Abstract
Improving glucose sensitivity remains an unmet medical need in treating type 2 diabetes (T2D). Dorzagliatin is a dual-acting, orally bioavailable glucokinase activator that enhances glucokinase activity in a glucose-dependent manner, improves glucose-stimulated insulin secretion and demonstrates effects on glycemic control in patients with T2D. We report the findings of a randomized, double-blind, placebo-controlled phase 3 clinical trial to evaluate the efficacy and safety of dorzagliatin in patients with T2D. Eligible drug-naïve patients with T2D (n = 463) were randomly assigned to the dorzagliatin or placebo group at a ratio of 2:1 for 24 weeks of double-blind treatment, followed by 28 weeks of open-label treatment with dorzagliatin for all patients. The primary efficacy endpoint was the change in glycated hemoglobin from baseline to week 24. Safety was assessed throughout the trial. At week 24, the least-squares mean change in glycated hemoglobin from baseline (95% confidence interval) was −1.07% (−1.19%, −0.95%) in the dorzagliatin group and −0.50% (−0.68%, −0.32%) in the placebo group (estimated treatment difference, −0.57%; 95% confidence interval: −0.79%, −0.36%; P < 0.001). The incidence of adverse events was similar between the two groups. There were no severe hypoglycemia events or drug-related serious adverse events in the dorzagliatin group. In summary, dorzagliatin improved glycemic control in drug-naïve patients with T2D and showed a good tolerability and safety profile.
Similar content being viewed by others
Main
The global population with diabetes has increased from 151 million to 537 million people worldwide in the past two decades, 90–95% of whom have T2D1. T2D is characterized by a progressive deterioration of beta-cell function, which is associated with a continuous decline in insulin secretion function and is commonly related to insulin resistance2. Despite the availability of antidiabetic medications from nine different classes, only 49.2% of patients with T2D in China achieved the control target of a glycated hemoglobin (HbA1c) level of <7.0%3. Therapeutics such as metformin, glucagon-like peptide-1 (GLP-1) receptor agonists (liraglutide) and insulin (insulin glargine) failed to achieve durable improvements in beta-cell function in drug-naïve patients with T2D after the drug withdrawal4. Patients with T2D show marked delay in early-phase insulin secretion in response to glucose5,6. Targeting the earlier phases of insulin secretion, by improving glucose sensitivity, could be a valuable approach to improve beta-cell function7. New antidiabetic agents that directly target the driver of early-phase insulin secretion in glucose-stimulated insulin secretion (GSIS) are needed to optimize diabetes management8,9,10.
The first report of glucokinase was published in 1968 by Matschinsky, which identified glucokinase’s critical role in hepatic glucose metabolism and also its presence in insulin-producing islets of Langerhans of obese mice11. In beta cells, glycolysis is a transducer for triggering physiological GSIS12. Glucokinase is the first rate-limiting enzyme of glycolysis expressed in pancreatic beta cells and plays a central role in the GSIS-triggering process13. Glucokinase is recognized as a glucose sensor due to its regulation of set points in glucose homeostasis11,12,14,15. Inactivating and activating glucokinase genetic mutations cause critical impacts on the threshold of GSIS16. Homozygous and heterozygous inactivating mutations in the glucokinase gene are associated with the development of permanent neonatal diabetes, a life-threatening disease requiring intensive and lifelong insulin treatment17, and maturity-onset diabetes of the young type 2, which shows reduced insulin secretion in response to glucose stimulation and decreased hepatic glycogen content18,19, respectively. By contrast, activating mutations lead to clinical hyperinsulinemia, the most common cause of persistent hypoglycemia in newborns20. Glucokinase is also present in pancreatic alpha cells and intrinsically regulates glucagon secretion21,22,23. The majority of glucokinase is found in hepatocytes, where it is tightly regulated by the glucokinase regulatory protein in response to hepatic glucose changes and it controls hepatic glucose uptake and glycogen synthesis24. In patients with T2D, the reduction in glucokinase expression and activity in the pancreas and liver might explain the impaired GSIS, insulin resistance and loss of glycemic control. The reduction in glucokinase expression in the pancreas and liver has been reported by Matschinsky and Haeusler25,26. A substantial decrease in pancreas glucokinase activity was found in T2D islets, which showed impaired GSIS function25. A reduction of glucokinase expression in the range of 50–60% was found in the livers of patients with T2D whose HbA1c was above 7.0%26. Decreased expression of glucokinase in the liver and reduction of hepatic glycogen contents were associated with hypermethylation in the hepatic glucokinase gene promoter and were involved in increasing the age-dependent susceptibility to hepatic insulin resistance and diabetes27. Some evidence was also found for a defect in hepatic glucokinase activity in T2D28,29.
Glucokinase activators (GKAs) are a class of small molecules that bind to an allosteric site on glucokinase and aim to restore glucokinase function in patients with T2D. GKAs can be classified as pancreas and liver dual-acting GKAs30,31,32 and liver-selective GKAs33. Additionally, GKAs can be divided into full GKAs31,32,34 and partial GKAs35,36. Challenges emerged through phase 2 trials during the clinical development of GKAs for T2D37,38,39,40,41,42, such as problems related to hypoglycemia, unsustainable efficacy and other adverse reactions38 (Supplementary Table 143,44,45,46,47. Over the past 5 years, considerable progress has been made in developing GKAs, such as dorzagliatin, which showed good efficacy and safety profiles along with a low incidence of hypoglycemia in a 12-week study of patients with T2D48. GKAs have also been developed for diseases other than T2D, including TTP399 for type 1 diabetes (T1D)49 and AZD1656 for reducing mortality in patients with diabetes who were infected with severe acute respiratory syndrome coronavirus 2 (ref. 50).
