.68 both for the derivation and validation cohort. Calibration was good.
Conclusions
We developed a model to identify a group of individuals at high risk of AF and adverse outcomes who could benefit from long-term arrhythmia monitoring, risk factor management, rhythm control and/or thromboprophylaxis.
Graphical abstract

Similar content being viewed by others
Introduction
Atrial fibrillation after cardiac surgery (AFACS) is frequent, occurring in 30–50% of cases [1]. Development of AFACS is associated with a number of perioperative pathophysiological and clinical factors [2]. Besides leading to longer hospital stays, AFACS has a prognostic impact, and has been associated with a higher risk of stroke, thromboembolism, and heart failure [3,4,5].
Interventions for preventing AFACS have shown to decrease AF incidence, length of hospital stay, and stroke [6]. Unfortunately, these treatments are not devoid of side effects. The Society of Cardiovascular Anesthesiologists and the European Association of Cardiothoracic Anaesthetists recommend different perioperative management depending on AFACS risk [7, 8]. However, there is no effective or validated way of risk stratifying these patients.
Strategies to identify patients at risk of developing AFACS would therefore be of interest and would allow the implementation of preventive strategies and more intensive monitoring to high-risk individuals. Some attempts have been made to develop prognostic schemes, but the currently available models [9,10,11] do not meet TRIPOD quality criteria [12].
A validated multivariable prognostic model allowing targeted prophylaxis is the first step to improving outcomes, informing patients, and resource planning. The objective of the study is to develop and validate a clinical prognostic model to determine the risk of a patient developing AFACS at the time of cardiac surgery.
Methods
This investigation is part of a project addressing a National Institute of Health Research (NIHR) call on AFACS—HTA no 19/132: “Predicting AF after Cardiac Surgery–the PARADISE Score. A Clinical Prediction Rule for Post-operative Atrial Fibrillation in Patients Undergoing Cardiac Surgery (PARADISE)”; NIHR131227. The PARADISE project aims to develop validated clinical prediction models to determine the risk of a patient developing AFACS: in the pre-operative assessment clinic or on admission for surgery (PARADISE-1) and on arrival in the post-operative care unit (PARADISE-2). In this paper, we will identify variables from a linked electronic health record dataset associated with AFCAS. In the near future, we will subsequently test these variables in British and American datasets and trials, with the aim of developing the PARADISE-1 score. Both PARADISE 1 and 2 will subsequently be validated in British, US-American and German real-world patient cohorts.
Study design, source of data, and population
We used a prospective cohort study to assess AF incidence among individuals with cardiac surgery. The Clinical Practice Research Datalink (CPRD) was established in 1987 and as of 2018 includes 7,998,501 patients in the UK with linked data of primary care consultation, hospital data (Hospital Episodes Statistics), national cancer registry (National Cancer Intelligence Network) and death registry data (Office for National Statistics—ONS) [13]. The data are generally representative of the age, gender, and geographic distribution of the UK population [13]. Previous validation studies of the UK nationwide EHR showed high quality and completeness of clinical information recorded in the data [14, 15]. The data used for the present study were approved by the MHRA (UK) Independent Scientific Advisory Committee [17_205], under Section 251 of the National Health Service (NHS) Social Care Act 2006. CALIBER has research ethics approval (09/H0810/16) and ECC approval (ECC 2-06(b)/2009 CALIBER dataset). The study followed the Transparent Reporting of a multivariable prognostic model for Individual Prognosis or Diagnosis (TRIPOD) recommendations [12].
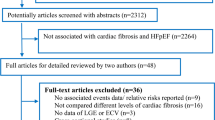
We identified individuals aged 18 years or older that had been registered in the current primary care practice for at least 1 year. The study period was between January 1, 1998, and May 31, 2016, and there were 401 practices included in the data (Fig. 1).
Participants
Individuals who underwent cardiac surgery were included in the study. The definition of cardiac surgery was based on the Office of Population Censuses and Surveys Classification of Surgical Operations and Procedures (4th revision, OPCS-4) [16] in hospitalisation and their corresponding primary care READ coding. The complete definition was summarised in supplementary table S1. Individuals were excluded if they had a prior history of AF or cardiac surgery before study entry. Follow-up ceased for the following reasons: death, the end date of registration with the practice, last day of the general practice data collection or the end of the study period (31 May 2016).
