Abstract
Background
Collateral damage of the COVID-19 pandemic on cardiovascular health is increasingly studied. This is a population-based study addressing multiple aspects of cardiovascular care during the pandemic in a country of Lithuania, in which pandemic waves were significantly different.
Methods
Data on cardiology outpatient care, hospitalizations and cardiovascular mortality in 2019 and 2020 were collected from Lithuanian nationwide administrative databases and registries. Weekly data and aggregated numbers of corresponding 6-week phases were analyzed comparing the numbers between 2019 and 2020. Age, sex and regional subgroup analysis was performed.
Results
Both cardiovascular outpatient care visits and hospitalizations decreased dramatically in 2020 compared to 2019 with a peak reduction (up to − 60% for both) during the first pandemic wave in spring of 2020. Simultaneously, cardiovascular mortality was much higher in 2020, with a pronounced peak at the end of the year compared to 2019 (up to 46%). The increase was even more staggering when analyzing home deaths, which rose up to 91% by the end of 2020. Notable differences between age groups, regions and sexes were documented.
Conclusion
A profound indirect damage of COVID-19 pandemic on cardiovascular care was observed in this study, with striking decreases in cardiovascular care provision and concurrent increase in cardiovascular mortality, both overall and, even more dramatically, at home.
Trial registration
ClinicalTrials.gov: NCT05021575 (registration date 25–08–2021, retrospectively registered).
Graphical abstract

Similar content being viewed by others
Introduction
During the spring of 2020, a lot of countries were severely affected by the first pandemic wave, and, unsurprisingly, most of the studies focused on direct impact of COVID-19 on community health. The collateral damage of COVID-19 pandemic on the provision of cardiovascular (CV) care and cardiovascular mortality has been noticed early and reported in several nationwide and selected cohort studies [1,2,3,4].
The research was mainly focused on acute coronary and other acute CV syndromes; changes in-hospital admissions and early mortality after myocardial infarction were also often analyzed [2, 3]. Meanwhile, a substantial proportion of routine appointments, diagnostic and therapeutic procedures was canceled, with unclear impact of total changes in CV provision on patient prognosis. Data on the changes in total national CV services, including out- and in-patient health care facilities, acute and chronic conditions due to all CV diagnoses, during the outbreak, between the two pandemic waves and onwards are scarce.
First confirmed case of COVID-19 in Lithuania was recorded on 28th February 2020. Nationwide quarantine was introduced by Lithuanian government on 16th March and ended on 16th June 2020. In the period before the end of quarantine 1 773 COVID-19 cases were recorded and 86 patients (of whom 10 patients died from other causes after testing positive for SARS-CoV-2) had died. In that period, Lithuania was reported among the least affected countries according to World Health Organization [5]. However, during quarantine Lithuanian government limited contact appointments to urgent conditions only. The utmost efforts to provide triage, follow-up care by telephone call and e-prescriptions were recommended. This greatly affected availability of cardiovascular care.
The second pandemic wave in Lithuania was substantially more severe [6]. Consequently, the second nationwide quarantine was implemented on 7th November 2020, which ended on 30th June 2021. Contact appointments were not limited by the government this time; however, the scope of CV care was again negatively affected, probably for multiple reasons.
The objectives of this population-based study were: (1) to assess the impact of the COVID-19 pandemic on provision of CV care at the national and regional level; (2) to compare the parallel changes of CV mortality in Lithuania in 2020 to the same period of 2019; (3) to evaluate sex and age differences in changes of CV care provision and CV deaths during the pandemic.
Methodology
Data collection
Effects of COVID-19 Pandemic on a Health Care System: Case Study of the CirculatORy System in LiThuania (COVID-COR-LT, NCT05021575) was a population-based study performed in collaboration with nationwide registries. Outpatient and hospitalization data from 1 January 2019 to 30 November 2020 were obtained from National Health Insurance Fund. This system covers more than 99% of Lithuanian health care facilities and collects data from electronic health records. To ensure completeness of outpatient data related to cardiovascular diseases (CVD) different approaches were used: (1) data on visits were collected using ICD-10 codes I00-I99 and other CVD related codes (e.g., certain Z, Q codes, J81.0, R57.0); (2) data were collected from CVD prevention program; (3) data on interventional cardiology were collected from day care facility regardless of the diagnosis. Date of the visit, patient age, sex and municipality, service level (primary, secondary, or tertiary), type of service and main diagnosis were recorded.