Dorzagliatin is an orally bioavailable, dual-acting full GKA (molecular weight, 462.94 g mol−1) that activates pancreatic and hepatic glucokinase in a glucose-dependent manner to improve glycemic control in patients with T2D. Dorzagliatin demonstrated positive effects on recovering the number of insulin-secreting cells in the pancreas and on the glucokinase expression at both mRNA and protein levels in the livers of diabetic rats51. Multiple phase 1 trials34,52,53 and one phase 2 trial48 of dorzagliatin have been completed in China and the United States. In addition to effectively reducing 24-h plasma glucose levels, dorzagliatin improved the GSIS in patients with T2D who were treated for 28 days, as indicated by a significant increase in the early-phase insulin secretion index (ΔC30/ΔG30) and homeostasis model assessment 2 of beta-cell function (HOMA2-β) from baseline in a phase 1 trial52. Patients who were treated with dorzagliatin monotherapy of 75 mg twice a day for 12 weeks in a phase 2 trial showed significant improvement in the glucose disposition index and reductions in insulin resistance indicated by homeostasis model assessment 2 of insulin resistance (HOMA2-IR), which were sustained at 1 week after drug withdrawal48. This trial (SEED) is a phase 3 placebo-controlled study of dorzagliatin in drug-naïve patients with T2D, comprising 24 weeks of double-blind treatment followed by 28 weeks of open-label treatment to evaluate the efficacy and long-term safety of dorzagliatin.
Results
Patient demographics and clinical characteristics
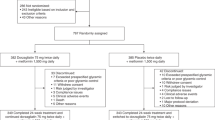
Patients were recruited from 18 July 2017 to 28 February 2019, and the last patient visit was conducted on 6 March 2020. Of the 975 patients screened, 463 eligible patients were randomly assigned to one of two treatment groups: 310 patients received dorzagliatin 75 mg twice a day, and 153 patients were assigned to the placebo group (Fig. 1). A total of 457 patients received at least one dose of the study drug and had HbA1c measurements at baseline and at least one post-baseline time point. Among all of the patients who underwent randomization, 401 (86.6%) patients completed the 24 weeks of double-blind treatment (281 (90.6%) in the dorzagliatin group and 120 (78.4%) in the placebo group). All patients were switched to dorzagliatin treatment after the 24-week double-blind period. Subsequently, 351 (75.8%) patients completed 52 weeks of treatment (246 (79.4%) from the original dorzagliatin group and 105 (68.6%) from the original placebo group; Fig. 1 and Extended Data Fig. 1). Among the 463 randomized patients, 301 (65%) were male and 162 (35%) were female. The average age of the study patients was 53.3 ± 9.7 years, and the average duration of disease was 11.7 ± 8.7 months. The patients had an average body mass index (BMI) of 25.5 ± 2.9 kg/m2 and a mean HbA1c value of 8.4% ± 0.7%. The demographic and baseline characteristics were similar between the two groups (Table 1).
Efficacy outcomes
The primary outcome at week 24 was achieved. The HbA1c level was reduced from baseline by 1.07% (95% confidence interval (CI): −1.19%, −0.95%) in the dorzagliatin group and by 0.50% (95% CI: −0.68%, −0.32%) in the placebo group (estimated treatment difference (ETD), −0.57%; 95% CI: −0.79%, −0.36%; P < 0.001; Fig. 2a, Table 2 and Supplementary Table 2).
a, The least-squares (LS) mean changes in the HbA1c level from baseline at week 24 in patients who received either dorzagliatin or placebo. The ETD and corresponding 95% CI were estimated using an MMRM without missing-value imputation in the FAS (dorzagliatin, n = 306; placebo, n = 148); P < 0.001. b, HbA1c level over 24 weeks in patients who received either dorzagliatin or placebo at each visit. c, The LS mean change in 2h-PPG from baseline. ETD and 95% CI were estimated in the FAS using a mixed model of repeated measure (MMRM) (dorzagliatin, n = 293; placebo, n = 133). d, The LS mean change in FPG from baseline. ETD and 95% CI were estimated in the FAS using an MMRM (dorzagliatin, n = 306; placebo, n = 148). e, The mean value of HbA1c over 52 weeks at each visit. The FAS comprised all randomized patients who took at least one dose of the study drug and had at least one posttreatment measurement of the primary endpoint during the double-blind treatment period. All statistical tests were two sided at a significance level of 0.05, and no adjustments were made for multiplicity. Data in a, c and d are presented as LS means ± s.e., and data in b and e are presented as means ± s.e.
The secondary outcome showed that the reduction in HbA1c levels in the dorzagliatin group started at week 4, reaching the maximum reduction at week 12 (Fig. 2b, Table 2 and Supplementary Table 2). The effects of dorzagliatin on reducing 2-h post-challenge glucose (2h-PPG) and fasting plasma glucose (FPG) levels at week 24 compared to placebo are also shown (Fig. 2c,d, Table 2 and Supplementary Tables 3 and 4). A greater decrease in the 2h-PPG level was observed after treatment with dorzagliatin than with placebo (−50.9 mg dl−1 versus −9.0 mg dl−1; ETD, −41.94 mg dl−1; 95% CI: −57.06 mg dl−1, −26.82 mg dl−1; Fig. 2c, Table 2 and Supplementary Table 4). In addition, the FPG level showed a greater reduction in the dorzagliatin group than in the placebo group (−10.4 mg dl−1 versus −4.7 mg dl−1; ETD, −5.94 mg dl−1; 95% CI: −13.68 mg dl−1, 1.98 mg dl−1; Fig. 2d, Table 2 and Supplementary Table 3).
At week 24, 42.5% of the patients in the dorzagliatin group versus 17.3% in the placebo group achieved an HbA1c level of <7.0% (odds ratio (OR), 4.20; 95% CI: 2.51, 7.02). HbA1c levels of <7.0% were achieved by week 8 in 40.8% of patients on dorzagliatin versus 10.0% of patients on placebo, respectively, and were sustained until week 24 (Table 2).
The exploratory endpoints included the composite endpoint (an HbA1c level of <7.0% without hypoglycemia and no weight gain) and HOMA2-β at week 24. The composite endpoint in the dorzagliatin group was 29.4% at week 24, compared with 13.3% in the placebo group (OR, 2.87; 95% CI: 1.66, 4.96; Table 2). In addition, HOMA2-β showed consistent improvement at week 24 in the dorzagliatin group compared with the placebo group (+2.56 change from baseline with dorzagliatin versus −0.72 with placebo; ETD, 3.28; 95% CI: 0.44, 6.11; Table 2).