Outcome
The primary outcome was new-onset AF occurring after the date of cardiac surgery (AFACS). AF was defined from the International Classification of Diseases, tenth revision as I48 from HES and Read codes G573400, G573500, 3272.00, G573000, G573300, G573.00, G573z00 from CPRD. Based on the definition, AF cases included a minor proportion of atrial flutter [17]. The definition was developed and tested in cardiovascular disease research using linked bespoke studies and the electronic health records (CALIBER) platform (https://caliberresearch.org/portal) [18]. Previous research has shown high validity and completeness of the disease definition in AF and other conditions [19, 20]. We identified death, date of death and causes of death from the Office of National Statistics (ONS) records. New-onset AF included individuals with first AF diagnoses as the primary cause of death.
Predictors
We used the Index of Multiple Deprivation (IMD) 2015 quintile to describe socioeconomic status, with a higher quintile representing the more deprived areas [21]. For eligible participants, we identified 45 predictors reported in the literature [22], reported in a Delphi process [23] or with high prevalence observed in the study cohort: age at cardiac surgery, sex, ethnicity categories, smoking status, history of diabetes, hypertension, stable angina, unstable angina, myocardial infarction, stroke, dementia, heart failure, chronic obstructive pulmonary disease, chronic kidney disease, cancer, asthma, valvular disease, deep vein thrombosis, pulmonary embolism, mitral valve disease, supraventricular tachycardia, cardiogenic shock, ventricular tachycardia, transient ischemic attack, hypothyroidism, dyslipidaemia, systolic blood pressure, diastolic blood pressure, calendar year at study entry [24], the use of anticoagulants, antiplatelet drugs, anti-arrhythmic drugs, beta-adrenoceptor blocking drugs, diuretics, warfarin, hypertension and heart failure drugs, statin, NSAIDS, cardiac glycosides, immunosuppressants, inotropic drugs. The CHA2DS2-VASc score was calculated [25], as a measure of stroke risk although prior studies have examined the role of this score in predicting AFCAS [26]. CHA2DS2-VASc Score and categorised into elevated CHA2DS2-VASc Score (≥ 1 for men and ≥ 2 for women). We reported the proportion of individuals with a diagnosis recorded in their primary care or hospital admissions, before their initial documentation of cardiac surgery. Diagnosis code lists for each condition were adapted from the CALIBER code repository (Supplementary table S2).
Statistical analyses
Baseline characteristics were presented among derivation and validation groups. We reported frequencies (%) for categorical data and means with standard deviation for continuous data, and chi-square and t tests were used to examine the difference between sex and socioeconomic categories. The extent of missing values was assessed and then managed by recoding for categorical variables or multiple imputations for continuous variables.
Model construction
Univariable models were used to examine non-linear trends. We used multivariable logistic regression with the least absolute shrinkage and selection operator (LASSO) for model building [27]. Variance inflation factors were calculated to detect evidence of multicollinearity problems in the model selection process. The minimum sample size for developing the was estimated [28]. Assuming a 0.21 prevalence of AF post cardiac surgery, 50 parameters (including dummy variables of predictors), and a Cox-Snell R2 of 0.0208. We estimated the minimum sample size required for new model development was 21,384.
Model validation and performance
Model validation was implemented by internal bootstrap validation [29]. Model performance was examined by assessing discrimination and calibration in the study cohort. Discrimination was quantified with the c-statistic. Model calibration was assessed by calibration plots [30] and Hosmer–Lemeshow goodness-of-fit tests.
Additional analyses were performed using random forests for variable selection in constructing the prognostic model, with the 100 trees built from the randomly split training (75% of the full cohort) and validation (25% of the full cohort) populations. We performed the analyses in the secured Data Safe Haven, meeting the data safety and information governance requirements by University College London, NHS Digital and ONS. Analyses were performed in SAS (version 9.4), R (version 3.6.1) and Stata (version 16.1). The funders did not have any role in the study design, data collection, data analysis, interpretation, and writing of the report.
Public and patient involvement
Patients were involved in the Delphi process for the selection of potential candidate variables, and will be involved in the dissemination of the study results.
Results
The mean age of the 33,464 patients who received cardiac surgery was 57.3 years (standard deviation 13.5 years). 29.2% of the patients were women. Frequent comorbidities included hypertension (prevalence at baseline: 41.1%), ischaemic heart disease (38.7%), angina (37.3%), myocardial infarction (30.4%), and valvular disease (23.2%). (Table 1).
There were 6902 (20.6%) individuals with AFACS reported. The incidence of AF was 20.8% in patients receiving bypass surgery and 29.4% among patients receiving valve surgery.