Data on hospitalization was collected if any of the diagnoses (principal or secondary) were in I00-I99 range. Hospitalization data covered hospitalization date, patient age, sex, municipality, and outcome. Data on CV procedures performed during hospitalizations included date of the procedure and ACHI (Australian Classification of Health Interventions) code.
Data on CV mortality was obtained from death certificates provided by Causes of Death Registry from Institute of Hygiene. Death certificates are uploaded to electronic system and reviewed by dedicated registry specialists, according to WHO recommendations. Uncertain cases are additionally compared with the data from Compulsory Insurance Information System SVEIDRA and, if it is not yet clear, nosologists of the Registry contact the doctor who issued the e-certificate. Death certificates were included in the study when cause of death was adjudicated to be in I00-I99 range. Date and place of death, patient age and sex were recorded. Four options can be selected in death certificate for death place—hospital, home, other or unspecified. For death place analyses, certificates where place of death was unspecified (< 0.5% of all death certificates) were excluded. Mortality data covered the period from 1 January 2019 to 31 December 2020. The study was approved by Vilnius Regional Biomedical Research Ethics Committee (Nr. 2020/8–1247-730) and conducted in accordance with the Declaration of Helsinki.
Data analysis
Weekly data using complete weeks (Monday-Sunday) were analyzed, hence weeks 2–48 of outpatient care and hospitalizations and weeks 2–52 of CV mortality were investigated and compared, respectively between 2019 and 2020. We calculated 4-week moving average of all analyzed aspects, averaging data over each 4-week period, starting 3 weeks prior to the week of interest. This method facilitates visualization of trends and comparison between respective periods by smoothing out variability of data. Reference lines for the first COVID-19 case (week 9), start of the 1st quarantine (week 12), end of the 1st quarantine (week 25) and start of the 2nd quarantine (week 45) were added to all weekly graphs. We also divided the study period to corresponding 6-week phases, containing the same number of workdays in 2019 and 2020: (1) 6 weeks before quarantine (2) 1st stage of quarantine (3) 2nd stage of quarantine (4) 1–6 weeks after quarantine (5) 7–12 weeks after quarantine (6) 13–18 weeks after quarantine (7) 19–24 weeks after quarantine (see Online Resource 1). The last periods also cover the beginning of the second pandemic wave in Lithuania and a second nationwide quarantine.
Regional differences in out- and in-patient care were analyzed by creating informational maps coloring ten Lithuanian counties according to percental change in outpatient and hospital services during the first quarantine compared to corresponding period in 2019.
Sex differences were evaluated performing weekly data analyses in men and women. Cases, when sex was not available (< 0.01% in hospitalization and outpatient data) were excluded from this analysis.
Data were analyzed in adult (> 18 years old) patients only. Patients were divided into age groups (18–39, 40–49, 50–59, 60–69, 70–79, 80–89, 90 +). We examined how outpatient care, hospitalizations and CV mortality differed between these groups in the 1st quarantine period (16th March–16th June of 2020) and compared this data to respective period in 2019 (18th March–18th June).
Data are provided per 100,000 population, using 2019 and 2020 estimated monthly populations as reported by National Health Insurance Fund (see Online Resource 1). Associated 95% confidence intervals (CIs) were estimated by calculating standard error (SE) of proportion (rate per 100,000 population) and using CI formula: Sample statistic ± 1.96*SE. In addition, we calculated percentage change from the corresponding period in 2019 together with 95% CIs using the Wilson score interval in all analyses described above.
Continuous variables are presented as median and interquartile ranges [IQR], categorical variables are presented as counts (percentage). The differences between study groups were compared using Kruskal–Wallis test for continuous variables and χ2 test for the categorical variables. Statistical analysis and data visualization was performed with R version R 4.0.3 (The ‘R’ Foundation for Statistical Computing) and Tableau Software version 2020.3.3.