Moreover, from week 24 to week 52, in the open-label treatment period, the reduction in HbA1c observed in the dorzagliatin group during the double-blind period of the trial was sustained with reductions of 1.15% ± 1.10% and 1.11% ± 1.00% from baseline at week 24 and week 52, respectively. A decrease of 1.27% ± 1.02% in HbA1c levels from baseline was also observed in the original placebo group after the switch to dorzagliatin treatment at week 52 (Fig. 2e and Supplementary Table 5).
Post hoc analyses were performed to explore outcomes other than primary and secondary endpoints. The time to first achieving an HbA1c level of <7.0% was shorter in the dorzagliatin group than in the placebo group (12.1 weeks versus not estimable, respectively; Table 2).
Safety outcomes
During the 24-week double-blind treatment period, at least one adverse event was reported in 240 of 310 patients (77%) in the dorzagliatin group and 103 of 153 patients (67%) in the placebo group (Table 3). Most of the adverse events were mild and resolved during treatment, and the investigators considered them unrelated to the drug (Supplementary Table 8). No clustering of serious adverse events in any organ system occurred (Supplementary Table 9). In addition, no severe hypoglycemia events or drug-related serious adverse events were observed in the dorzagliatin group. The adverse events that occurred in at least 5% of the patients were upper respiratory tract infection, hyperlipidemia, protein in urine, abnormal hepatic function and hypertension, in order, which are mostly not related to investigational drug judged by investigators (Table 3). During the open-label treatment period, the rates of both adverse events and serious adverse events remained the same in terms of type and incidence as those that occurred during the double-blind treatment period. No deaths were reported during the study (Supplementary Table 8).
Clinically significant hypoglycemia (blood glucose level < 54 mg dl−1) was reported in 1 (0.3%) of the 310 patients in the dorzagliatin group during the 24-week double-blind period and none of the 281 patients during the 28-week open-label period (Table 3 and Supplementary Table 8), whereas it was reported in none of the 153 patients in the placebo group during the 24-week double-blind period and 1 (1%) of the 120 patients during the 28-week open-label period (Table 3 and Supplementary Table 8). The incidence of exposure-adjusted events for clinically significant hypoglycemia over the 52 weeks was 0.006 events per patient year.
There were no significant differences in blood pressure or BMI between the two groups. All laboratory indicators related to liver and kidney function were within the normal ranges during the study. Regarding blood lipids, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were also within the normal range. At the same time, triglyceride level showed a minor increase at week 24 without further change noted over the 52 weeks of treatment (Table 4). The incidence of hyperlipidemia was 12% in the dorzagliatin group and 11% in the placebo group. Only one case of a hyperlipidemia adverse event in the dorzagliatin group was judged by investigators to be related to dorzagliatin (Table 3).
Discussion
The SEED study was a phase 3 trial to evaluate the efficacy and long-term safety of dorzagliatin, a GKA, as monotherapy in drug-naïve patients with T2D. The population enrolled in the SEED study had a new diagnosis of T2D, were on a diet and exercise regimen for at least 3 months and had not previously received any antidiabetic treatment. The baseline characteristics of the participants reflect a group of patients with T2D primarily with impaired pancreatic beta-cell function rather than insulin resistance with an increased postprandial glucose and relatively high HbA1c (baseline of 8.4%). The SEED study achieved its primary efficacy endpoint of a reduction in HbA1c compared to placebo in a 24-week double-blind period.
Dorzagliatin had a good safety profile during the 52-week treatment period, with no drug-related serious adverse events or severe hypoglycemia that required medical assistance. Clinically significant hypoglycemia (blood glucose < 54 mg dl−1) occurred in one patient (0.3%) treated with dorzagliatin over 24 weeks, and the incident was mild in nature.
GSIS plays a central role in the glucose regulation of pancreatic beta cells. Despite an initial failure with GKAs in phase 2 clinical trials, such as piragliatin37 and MK-0941 (ref. 38), it has led to the understanding that glucokinase plays a glucose-sensing role in GSIS. The failure was due to clinical hypoglycemia induced by the disruption of the GSIS threshold. Allosteric GKAs developed for diabetes therapeutics can change the kinetic parameters of the glucokinase, such as the Hill coefficient, the changes of which can result in the alteration of its glucose-dependent activity, showing different clinical outcomes during their development. The excessive decrease in the Hill coefficient by GKAs might be the primary cause of a reduced GSIS threshold and an increased incidence of clinical hypoglycemia13,38,54. MK-0941 changed the GSIS threshold to 45 mg dl−1 of glucose, which is similar to the value under the effects of activating glucokinase mutations31,55. The chemical structure of dorzagliatin is markedly different from that of MK-0941, and it has shown minimum disruption of Hill coefficient values of glucokinase. In a phase 2 study, dorzagliatin demonstrated improved glucose dependency of insulin secretion and increased glucose sensitivity with low hypoglycemia risks48. Among the partial GKAs, AZD1656 and PF-04937319 are the two leading candidates evaluated in phase 2 trials. PF-04937319 is currently being studied in China in phase 3 trials56, and AZD1656 has shown encouraging outcomes for the reduction of overall coronavirus disease 2019 mortality in patients with diabetes in the ARCADIA study50. A liver-selective GKA, TTP399, which is chemically modified to optimize its uptake into hepatocytes and prevent its entry into pancreatic beta cells, has been developed for T2D and was shown to achieve sustained glycemic control without dyslipidemia with 6 months of treatment33. TTP399 also demonstrated benefits in patients with T1D when used as an adjunct treatment with insulin49.
Dorzagliatin also showed other clinical outcomes in different study populations through several phase 1 trials. In a combination study of dorzagliatin with sitagliptin in patients with T2D in the United States, active GLP-1 was increased in the dorzagliatin plus sitagliptin regimen compared to dorzagliatin alone, while GLP-1 secretion in the dorzagliatin alone was markedly enhanced compared with the combination therapy. In addition, dorzagliatin showed a synergistic glycemic reduction with the addition of sitagliptin57. Improved postprandial glucose control was observed using dorzagliatin as an add-on therapy to empagliflozin, an SGLT2 inhibitor, in patients with T2D in the United States57. Dorzagliatin was also studied in a population with end-stage renal disease and a healthy control group to evaluate the effect of renal impairment on pharmacokinetics and safety. The results suggested that dorzagliatin can be safely used in patients with T2D at all stages of renal impairment without a need for dose adjustment58.