The C-statistic of the full model with 49 covariates was 0.69. LASSO selection of variables concluded in a final model with 13 predictors at baseline: including age (centred at 60 years), elevated CHA2DS2-VASc score, congestive heart failure, hypertension, acute coronary syndromes, mitral valve disease, ventricular tachycardia, statin use, valve surgery, receiving two combined procedures (e.g., heart valve repair + coronary artery bypass grafting), or three combined procedures (e.g., dual heart valve replacement + coronary artery bypass grafting) in the index cardiac surgery, ethnicity other than white or black, and year of the index surgery (Fig. 2). Statin use and ethnicity other than white or black were associated with a protective effect. Valve surgery as a type of cardiac surgical procedure was the strongest predictor of AFACS.
This model had a C-statistic of 0.68 in the estimation cohort. The C index for the prognostic model in the bootstrapping validation was 0.68, confirming the model has a moderate discrimination ability to identify patients at risk of AFACS. The model was well calibrated (Fig. 3). Sensitivity analyses with random forest model selection reported similar performance to the prognostic model (with the area under the curve: 0.64) (Supplementary Figs. 1, 2).
Analysis of the performance of the model showed that three quarters of the 7750 patients with valvular heart disease were classified as having a high or highest risk for developing new-onset AFACS (Table S3). Most cases (nearly 90%) of the 2214 new-onset AFACS events in patients with valvular heart disease were detected in the groups with high or highest AF risk as defined by our model (Table S4).
The AFACS risk profile of patients without valvular heart disease was lower, with more than half being assigned to the low or lowest risk groups. However, most of the new-onset AF cases in this group was also detected in the highest AFACS risk classes as defined by our model.
Finally, we estimated subsequent stroke occurrences in the different Predicted AFACS risk groups, as defined by our model, and observed that of the 2514 strokes occurring during follow-up ¾ were observed in the high or highest AFACS risk groups (Table S5).
Discussion
In this multi-center cohort study, we successfully developed and validated an AF incidence prediction model for patients receiving cardiac surgery. The model showed adequate validity with a C-index of 0.68 and had good calibration for predicting AFACS.
From the predictors of AFACS in the model, we found that older age, elevated CHA2DS2-VASc score, history of congestive heart failure, hypertension, acute coronary syndromes, mitral valve disease, ventricular tachycardia at the time of cardiac surgery and earlier year of surgery performed, receiving valve surgery or multiple procedures performed during the index cardiac surgery were significantly associated with the subsequent AFACS, as documented in previous literature. We also found that statin use and ethnicity other than white or black were more likely to have a better prognosis (i.e., protective factors). These results have been consistent with previous reports.
Individuals with a higher risk of AFACS were more frequently diagnosed with AF and sustained more strokes during follow-up. This suggests that individuals with a higher risk of AFACS, as identified through our model, may represent a sub-population in whom mid to long-term arrhythmia monitoring (e.g., with implantable loop recorders) may be of interest, and measures like risk factor management, rhythm control and/or anticoagulation should be tested in future trials.
This study has several strengths. First, the large sample size of a total of 33,464 patients provides sufficient power in its results. Second, by including all patients receiving cardiac surgery the outcome can be representative of the national population of patients. Third, the use of a wide range of predictor variables, including socio-demographic data and data on clinical factors, and fourth the reproducibility of the model has been confirmed by bootstrapping validation and the performance was better than the modelling method using random forest. Our model also has several limitations. Detailed biomarker information, and information on clinical types of AF (paroxysmal or persistent), is not available for all patients. However, even though it is important to understand whether AFACS has a different prognosis or clinical impact depending on whether it is self-limited, behaving like paroxysmal AF (the most frequent occurrence according to Lin et al. [31]), or if it progresses to a more persistent form, the aim of our investigation was to develop a predictive model for AFACS, new-onset AF after cardiac surgery, irrespectively of its subsequent behaviour or burden. It is possible that the inclusion of additional variables could have improved the discrimination of the model and can be investigated in future research. The C-index of 0.68 is indicative of the multifactorial nature of risk for patients receiving cardiac surgery who subsequently developed AF. However, since strong statistically significant predictors were found, we can still draw important conclusions about how changes in the predictor values are associated with changes in the outcome, consistent with the literature.