Results
Provision of CV care
The total number of ambulatory appointments for CV reasons from January 1st until November 30 in 2020 was 1,694,417 (60,643/100,000 population) versus 2,146,908 (76,878/100,000 population, -21%) in 2019, with 1,377,101 (49,287/100,000) vs 1,737,625 (62,222/100,000, -21%) visits to general practitioners, 229,954 (8,230/100,000) vs 283,537 (10,153/100,000,—19%) visits to specialized secondary care and 87,362 (3,127/100,000) vs 125,746 (4,503/100,000, − 31%) visits to tertiary care, respectively. The first COVID-19 case in Lithuania was registered on February 28 (week 9), since then a rapid decline in the scale of outpatient visits at all levels has been observed—see Figs. 1A, 2.
Comparison of numbers of outpatient cardiovascular visits in Lithuania in 2019 and 2020. A Weekly variations of the outpatient cardiovascular visits. Vertical reference lines denote important dates of the pandemic in Lithuania. B Number of outpatient cardiovascular visits in 6-week periods before, during and after quarantine
The peak reduction of outpatient visits occurred at weeks 13–21 of 2020 (up to 57%, Fig. 1A), relatively less in primary care (up to 52%), more in secondary (up to 73%) and maximally in tertiary care (up to 85%) (Fig. 2). Dividing study period into phases in relation to lockdown, the prominent fall of 55% in cumulative outpatient CV visits can be seen during the first stage of the quarantine, with 38% decrease during the second stage (Fig. 1B). Since week 19 of the year, the partial recovery of outpatient service had started, however, even at week 38 (since September 21) it still did not reach the baseline level, with the persisting decline in specialized care (Figs. 1A, 2). A recurrent decrease in ambulatory care was again observed after implementation of 2nd quarantine (weeks 45–48 of 2020).
In the time of officially announced 1st quarantine period, which lasted 12 weeks, a cumulative number of primary care visits have reduced by 42%, referrals to cardiologists by 66%; preventive and rehabilitation services have extremely decreased—see Table 1.
During study period in 2019 total number of hospitalizations due to CV reasons accounted for 101,939 cases (3,650/100,000) over Lithuania, while in the corresponding period of 2020 it reduced to 76,623 (2,742/100,000, − 26%) cases—see Fig. 3. The dip in admissions had started in pre-lockdown phase, which is reflected in a steep decrease in a moving average after start of quarantine. At weeks 13–20 of 2020 in-patient care decreased dramatically: up to 60% (Fig. 3A). The prominent fall of 59% in cumulative in-patient CV cases can be seen during the first stage of the 1st quarantine, with 40% decrease during the second stage (Fig. 3B). Among in-hospital procedures the least drop occurred in percutaneous coronary interventions (PCIs) for acute myocardial infarction (by 20%), while the greatest scaling down was documented for valve and coronary surgery (− 63% and − 57%, respectively), as well as for total invasive coronary angiographies (− 52%)—see Table 2. In contrast to the dynamics of outpatient appointments, number of cardiovascular hospitalizations remained persistently and markedly decreased after 1st quarantine, by 21% before the 2nd quarantine and declined even further after week 45.
Comparison of numbers of cardiovascular hospitalizations in Lithuania in 2019 and 2020. A Weekly variations of the cardiovascular hospitalizations. Vertical reference lines denote important dates of the pandemic in Lithuania. B Number of cardiovascular hospitalizations in 6-week periods before, during and after quarantine
We found regional heterogeneity in the reduction of ambulatory and hospital services throughout 10 Lithuanian districts (Fig. 4). For example, in the Western districts number of all outpatient visits fell by approximately 30%, whereas in the Eastern districts the decrease was substantially larger: 42–43%.
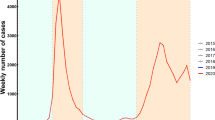
CV mortality
Between 1st January and 31st December in 2019 and 2020, 20,894 (748/100,000) and 22,937 (821/100,000) CV deaths (+ 10%), respectively, were documented. Weekly fluctuations in the number of CV deaths are shown in Fig. 5A. First peak of excess CV deaths in 2020 compared to 2019 was registered as early as at weeks 16–18 (first stage of 1st quarantine) and reached an increase of 13%. This acute effect of pandemic was followed by a stabilization period from week 20 to week 24 (second stage of 1st quarantine), after which a delayed long-term excess in CV mortality was observed, reaching an increase of 46% by the end of the 2020 compared to 2019 (Fig. 5A). During the first stage of 1st quarantine cumulative number of deaths rose by 11% and remained persistently increased by 11–12% between the two quarantines. At the start of 2nd quarantine, the cumulative number of deaths was 35% higher than in the same period of 2019.