The current study has several limitations. First, the SEED study focused on patients likely in the early stage of T2D, selected from newly diagnosed drug-naïve patients with T2D whose blood glucose was not controlled by diet and exercise regimens. Another phase 3 trial, the DAWN study59, was completed in patients with moderate T2D who had inadequate glycemic control using metformin alone. Therefore, the conclusions may not be generalizable to patients with severe T2D, and more clinical studies are needed. Second, both phase 3 studies were carried out in China; dorzagliatin has been evaluated in four phase 1 studies in the United States, including the pharmacological evaluation of combined dorzagliatin with metformin, sitagliptin and empagliflozin. Thus, long-term clinical studies in Europe and the United States are needed to evaluate the clinical benefit of dorzagliatin to the different T2D populations compared to Chinese populations. Third, according to ethical requirements, the duration of placebo observation in a diabetes monotherapy trial was limited to no more than 24 weeks; patients in the placebo group crossed over to dorzagliatin treatment during the extended 28-week open-label treatment period. No control group was designed for the entire 52-week period in this study. The total observation time in SEED was 52 weeks, and more time will be needed to observe dorzagliatin’s effects on cardiovascular and renal outcomes. No comparison with other hypoglycemic drugs was established in the SEED study, which will need to be considered in future trials. By the end of the 24-week double-blind treatment period, the proportion of participants missing HbA1c measurements was approximately 12%. Sensitivity analyses were performed to verify that the missing data had no impact on the primary analysis. Finally, the SEED study detected hypoglycemia by self-monitoring of blood glucose and laboratory glucose testing as well as self-reported symptoms associated with hypoglycemia. If a patient experienced a mild decrease in blood glucose but no overt symptoms before the detection time point, hypoglycemia will not have been detected.
In conclusion, we report that dorzagliatin as monotherapy for the treatment of drug-naïve patients with T2D is safe and well tolerated. Dorzagliatin treatment resulted in significant improvement in glycemic control starting at treatment week 4. These improvements were maintained throughout the 24-week double-blind treatment period and were sustained during a 28-week open-label extension out to 52 weeks of treatment.
Methods
Trial design
The SEED trial had a 2-week screening period and a 4-week single-blind placebo run-in period, a 24-week double-blind placebo-controlled treatment period followed by an extended 28-week open-label treatment period, and a 1-week safety follow-up period (Extended Data Fig. 1).
Patients
Patients were recruited at the study site by investigators. The patients were required to sign an informed consent form before any study procedures or screening for eligibility. Patients were not paid for taking part in the study, but the patients were compensated for the travel to site and blood draw at the site. During the study, patients were paid for completing different procedures at each visit. If the patients suffer any trial-related injury during the trial period, they can receive treatment at study hospital, and the sponsor will cover the relevant medical costs as well as financial compensation as defined in the relevant laws and regulations of China. Individuals (18 to 75 years old) were included in the trial if they met the following criteria: diagnosis of T2D; undergoing a diet and exercise regimen for at least 3 months; no antidiabetic pharmacotherapy before screening; HbA1c levels between 7.5% and 11.0%; a BMI between 18.5 and 35.0 kg/m2 at screening; and willingness to provide written informed consent and comply with the study protocol.
Individuals were excluded if they met the following criteria: T2D medical history of more than 3 years when signing the informed consent form; treatment with any antidiabetic drugs for more than 14 d within 3 years before screening; severe hypoglycemia with no known cause within 3 months if hypoglycemia occurred three or more times within 1 month before screening; fasting C-peptide level of <1.0 ng ml−1 (normal range: 0.81–3.85 ng ml−1) at screening; history of diabetic ketoacidosis, diabetes lactic acidosis or hyperosmotic nonketotic diabetic coma; diagnosis of T1D. Other exclusion criteria were: major cardio-cerebrovascular diseases within 6 months before screening; unstable or rapidly progressive kidney disease; active liver diseases; psychiatric diseases; hemoglobinopathy; immunocompromised participants; any type of malignancy; unstable endocrine system diseases; history of drug abuse; received oral or injected corticosteroids treatment within 1 year at screening; alcohol intake >2 units a day or >14 units a week; ALT or AST > 2.5 times the upper limit of normal (ULN); or a serum total bilirubin level > 1.5 × ULN; serological evidence of hepatitis virus infection at screening; eGFR < 60 ml min−1/1.73m2; triglyceride level > 5.7 mmol l−1; anemia; and any accompanied diseases, treatment or participant status that may impede completion of the whole study or potentially affect the interpretation of efficacy and safety data.
Trial procedures
At week 3 of the 4-week run-in period, the patients were reevaluated before randomization to confirm eligibility. Eligibility criteria included HbA1c levels between 7.5% and 10.0% and FPG levels between 126.0 and 239.4 mg dl−1 at randomization. Diet and exercise counseling was provided throughout the study.
Patients were randomly assigned at a 2:1 ratio to receive dorzagliatin or placebo during the double-blind period. Randomization and drug dispensation were performed with an interactive web response system (IWRS; Medidata RAVE RTSM, v2020.1.1). A stratified randomization method with the permuted block randomization algorithm was used. The blocks were dynamically allocated to each site and stratum from the randomization list. A unique ID number was provided by the vendor and marked on the medication box. Using central randomization, randomization codes were assigned to eligible participants by the IWRS system based on stratification factors (baseline HbA1c level ≤ 8.5% or >8.5%) and the block size. During the double-blind treatment, the random allocation sequences were concealed from patients, investigators and other study members until week 24. All patients received dorzagliatin twice a day during 28-week open-label period. The blinding was maintained throughout the entire 52 weeks of treatment. The placebo tablets had the same size, color, odor and appearance as the investigational drug.