Implications and future research
Clinicians can utilize information from electronic health records to identify patients with a greater AFACS risk to aid the prioritisation of preventive care. This study will feed into the PARADISE-1 risk score, which aims at identifying patients at risk of AFACS prior to cardiac surgery. Combining some of the identified variables with biomarkers and imaging parameters may lead to better discrimination. The performance of any future scores can also be improved by adding intra-operatory variables or measures (as planned for PARADISE-2). Our research also supports future studies on other clinical outcomes, such as cerebrovascular ischemic events, following cardiac surgery, and interventions aimed at preventing them. An important aspect to clarify in future studies, as prevention treatment in the AFACS population starts to be considered, is the impact of AF burden or AF clinical type (paroxysmal vs. persistent) on subsequent clinical outcomes. This knowledge gap was highlighted in a systematic review by Lin et al. [31] assessing the impact of AFACS on mortality and stroke. The authors highlighted that none of the 35 included studies separately reported events for paroxysmal and persistent AF.
Conclusion
We established and validated a prognostic model for new-onset atrial fibrillation among patients who received cardiac surgery. This model, or a future iteration utilizing some of its variables, can be useful to identify a group of high-risk individuals who could benefit from mid to long-term arrhythmia monitoring, risk factor management, rhythm control and/or thromboprophylaxis.
References
Lowres N, Mulcahy G, Jin K et al (2018) Incidence of postoperative atrial fibrillation recurrence in patients discharged in sinus rhythm after cardiac surgery: a systematic review and meta-analysis. Interact Cardio Thorac Surg 26:504–511. https://doi.org/10.1093/icvts/ivx348
Kaireviciute D, Aidietis A, Lip GYH (2009) Atrial fibrillation following cardiac surgery: Clinical features and preventative strategies. Eur Heart J 30:410–425. https://doi.org/10.1093/eurheartj/ehn609
Badhwar V, Rankin JS, Thourani VH et al (2018) The society of thoracic surgeons adult cardiac surgery database: 2018 update on research: outcomes analysis, quality improvement, and patient safety. Ann Thorac Surg 106:8–13. https://doi.org/10.1016/j.athoracsur.2018.04.052
Gialdini G, Nearing K, Bhave PD et al (2014) Perioperative atrial fibrillation and long-term risk of ischemic stroke. JAMA 312:616–622. https://doi.org/10.1001/jama.2014.9143
Lapar DJ, Speir AM, Crosby IK et al (2014) Postoperative atrial fibrillation significantly increases mortality, hospital readmission, and hospital costs. Ann Thorac Surg 98:527–533. https://doi.org/10.1016/j.athoracsur.2014.03.039
Burgess DC, Kilborn MJ, Keech AC (2006) Interventions for prevention of post-operative atrial fibrillation and its complications after cardiac surgery: a meta-analysis. Eur Heart J 27(2846):57. https://doi.org/10.1093/eurheartj/ehl272
Burrage PS, Low YH, Campbell NG et al (2019) New-onset atrial fibrillation in adult patients after cardiac surgery. Curr Anesthesiol Rep 9:174–193. https://doi.org/10.1007/s40140-019-00321-4
Muehlschlegel JD, Burrage PS, Ngai JY et al (2019) Society of cardiovascular anesthesiologists/European association of cardiothoracic anaesthetists practice advisory for the management of perioperative atrial fibrillation in patients undergoing cardiac surgery. Anesth Analg 128:33–42. https://doi.org/10.1213/ANE.0000000000003865
Kolek MJ, Muehlschlegel JD, Bush WS et al (2016) A combined genetic and clinical risk prediction model for postoperative atrial fibrillation. Circ Arrhythm Electrophysiol 8:25–31. https://doi.org/10.1161/CIRCEP.114.002300
Tran DTT, Perry JJ, Dupuis JY et al (2015) Predicting new-onset postoperative atrial fibrillation in cardiac surgery patients. J Cardiothorac Vasc Anesth 29:1117–1126. https://doi.org/10.1053/j.jvca.2014.12.012
Cameron MJ, Tran DTT, Abboud J et al (2018) Prospective external validation of three preoperative risk scores for prediction of new onset atrial fibrillation after cardiac surgery. Anesth Analg 126:33–38. https://doi.org/10.1213/ANE.0000000000002112
Moons KG, Altman DG, Reitsma JB et al (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:W1-73. https://doi.org/10.7326/M14-0698