Striking redistribution in the place of CV deaths was found comparing 2020 with 2019: much more deaths happened at home during the pandemic, reaching the maximum increase of 37–41% at weeks 17–18 (end of April) and moving up extremely up to 40–91% in November and December—see Fig. 6A. Notably, throughout all periods of year 2020 risk of dying at home was greater compared to 2019, with most prominent elevations during the spring quarantine and with the rise of the second pandemic wave and the late autumn quarantine (Fig. 6B).
At the same time remarkable deviation of in-hospital mortality was registered during the two quarantines—see Fig. 7. Concomitantly with drop in CV admissions, in-hospital mortality went up dramatically: from baseline 6–7% in 2019 to 13–14% in corresponding periods of 2020 (Fig. 7). However, absolute number of in-hospital deaths decreased by 14–16% during the first quarantine, stabilized between the two quarantines, and then, conversely, increased by up to 21% after the start of second quarantine (see Online Resource 1).
To investigate any possible direct influence of COVID-19 on cardiovascular mortality, we examined the secondary diagnoses listed in the death certificates for COVID-19, pneumonia or other acute respiratory illnesses (see Online Resource 1). Only 3% of the cardiovascular death certificates in 2020 had COVID-19 listed as a secondary diagnosis and proportions of other acute respiratory diseases were smaller or comparable to 2019.
Age and sex subgroups
Of note, reduction of outpatient visits was dependent on age: it was the greatest in younger subjects, with proportionate preservation of ambulatory care with increasing age (Fig. 8A). Conversely, the fall of hospital CV admissions was similar in all age groups (Fig. 8B). Also, the age gradient in excess CV mortality was detected: increase of deaths was larger, although not statistically significant, in the younger age groups (36–47%), statistically significant in age groups 50–59 and 70–79, while death rate of octo- and nonagenarians did not change—see Fig. 9. During the first quarantine, a significant difference in age was observed between the patients deceased in 2020 compared to 2019 (82 [72–88] vs. 83 [74–88] years, respectively, p = 0.002), this difference disappeared when analyzing the whole year.
The reduction of CV out- and in-patient care did not vary with sex (see Online Resource 1); however, during the first pandemic wave, increase in CV mortality was more pronounced in men than in women (up to 19% vs up to 9%, respectively, Fig. 10A). Conversely, after the start of second quarantine, redundant CV mortality increased more in women compared to men (up to 51% vs up to 40%, respectively, Fig. 10A). The difference was even more striking when analyzing home deaths—although the increase was greater in men up until the second wave, after it, the mortality at home increased exponentially in women (up to 110% by the end of the year, Fig. 10B), and less so in men.
Discussion
Our population-based study clearly demonstrates a dramatic effect of COVID-19 pandemic on provision of CV care and CV mortality in Lithuania. To our knowledge, this is the first study to systematically investigate changes in the total nationwide CV care and parallel changes in the death rate due to CV reasons. There was a striking reduction in CV outpatient care and CV hospitalizations, whereas cardiovascular mortality increased compared to corresponding periods in 2019. Also, our analysis is one of the first covering not only pre-pandemic period and first pandemic wave, but also a delayed period after it and a part of a more severe second wave.
Out-patient care
A reduction in outpatient care during the pandemic was observed in several studies. Wosik J [7] showed a 33% decline of outpatient CV visits between March 15 and June 30, 2020, within the Duke University Health System in the US. A decline of nearly 60 percent of all outpatient visits (including cardiology) in April 2020 was highlighted by Mehrotra A [8]. A resurgence in outpatient care was observed in this study in later months, but until October there still was a persistent reduction of 10% in cardiology visits compared to pre-pandemic period [8]. At U.S. Department of Veterans Affairs despite the twofold increase of the tele-health visits during the first 10 weeks of the pandemic, overall number of outpatient visits still decreased by 30% [9]. Not only quantitative but also structural changes in the primary care delivery are reported, with less assessment of blood pressure, cholesterol level concomitantly with less office-based visits in the US [10].