Efficacy endpoints
The primary efficacy endpoint was the change from baseline in the HbA1c level at week 24. Key secondary efficacy endpoints included the changes from baseline in 2h-PPG, FPG levels at week 24, HbA1c level at each visit (except week 24) and the percentage of patients who reached an HbA1c level of <7.0% at week 24. Additional efficacy endpoints included the composite endpoint (HbA1c level of <7.0% without hypoglycemia and no weight gain) as well as the change from baseline in HOMA2-β and HOMA2-IR. During the study, HbA1c and FPG levels were measured and evaluated at visits 4 to 15. At visits 4, 7, 10 and 15, 2h-PPG was measured by a standardized mixed-meal tolerance test (MMTT).
Safety endpoints
Safety assessments were completed at each study visit. Blood and urine were sampled at each visit. Adverse events and serious adverse events were assessed throughout the trial. Hypoglycemic episodes were classified according to the American Diabetes Association (ADA) definitions. Vital signs and clinical laboratory test results were assessed, and physical examinations were performed. All laboratory tests were conducted in the central laboratory. All samples were collected at the site.
Trial oversight
The trial was conducted in accordance with the principles of the Declaration of Helsinki, Good Clinical Practice guidelines, and laws and regulations in China. The study protocol was amended once during study enrollment. The important changes to the protocol are listed as follows, which mainly involve exclusion criteria and randomization criteria: exclude patients treated with any antidiabetic drugs within 3 months before screening; round original fasting C-peptide values to 1 decimal place; short-term external use of corticosteroids treatment within 1 year at screening was allowed and inhaled glucocorticoid treatment was forbidden; stable coronary heart disease was allowed; exclusion and randomization criteria related to blood pressure and antihypertensive drugs were redefined as systolic blood pressure ≥ 160 mm Hg or diastolic blood pressure ≥ 100 mm Hg at screening, or who added/changed antihypertensive drugs or adjusted dose within 4 weeks before screening; added electrocardiogram (ECG) examination at visit 3 and evaluation of ECG results to the randomization criteria; added a visit window period of ±3 d for visit 2 to match actual operational needs; added the 30-min testing point for the MMTT to optimize the study protocol; removed the rule that patients need not be in fasting status at visit 2; and clarified samples collected was blood sample in workflow. Minor protocol revisions involve wording, consistency and accuracy. The trial protocol and amendments were approved by the local ethics committees of all study sites: Affiliated Drum Tower Hospital, Medical School of Nanjing University, Nanjing, China; Zhongshan Hospital, Fudan University, Shanghai, China; Nanjing First Hospital, Nanjing, China; Jingzhou Hospital Affiliated to Yangtze University, Jingzhou, China; The First People’s Hospital of Changde City, Changde, China; Jinan Central Hospital Affiliated to Shandong First Medical University, Jinan, China; The First Hospital of Shanxi Medical University, Taiyuan, China; Zhuzhou Central Hospital, Zhuzhou, China; The Second Hospital of Jilin University, Changchun, China; Chenzhou First People’s Hospital, Chenzhou, China; Taihe Hospital, Hubei University of Medicine, Shiyan, China; Tongji Hospital of Tongji University, Shanghai, China; The First Affiliated Hospital of Anhui Medical University, Hefei, China; The Second Affiliated Hospital of Nanjing Medical University, Nanjing, China; Wuxi People’s Hospital, Wuxi, China; Changsha Central Hospital, Changsha, China; The First Hospital of Jilin University, Changchun, China; Affiliated Hospital of Jiangsu University, Zhenjiang, China; West China Hospital, Sichuan University, Chengdu, China; The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Jinan, China; The Affiliated Hospital of Qingdao University, Qingdao, China; Siping Hospital of China Medical University, Siping, China; The Affiliated Hospital of Guizhou Medical University, Guiyang, China; The 960th Hospital of the PLA Joint Logistics Support Force, Jinan, China; Southern Medical University Nanfang Hospital, Guangzhou, China; The First Affiliated Hospital and College of Clinical Medicine of Henan University of Science and Technology, Luoyang, China; PLA Rocket Force Characteristic Medical Center, Beijing, China; Sanya Central Hospital, Sanya, China; The Second Affiliated Hospital of Hainan Medical University, Haikou, China; Chongqing Red Cross Hospital, Chongqing, China; Chongqing University Three Gorges Central Hospital, Chongqing, China; Tianjin Medical University General Hospital, Tianjin, China; The Third Medical Center of PLA General Hospital, Beijing, China; Peking Union Medical College Hospital, Beijing, China; Tongji Hospital, Tongji Medical College of HUST, Wuhan, China; The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China; Jiangxi Pingxiang People’s Hospital, Pingxiang, China; The Second Hospital of Dalian Medical University, Dalian, China; The Third Affiliated Hospital, Sun Yat-sen University, Guangzhou, China; Xuzhou Central Hospital, Xuzhou, China; Shanghai Changzheng Hospital, Shanghai, China; and China-Japan Friendship Hospital, Beijing, China. Written informed consent was obtained from all patients before initiating any trial-related procedures. The trial was also conducted in accordance with the Chinese Diabetes Society guidelines, which require physicians to provide education and to strictly enforce improved exercise and dietary control as well as self-monitoring of blood glucose (at least twice per week) when treating patients with T2D.
Statistical analyses
We hypothesized that dorzagliatin would show superiority to placebo in decreasing HbA1c levels in patients after 24 weeks of treatment. For the primary endpoint HbA1c, we calculated that a total sample size of 450 patients would provide the trial with 91.4% power to detect a difference of 0.4% between the dorzagliatin group and the placebo group in a 2:1 ratio of allocation at a two-sided significance level of 0.05, assuming a standard deviation of 1.2%. The FAS included all randomized patients who received at least one dose of the study drug and had at least one posttreatment measurement of the primary endpoint during the double-blind treatment period. All major protocol deviations were reviewed in the blind-data-review meeting to determine whether a participant with any major protocol deviations should be excluded from the per-protocol set. The safety set included all randomized patients who received at least one dose of the study drug. Because this trial had only one confirmatory hypothesis test, that is, to test the null hypothesis of no difference in the primary endpoint between dorzagliatin and placebo, there was no adjustment for multiplicity.