Padmanabhan S, Carty L, Cameron E et al (2019) Approach to record linkage of primary care data from clinical practice research datalink to other health-related patient data: overview and implications. Eur J Epidemiol 34:91–99. https://doi.org/10.1007/s10654-018-0442-4
Setakis E, Puri S, Williams TJ et al (2018) Representiveness of subset of the general practice research database (GPRD) linked to other data sources. Pharmacoepidemiol Drug Saf 736:19
Herrett E, Thomas SL, Schoonen WM et al (2010) Validation and validity of diagnoses in the general practice research database: a systematic review. Br J Clin Pharm 69:4–14. https://doi.org/10.1111/j.1365-2125.2009.03537.x
NHS Digital. National clinical coding standards OPCS-4. Accurate data for quality information. Accessed at https://classbrowser.nhs.uk/ref_books/OPCS-4.9_NCCS-2021.pdf (2022)
Rix TA, Riahi S, Overvad K et al (2012) Validity of the diagnoses atrial fibrillation and atrial flutter in a Danish patient registry. Scand Cardiovasc J 46:149–153. https://doi.org/10.3109/14017431.2012.673728
Denaxas S, Gonzalez-Izquierdo A, Direk K et al (2019) UK phenomics platform for developing and validating electronic health record phenotypes: CALIBER. J Am Med Inform Assoc 26:1545–1559. https://doi.org/10.1093/jamia/ocz105
Chung SCSR, Acosta-Mena D, Taylor J et al (2021) Atrial fibrillation epidemiology, disparity and healthcare contacts: a population-wide study of 5.6 million individuals. Lancet Reg Health Europe 7:100157. https://doi.org/10.1016/j.lanepe.2021.100157
Morley KI, Wallace J, Denaxas SC et al (2014) Defining disease phenotypes using national linked electronic health records: a case study of atrial fibrillation. PLoS ONE 9:e110900. https://doi.org/10.1371/journal.pone.0110900
Department for communities and local government (DCLG). The english index of multiple deprivation 2015: guidance. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015. (2022)
Muehlschlegel JD, Alhassan H, Fields K et al. (2019) Preoperative risk prediction models for atrial fibrillation after cardiac surgery: a systematic review and retrospective external validation. Prospero CRD42019127329
Bedford JP, Harford M, Petrinic T et al (2019) Risk factors for new-onset atrial fibrillation on the general adult ICU: a systematic review. J Crit Care 53:169–175. https://doi.org/10.1016/j.jcrc.2019.06.015
Pate A, van Staa T, Emsley R (2020) An assessment of the potential miscalibration of cardiovascular disease risk predictions caused by a secular trend in cardiovascular disease in England. BMC Med Res Methodol 20:289. https://doi.org/10.1186/s12874-020-01173-x
Lip GY, Nieuwlaat R, Pisters R et al (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137:263–272. https://doi.org/10.1378/chest.09-1584
Chen Y, Zeng M, Liu Y et al (2020) CHA2DS2-VASc score for identifying patients at high risk of postoperative atrial fibrillation after cardiac surgery: a meta-analysis. Ann Thorac Surg 109:1210–1216. https://doi.org/10.1016/j.athoracsur.2019.07.084
BL. Logistic model selection with SAS® PROC’s Logistic, hplogistic, hpgenselect. Paper AA02. Paper presented at: MidWest SAS Users Group; 2017; St Louis, MO
Riley RD, Ensor J, Snell KIE et al (2020) Calculating the sample size required for developing a clinical prediction model. BMJ 368:m441. https://doi.org/10.1136/bmj.m441
Lankham I, Slaughter M. Simple and efficient bootstrap validation of predictive models using SAS/STAT® Software. Paper 4647–2020. SAS Global Forum https://www.sas.com/content/dam/SAS/support/en/sas-global-forum-proceedings/2020/4647-2020.pdf (2020)
Austin PC, Steyerberg EW (2014) Graphical assessment of internal and external calibration of logistic regression models by using loess smoothers. Stat Med 33:517–535. https://doi.org/10.1002/sim.5941
Lin M, Kamel H, Singer DE et al (2019) Perioperative/postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke 50:1364–1371. https://doi.org/10.1161/STROKEAHA.118.023921
Funding
Open Access funding enabled and organized by Projekt DEAL. NIHR131227: “Predicting AF after Cardiac Surgery–the PARADISE Score. A Clinical Prediction Rule for Post-operative Atrial Fibrillation in Patients Undergoing Cardiac Surgery (PARADISE)”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, SC., O’Brien, B., Lip, G.Y.H. et al. Prognostic model for atrial fibrillation after cardiac surgery: a UK cohort study. Clin Res Cardiol 112, 227–235 (2023). https://doi.org/10.1007/s00392-022-02068-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-022-02068-1