In our study, we compared weekly data of CV outpatient visits from January to November with corresponding weeks in 2019. Our results confirm the data from previous studies, as a significant drop in services during quarantine is followed by a prolonged recovery to a previous level.
Our research is rather unique for its deeper analysis based on the level of care. This additional analysis revealed that specialized cardiology care had especially declined, with up to 85% reduction of the tertiary referrals, while 50% of appointments to general practitioners were preserved (the proportion of teleconsultations among them was not available). The overall return to the pre-pandemic scale in October was mainly owing to primary and secondary level outpatient visits, while the number of tertiary CV consultations remained markedly declined. A repeated decline throughout all levels at the beginning of the 2nd quarantine was observed with the most pronounced reduction in the tertiary care again.
Hospitalizations
Bhatt AS [11] highlighted the 43% fall of acute hospitalizations due to CVD during the first phase of the COVID-19 pandemic in Massachusetts, U.S. In Monaco, total CV admissions went down by only 18% in March 2020 compared to March 2019, which the authors attribute to a well-organized public health care system [12]. The systematic review of 103 observational studies reported a decline of hospitalizations for acute coronary syndrome, ischemic strokes and heart failure in 89% of studies, with reductions ranging from 20 to 73% during the pandemic [13]. Between March 11 and April 21, 2020, the number of patients admitted to the U.S. Department of Veterans Affairs for myocardial infarction and heart failure decreased by 40.3% and 49.1%, respectively [14]. We extended the analysis to all CV hospitalizations, regardless of the diagnosis, and, in parallel with previous publications, observed a prominent fall up to 60% in April 2020, compared to 2019. A similar drop in CV admission rate during that period was reported in Germany [15]. We also demonstrated a remarkable decrease in diagnostic and therapeutic percutaneous procedures, pacemaker implantations, and rates of cardiac surgery—up to 57–63% during the spring quarantine in 2020. Acute treatment, such as PCI for myocardial infarction, was mostly preserved: the change reached only − 10%. The hospitalization rate had not recovered to pre-lockdown numbers during the period between the two quarantines and dropped again with the rise of the second pandemic wave.
Mortality
The combination of lockdown orders, constant media coverage and fear of the novel virus took a toll on the healthcare systems around the world and may have caused an increase in COVID-19 unrelated mortality observed in several studies. Wu J et al. [16] demonstrated that during pandemic in England and Wales acute CV mortality increased by 8% with increase in a death rate at home and simultaneous decrease in-hospital deaths. Similarly, a lockdown period was associated with an increase of CV mortality by 7.6% in central Germany [17]. Data from the National Center for Health Statistics in US showed that deaths caused by ischemic heart disease and hypertensive disease increased in some regions during the initial phase of the COVID-19 pandemic [18].
During the spring of 2020, quarantine measures were introduced early in Lithuania reflecting the serious situation in other countries. Notably, Lithuania was among the least affected countries until the beginning of autumn of 2020 [6]. Despite a relatively low burden of COVID-19 in the spring, we found that weekly CV death rate increased by as high as 13% during the early first quarantine phase compared to 2019. In the later phase, mortality rate stabilized, however, in the following months after quarantine it rose again to 46%. The second pandemic wave affected Lithuania more severely, and consequently a lot of medical resources had to be reallocated to sustain the mounting numbers of infected patients. This burden on the health care system and an observed striking CV care disturbance, reflected in reduction in CV outpatient care and hospitalizations, might have had an adverse impact on CV patients. This hypothesis is further supported by a considerably higher proportion of death at home and lower absolute number of in-hospital death during the first quarantine compared with the same time period in 2019, reflecting avoidance to seek medical care [19]. Analogous data were documented in 4 Italian regions with 52% increase of out-of-hospital cardiac arrest in the very early phase of COVID-19 pandemic [20]. A corresponding redistribution of death places was also reported in a study of Danish citizens with CV disease [21]. Furthermore, during the more severe second pandemic wave, death rate at home has risen even more, reaching up to 90% difference compared to the autumn of the previous year.
We observed that the highest proportions of weekly in-hospital mortality were recorded during the same weeks when numbers of CV hospitalizations were the lowest, although the absolute number of in-hospital deaths was lower during the first quarantine. This finding most probably reflects the extreme situation when only patients with urgent and severe conditions were hospitalized. This was also reported in a systematic review of twenty-three studies analyzing several acute CV conditions, with worse in-hospital outcomes during the pandemic [13]. However, the start of the second pandemic wave resulted in an increase in absolute death rate both at home and in hospital.