The primary analysis method for the primary endpoint was in the FAS using an MMRM without missing-value imputation, which included treatment group, scheduled visit, the interaction of treatment group with the scheduled visit, pooled site and HbA1c baseline value as fixed effects. In the MMRM, data collected after initiation of prohibited antidiabetic medications were handled as missing data. The LS means of each treatment group, the ETD between dorzagliatin and placebo and its 95% CI were calculated. A sensitivity analysis was performed with the primary endpoint in the FAS using an ANCOVA with factors of treatment group, pooled site, interaction of treatment group with the pooled site (the interaction effect was removed if not significant on a two-sided alpha level of 0.1) and a covariate of HbA1c baseline value. In the ANCOVA model, missing values were imputed using the LOCF method, which was applied after excluding data collected after initiation of prohibited antidiabetic medications. Another sensitivity analysis was performed with the primary endpoint using the same MMRM in the per-protocol set.
The secondary efficacy endpoints, including 2h-PPG and FPG, were assessed using the same MMRM for the primary endpoint. Another secondary efficacy endpoint of the percentage of patients who reached an HbA1c level of <7.0% and an exploratory efficacy endpoint of the composite endpoint (HbA1c < 7.0% without hypoglycemia and no weight gain) were estimated based on the data imputed by the LOCF approach in the FAS. The OR and 95% CI between two treatment groups were estimated using the logistic regression model with categorical independent variables of the treatment group, pooled site, interaction of the treatment group with the pooled site (the interaction effect was removed from the model if not significant at a two-sided alpha level of 0.1) and a continuous independent variable of baseline HbA1c level. Another two exploratory efficacy endpoints of the change from baseline in the HOMA2-β and HOMA2-IR were analyzed using the ANCOVA model with factors of treatment group, pooled site, interaction of treatment group with the pooled site (the interaction effect was removed if not significant on a two-sided alpha level of 0.1) and baseline value of the analyzed variable. A post hoc analysis was conducted by using the Kaplan–Meier method to analyze the time to first reach an HbA1c level of <7.0% over 24 weeks. Furthermore, as a post hoc analysis to explore the in-group reduction in HbA1c from baseline at week 24 and week 52, paired t-tests based on observed measurements of HbA1c were carried out to compare baseline and week 24 or week 52 in each of dorzagliatin and placebo groups.
The incidence of treatment-emergent adverse events between the first intake of double-blind study drug and the seventh day after the last dose was summarized by the treatment group and compared between the two groups. The incidence of hypoglycemic events was also summarized by the treatment group and compared between treatment groups, including those spontaneously reported hypoglycemic events by patients and others reported at the on-site visit. The electronic data capture software (Medidata RAVE, Classic Rave v2018.2.4) was used for clinical trial patient data collection. Additional details regarding the statistical analysis are provided in the statistical analysis plan included in the Supplementary Information. Commercially available software (SAS v9.4, SAS Institute) was used for analyses.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data from analyses in the SEED study are not publicly available due to the sponsor’s contractual obligations. We encourage researchers or parties interested in collaboration for noncommercial use to submit an application to the corresponding authors (lichen@huamedicine.com). Applications should specifically outline the data the parties are interested in receiving and how the data will be used; the use of the data must also comply with the Human Genetics Resources Administration requirements of China and other country-specific or region-specific regulations. All shared data will be de-identified and will be made available 2 years after the date of publication. A signed data access agreement with the sponsor is required before accessing the shared data. The study protocol and statistical analysis plan are provided with the paper.
References
International Diabetes Federation. IDF Diabetes Atlas tenth edition (2021).
DeFronzo, R. A. Lilly lecture 1987. The triumvirate: beta cell, muscle, liver. A collusion responsible for NIDDM. Diabetes 37, 667–687 (1988).
Wang, L. et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317, 2515–2523 (2017).
Consortium, R. Lack of durable improvements in beta-cell function following withdrawal of pharmacological interventions in adults with impaired glucose tolerance or recently diagnosed type 2 diabetes. Diabetes Care 42, 1742–1751 (2019).
Basu, A. et al. Effects of type 2 diabetes on insulin secretion, insulin action, glucose effectiveness, and postprandial glucose metabolism. Diabetes Care 32, 866–872 (2009).
Rizza, R. A. Pathogenesis of fasting and postprandial hyperglycemia in type 2 diabetes: implications for therapy. Diabetes 59, 2697–2707 (2010).
Kahn, S. E. et al. Importance of early-phase insulin secretion to intravenous glucose tolerance in subjects with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 86, 5824–5829 (2001).
Schwartz, S. S. et al. The time is right for a new classification system for diabetes: rationale and implications of the beta-cell-centric classification schema. Diabetes Care 39, 179–186 (2016).
Chen, L. R&D Strategies for type 2 diabetes: elucidate the underlying pathology and improve the impaired organ functions. Prog. Pharm. Sci. 40, P161 (2016).
Wajchenberg, B. L. Beta-cell failure in diabetes and preservation by clinical treatment. Endocr. Rev. 28, 187–218 (2007).
Matschinsky, F. M. & Ellerman, J. E. Metabolism of glucose in the islets of Langerhans. J. Biol. Chem. 243, 2730–2736 (1968).
Matschinsky, F. M. & Wilson, D. F. The central role of glucokinase in glucose homeostasis: a perspective 50 years after demonstrating the presence of the enzyme in Islets of Langerhans. Front. Physiol. 10, 148 (2019).
Matschinsky, F. M. Assessing the potential of glucokinase activators in diabetes therapy. Nat. Rev. Drug Discov. 8, 399–416 (2009).
Matschinsky, F. M. Banting lecture 1995. A lesson in metabolic regulation inspired by the glucokinase glucose sensor paradigm. Diabetes 45, 223–241 (1996).
Agius, L. Glucokinase and molecular aspects of liver glycogen metabolism. Biochem. J. 414, 1–18 (2008).
Pino, M. F. et al. Glucokinase thermolability and hepatic regulatory protein binding are essential factors for predicting the blood glucose phenotype of missense mutations. J. Biol. Chem. 282, 13906–13916 (2007).
Raimondo, A. et al. Phenotypic severity of homozygous GCK mutations causing neonatal or childhood-onset diabetes is primarily mediated through effects on protein stability. Hum. Mol. Genet. 23, 6432–6440 (2014).
Matschinsky, F. M. Glucokinase, glucose homeostasis, and diabetes mellitus. Curr. Diab. Rep. 5, 171–176 (2005).
Froguel, P. et al. Familial hyperglycemia due to mutations in glucokinase. Definition of a subtype of diabetes mellitus. N. Engl. J. Med. 328, 697–702 (1993).
Glaser, B. et al. Familial hyperinsulinism caused by an activating glucokinase mutation. N. Engl. J. Med. 338, 226–230 (1998).
Heimberg, H. et al. The glucose sensor protein glucokinase is expressed in glucagon-producing alpha cells. Proc. Natl Acad. Sci. USA 93, 7036–7041 (1996).
Basco, D. et al. Alpha-cell glucokinase suppresses glucose-regulated glucagon secretion. Nat. Commun. 9, 546 (2018).
Moede, T. et al. Glucokinase intrinsically regulates glucose sensing and glucagon secretion in pancreatic alpha cells. Sci. Rep. 10, 20145 (2020).
Agius, L. Targeting hepatic glucokinase in type 2 diabetes: weighing the benefits and risks. Diabetes 58, 18–20 (2009).
Li, C. et al. Regulation of glucagon secretion in normal and diabetic human islets by gamma-hydroxybutyrate and glycine. J. Biol. Chem. 288, 3938–3951 (2013).
Haeusler, R. A. et al. Decreased expression of hepatic glucokinase in type 2 diabetes. Mol. Metab. 4, 222–226 (2015).
Jiang, M. H. et al. Hypermethylation of hepatic Gck promoter in ageing rats contributes to diabetogenic potential. Diabetologia 51, 1525–1533 (2008).
Basu, A. et al. Effects of type 2 diabetes on the ability of insulin and glucose to regulate splanchnic and muscle glucose metabolism: evidence for a defect in hepatic glucokinase activity. Diabetes 49, 272–283 (2000).
Basu, A. et al. Type 2 diabetes impairs splanchnic uptake of glucose but does not alter intestinal glucose absorption during enteral glucose feeding: additional evidence for a defect in hepatic glucokinase activity. Diabetes 50, 1351–1362 (2001).
Grimsby, J. et al. Allosteric activators of glucokinase: potential role in diabetes therapy. Science 301, 370–373 (2003).
Eiki, J. et al. Pharmacokinetic and pharmacodynamic properties of the glucokinase activator MK-0941 in rodent models of type 2 diabetes and healthy dogs. Mol. Pharmacol. 80, 1156–1165 (2011).
Sarabu, R. et al. Discovery of piragliatin–first glucokinase activator studied in type 2 diabetic patients. J. Med. Chem. 55, 7021–7036 (2012).
Vella, A. et al. Targeting hepatic glucokinase to treat diabetes with TTP399, a hepatoselective glucokinase activator. Sci. Transl. Med. 11, eaau3441 (2019).
Xu, H. et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of novel glucokinase activator HMS5552: results from a first-in-human single ascending dose study. Drug Des. Devel. Ther. 10, 1619–1626 (2016).
Ericsson, H. et al. Tolerability, pharmacokinetics, and pharmacodynamics of the glucokinase activator AZD1656, after single ascending doses in healthy subjects during euglycemic clamp. Int. J. Clin. Pharmacol. Ther. 50, 765–777 (2012).
Denney, W. S., Denham, D. S., Riggs, M. R. & Amin, N. B. Glycemic effect and safety of a systemic, partial glucokinase activator, PF-04937319, in patients with type 2 diabetes mellitus inadequately controlled on metformin—a randomized, crossover, active-controlled study. Clin. Pharmacol. Drug Dev. 5, 517–527 (2016).
Zhi, J. & Zhai, S. Effects of piragliatin, a glucokinase activator, on fasting and postprandial plasma glucose in patients with type 2 diabetes mellitus. J. Clin. Pharmacol. 56, 231–238 (2016).
Meininger, G. E. et al. Effects of MK-0941, a novel glucokinase activator, on glycemic control in insulin-treated patients with type 2 diabetes. Diabetes Care 34, 2560–2566 (2011).
Wilding, J. P., Leonsson-Zachrisson, M., Wessman, C. & Johnsson, E. Dose-ranging study with the glucokinase activator AZD1656 in patients with type 2 diabetes mellitus on metformin. Diabetes Obes. Metab. 15, 750–759 (2013).
Kiyosue, A., Hayashi, N., Komori, H., Leonsson-Zachrisson, M. & Johnsson, E. Dose-ranging study with the glucokinase activator AZD1656 as monotherapy in Japanese patients with type 2 diabetes mellitus. Diabetes Obes. Metab. 15, 923–930 (2013).
Amin, N. B. et al. Two dose-ranging studies with PF-04937319, a systemic partial activator of glucokinase, as add-on therapy to metformin in adults with type 2 diabetes. Diabetes Obes. Metab. 17, 751–759 (2015).
Katz, L. et al. AMG 151 (ARRY-403), a novel glucokinase activator, decreases fasting and postprandial glycaemia in patients with type 2 diabetes. Diabetes Obes. Metab. 18, 191–195 (2016).
Zhi, J. et al. A novel glucokinase activator RO4389620 improved fasting and postprandial plasma glucose in type 2 diabetic patients. Diabetologia 51, S23 (2008).
Zhai, S., Georgy, A., Liang, Z. & Zhi, J. Pharmacokinetic and pharmacodynamic drug interaction study of piragliatin, a glucokinase activator, and glyburide, a sulfonylurea, in type 2 diabetic patients. Clin. Pharmacol. Drug Dev. 5, 552–556 (2016).
Zheng, S. et al. Safety, pharmacokinetics, and pharmacodynamics of globalagliatin, a glucokinase activator, in chinese patients with type 2 diabetes mellitus: a randomized, phase ib, 28-day ascending dose study. Clin. Drug Investig. 40, 1155–1166 (2020).