Interestingly, there was a significant reduction in CV mortality in 2020 prior to the pandemic, compared to the same period of the previous year. Similar phenomenon was also observed in an aforementioned Danish analysis [21]. We can hypothesize that this reflected a long-term tendency of a decreasing CV mortality and had the COVID-19 pandemic and a concomitant lockdown not occurred, the mortality would have further decreased throughout the year.
Differences by age and sex
We detected that there were considerable age-related differences in outpatient appointments during the spring quarantine with a more pronounced decline in younger patients. This phenomenon was also documented by Mehrotra A [8]. It could be explained by the greater activity of older patients with established chronic diseases who actively seek outpatient care and are under closer supervision, while healthier or not yet diagnosed younger patients could postpone visits.
In the publication of Stöhr E [22], reporting a 20% decline of CV hospital admissions during COVID-19 lockdown in Western Germany, a greater drop of emergency admissions was seen for patients ≥ 60 years. Conversely, a decline of hospitalization rate fluctuated little among all age groups in our study. There were no differences in hospitalization rate between men and women in the aforementioned study; our results corresponded with this finding.
We found several age-related CV mortality differences during spring quarantine, with a higher increase in mortality in younger subjects (prominent from 18 to 59 years) and virtually no difference in the oldest age groups (namely, in patients older than 80 years).
While the reduction in out and in-patient care was irrespective of sex, we found striking differences in mortality between women and men. There was an early impact of the pandemic in men, which parallels other studies that reported higher mortality related to the pandemic in men [21, 23], however we documented a later increased in mortality and grave delayed consequences of the pandemic in women, which contrasted previous findings. Our results presumably correspond to previously reported generally worse CV outcomes in women [24].
Strengths and limitations
In the present study, we analyze complex unselected data from both nationwide outpatient care and hospitalizations, and mortality registries. We also provide information on a health care system from a country in Eastern/Central European region, which has not been presented as much as other regions in previous studies [25]. Furthermore, our analysis covers two very different periods—first pandemic wave, when the burden of COVID-19 in Lithuania was relatively small while the lockdown measures were rather strict, and the second wave, which affected Lithuania and its health care system more severely. Our study, however, has a few limitations. Due to the observational nature of the study and limited availability of clinical data, we cannot draw unambiguous conclusions about the reasons for the increase in CV mortality and the pronounced differences between mortality of women and men. Due to the short term of our project, we had to halt the collection of outpatient and in-patient data in November 2020 and the mortality data at December, 2020, therefore our data covers only the beginning of the second wave. However, this is one of the most extensive studies on CV care during the COVID-19 pandemic.
Implications
Our study adds to the growing concern of the grave collateral damage of lockdown measures [21, 25]. It will probably take a lot of years and colossal research efforts to determine the full extent of this effect. Measures taken to control the coronavirus pandemic and consequences may have been rather similar around the world, but our findings in context of other studies warrant further research into how the same measures affected different regions with different health care systems.
Conclusion
In summary, our study provides evidence of a partly collapsed CV care in Lithuania during the first pandemic wave, post-pandemic period and the rise of the second pandemic wave. Regardless of a relatively small number of COVID-19 cases during the first wave, a persistent negative impact on CV care has expanded far to the period between the quarantines and has grown even further in the second quarantine. Simultaneously with a more severe rise in coronavirus cases during the second pandemic wave, this disturbance in the health care system led to grave cardiovascular outcomes and will possibly affect cardiovascular patients for years to come.
Abbreviations
- ACHI:
-
Australian Classification of Health Interventions
- AMI:
-
Acute myocardial infarction
- CABG:
-
Coronary artery bypass grafting
- CIs:
-
Confidence intervals
- COVID-19:
-
Coronavirus disease 2019
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular diseases
- ED:
-
Emergency department
- ICA:
-
Invasive coronary angiography
- ICD:
-
Implantable cardioverter-defibrillator
- ICD-10:
-
International Statistical Classification of Diseases and Related Health Problems 10th Revision
- PCI:
-
Percutaneous coronary intervention
- SE:
-
Standard error
- WHO:
-
World Health Organization
References
Ball S, Banerjee A, Berry C, Boyle JR, Bray B, Bradlow W, Chaudhry A, Crawley R, Danesh J, Denniston A, Falter F, Figueroa JD, Hall C, Hemingway H, Jefferson E, Johnson T, King G, Lee KK, McKean P, Mason S, Mills NL, Pearson E, Pirmohamed M, Poon MTC, Priedon R, Shah A, Sofat R, Sterne JAC, Strachan FE, Sudlow CLM, Szarka Z, Whiteley W, Wyatt M, CVD-COVID-UK Consortium (2020) Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart Br Card Soc 106:1890–1897. https://doi.org/10.1136/heartjnl-2020-317870
Kiss P, Carcel C, Hockham C, Peters SAE (2021) The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes 7:18–27. https://doi.org/10.1093/ehjqcco/qcaa084
Andersson C, Gerds T, Fosbøl E, Phelps M, Andersen J, Lamberts M, Holt A, Butt JH, Madelaire C, Gislason G, Torp-Pedersen C, Køber L, Schou M (2020) Incidence of new-onset and worsening heart failure before and after the COVID-19 epidemic lockdown in Denmark: a nationwide cohort study. Circ Heart Fail 13:e007274. https://doi.org/10.1161/CIRCHEARTFAILURE.120.007274
Brant LCC, Nascimento BR, Teixeira RA, Lopes MACQ, Malta DC, Oliveira GMM, Ribeiro ALP (2020) Excess of cardiovascular deaths during the COVID-19 pandemic in Brazilian capital cities. Heart Br Card Soc 106:1898–1905. https://doi.org/10.1136/heartjnl-2020-317663
Coronavirus Disease (COVID-19) Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 25 Jul 2021
Lithuania: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data. https://covid19.who.int. Accessed 25 Jul 2021
Wosik J, Clowse MEB, Overton R, Adagarla B, Economou-Zavlanos N, Cavalier J, Henao R, Piccini JP, Thomas L, Pencina MJ, Pagidipati NJ (2021) Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am Heart J 231:1–5. https://doi.org/10.1016/j.ahj.2020.10.074
Impact COVID Outpatient Care: Visits Prepandemic Levels but Not All | Commonwealth Fund. https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels. Accessed 25 Jul 2021
Baum A, Kaboli PJ, Schwartz MD (2021) Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med 174:129–131. https://doi.org/10.7326/M20-3026
Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS (2020) Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open 3:e2021476. https://doi.org/10.1001/jamanetworkopen.2020.21476
Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD, Vaduganathan M (2020) Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol 76:280–288. https://doi.org/10.1016/j.jacc.2020.05.038
Enache B, Claessens Y-E, Boulay F, Dor V, Eker A, Civaia F, Pathak A (2020) Reduction in cardiovascular emergency admissions in Monaco during the COVID-19 pandemic. Clin Res Cardiol Off J Ger Card Soc 109:1577–1578. https://doi.org/10.1007/s00392-020-01687-w
Seidu S, Kunutsor SK, Cos X, Khunti K (2021) Indirect impact of the COVID-19 pandemic on hospitalisations for cardiometabolic conditions and their management: a systematic review. Prim Care Diabetes 15:653–681. https://doi.org/10.1016/j.pcd.2021.05.011
Baum A, Schwartz MD (2020) Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA 324:96–99. https://doi.org/10.1001/jama.2020.9972
Seiffert M, Brunner FJ, Remmel M, Thomalla G, Marschall U, L’Hoest H, Acar L, Debus ES, Blankenberg S, Gerloff C, Behrendt C-A (2020) Temporal trends in the presentation of cardiovascular and cerebrovascular emergencies during the COVID-19 pandemic in Germany: an analysis of health insurance claims. Clin Res Cardiol Off J Ger Card Soc 109:1540–1548. https://doi.org/10.1007/s00392-020-01723-9
Wu J, Mamas MA, Mohamed MO, Kwok CS, Roebuck C, Humberstone B, Denwood T, Luescher T, de Belder MA, Deanfield JE, Gale CP (2021) Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart Br Card Soc 107:113–119. https://doi.org/10.1136/heartjnl-2020-317912
Nef HM, Elsässer A, Möllmann H, Abdel-Hadi M, Bauer T, Brück M, Eggebrecht H, Ehrlich JR, Ferrari MW, Fichtlscherer S, Hink U, Hölschermann H, Kacapor R, Koeth O, Korboukov S, Lamparter S, Laspoulas AJ, Lehmann R, Liebetrau C, Plücker T, Pons-Kühnemann J, Schächinger V, Schieffer B, Schott P, Schulze M, Teupe C, Vasa-Nicotera M, Weber M, Weinbrenner C, Werner G, Hamm CW, Dörr O, CoVCAD –Study Group (2021) Impact of the COVID-19 pandemic on cardiovascular mortality and catherization activity during the lockdown in central Germany: an observational study. Clin Res Cardiol Off J Ger Card Soc 110:292–301. https://doi.org/10.1007/s00392-020-01780-0
Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW (2021) Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol 77:159–169. https://doi.org/10.1016/j.jacc.2020.10.055
Tsioufis K, Chrysohoou C, Leontsinis I, Tousoulis D (2020) Unveiling the mystery of “missing” emergencies in the era of COVID-19 pandemic: a generalized phenomenon with unclarified implications. Clin Res Cardiol Off J Ger Card Soc 109:1580–1581. https://doi.org/10.1007/s00392-020-01700-2
Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G, Reali F, Parogni P, Facchin F, Rizzi U, Bussi D, Ruggeri S, Oltrona Visconti L, Savastano S, Lombardia CARe researchers (2020) COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J 41:3045–3054. https://doi.org/10.1093/eurheartj/ehaa508
Butt JH, Fosbøl EL, Gerds TA, Andersson C, Kragholm K, Biering-Sørensen T, Andersen J, Phelps M, Andersen MP, Gislason G, Torp-Pedersen C, Køber L, Schou M (2021) All-cause mortality and location of death in patients with established cardiovascular disease before, during, and after the COVID-19 lockdown: a Danish Nationwide Cohort Study. Eur Heart J 42:1516–1523. https://doi.org/10.1093/eurheartj/ehab028
Stöhr E, Aksoy A, Campbell M, Al Zaidi M, Öztürk C, Vorloeper J, Lange J, Sugiura A, Wilde N, Becher MU, Diepenseifen C, Heister U, Nickenig G, Zimmer S, Tiyerili V (2020) Hospital admissions during Covid-19 lock-down in Germany: Differences in discretionary and unavoidable cardiovascular events. PLoS ONE 15:e0242653. https://doi.org/10.1371/journal.pone.0242653
Mohamed MO, Gale CP, Kontopantelis E, Doran T, de Belder M, Asaria M, Luscher T, Wu J, Rashid M, Stephenson C, Denwood T, Roebuck C, Deanfield J, Mamas MA (2020) Sex differences in mortality rates and underlying conditions for COVID-19 deaths in England and Wales. Mayo Clin Proc 95:2110–2124. https://doi.org/10.1016/j.mayocp.2020.07.009
Aggarwal NR, Patel HN, Mehta LS, Sanghani RM, Lundberg GP, Lewis SJ, Mendelson MA, Wood MJ, Volgman AS, Mieres JH (2018) Sex differences in ischemic heart disease: advances, obstacles, and next steps. Circ Cardiovasc Qual Outcomes 11:e004437. https://doi.org/10.1161/CIRCOUTCOMES.117.004437
Cannatà A, Bromage DI, McDonagh TA (2021) The collateral cardiovascular damage of COVID-19: only history will reveal the depth of the iceberg. Eur Heart J 42:1524–1527. https://doi.org/10.1093/eurheartj/ehab097
Funding
The work was supported by the Research Council of Lithuania (Lietuvos mokslo taryba), grant Nr. S-COV-20-27. Research Council of Lithuania was not involved in study design, data collection, analysis and interpretation, writing the paper, and the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Čelutkienė, J., Čerlinskaitė-Bajorė, K., Bajoras, V. et al. Collateral effect of the COVID-19 pandemic on cardiology service provision and cardiovascular mortality in a population-based study: COVID-COR-LT. Clin Res Cardiol 111, 1130–1146 (2022). https://doi.org/10.1007/s00392-022-02033-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-022-02033-y