Scheen, A. J. New hope for glucokinase activators in type 2 diabetes? Lancet Diabetes Endocrinol. 6, 591–593 (2018).
Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin. J. Diabetes Mellitus 13, 315–409 (2021).
Zhu, D. et al. Dorzagliatin monotherapy in Chinese patients with type 2 diabetes: a dose-ranging, randomised, double-blind, placebo-controlled, phase 2 study. Lancet Diabetes Endocrinol. 6, 627–636 (2018).
Klein, K. R. et al. The SimpliciT1 study: a randomized, double-blind, placebo-controlled phase 1b/2 adaptive study of TTP399, a hepatoselective glucokinase activator, for adjunctive treatment of type 1 diabetes. Diabetes Care 44, 960–968 (2021).
McCafferty, K. et al. ARCADIA study protocol: a phase II, randomised, double-blind, placebo-controlled clinical trial to assess the safety and efficacy of AZD1656 in patients with diabetes hospitalised with suspected or confirmed COVID-19. BMJ Open 11, e049650 (2021).
Wang, P. et al. Effects of a novel glucokinase activator, HMS5552, on glucose metabolism in a rat model of type 2 diabetes mellitus. J. Diabetes Res. 2017, 5812607 (2017).
Zhu, X. X. et al. Dorzagliatin (HMS5552), a novel dual-acting glucokinase activator, improves glycaemic control and pancreatic β-cell function in patients with type 2 diabetes: a 28-day treatment study using biomarker-guided patient selection. Diabetes Obes. Metab. 20, 2113–2120 (2018).
Zhu, D. L. et al. Clinically differentiated glucokinase activator HMS5552: effective control of 24-hour glucose and improvement of beta cell function in T2DM patients. Diabetes https://doi.org/10.2337/db15-932-1471 (2015).
Chen, L., Shan, Y., Jin, X. & Lv, X. Dorzagliatin differentiates from early generation of glucokinase activators: an enzyme kinetics study. Diabetes 68, 1151-P (2019).
Davis, E. A. et al. Mutants of glucokinase cause hypoglycaemia- and hyperglycaemia syndromes and their analysis illuminates fundamental quantitative concepts of glucose homeostasis. Diabetologia 42, 1175–1186 (1999).
NCT05102149: Study to evaluate the safety and efficacy of PB-201 in treatment-naive patients with type 2 diabetes mellitus. https://www.clinicaltrials.gov/ct2/show/NCT05102149 (2021).
Chen, L., Zhang, J., Yang, R. & Feng, L. Glucokinase activator dorzagliatin (HMS5552) regulates GLP-1 release in T2D patients and is synergistic with sitagliptin and empagliflozin in optimizing beta-cell function. Diabetes 70, 117-LB (2021).
Miao, J. et al. Effect of renal impairment on the pharmacokinetics and safety of dorzagliatin, a novel dual-acting glucokinase activator. Clin. Transl. Sci. 15, 548–557 (2021).
DAWN Study Group. Dorzagliatin add-on therapy to metformin in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, phase 3 trial. Nat. Med. (2022) (in press).
MedDRA Maintenance and Support Services Organization. Introductory Guide to MedDRA version 23.0 (March 2020). https://www.meddra.org/how-to-use/support-documentation
Acknowledgements
This study was sponsored by Hua Medicine. We thank J. Chen for medical writing and editing support, funded by Hua Medicine; L. Li, C. Geng and L. Yuan (Hua Medicine) for assistance with the efficacy data; A. Wang (Hua Medicine) for assistance with the safety data; X. Liu (Hua Medicine) for assistance with the statistical analyses; and G. Yu and F. Tang, who reviewed an earlier version of the manuscript on behalf of Hua Medicine. Hua Medicine participated in the design, conduct and data analysis and interpretation of the clinical study, the preparation of the manuscript, and were involved in making the decision to publish. The study was also funded in part, by grants from the National Major Scientific and Technological Special Project for Significant New Drug Development (2014ZX09101002004 and 2018ZX09711002–012–001), the Shanghai Science and Technology Innovation Action Project (14431908300, 15XD1520500, 17DZ1910200 and 19431905200), the Shanghai Pudong District Science and Technology Innovation Action Project (PKJ2014-S06) and the Shanghai Municipal Commission of Economy and Informatization Innovation Action Project (XC-ZXSJ-01-2015-02 and 18XI-18).
Author information
Authors and Affiliations
Contributions
D.Zhu and L.Chen led the design, conduct and analysis of the clinical study and the development of the manuscript. X.Li and W.Yang contributed to the protocol design, data analysis and manuscript draft as the study consultants. The trial was designed and overseen by representatives of Hua Medicine with input from selected site investigators. The site investigators collected the data, and the sponsor performed the data analyses. All of the authors interpreted the data and vouched for its accuracy and completeness and the fidelity of the trial to the protocol. The first author wrote the first draft of the manuscript with assistance from an independent medical writer funded by the sponsor. The manuscript was subsequently revised and approved by all authors, who agreed to submit the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
L.Chen, Y. Zhao and Y. Zhang are employees of Hua Medicine. D.Zhu, X.Li and W.Yang served on the Diabetes Advisory Board for Hua Medicine. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Victor Volovici, Naveed Sattar and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Jennifer Sargent and Joao Monteiro, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
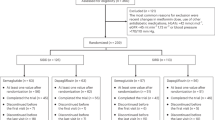
Extended Data Fig. 1 SEED trial design.
The SEED trial design was shown in the Extended Data Fig. 1, in which it showed the process of T2D patients completing the SEED study. Selected drug naive T2D patients entered into a 4 week single-blinded placebo run-in period followed by a randomization into a 24-week double blinded placebo controlled treatment to evaluate the primary efficacy and safety endpoints. Upon completion of the double blinded period, patients entered into an open-label 28 week treatment to evaluate drug safety endpoints, followed by a 1-week end of study follow-up.
Supplementary information
Supplementary Information
Supplementary Tables 1–10, clinical study protocol and statistical analysis plan
Rights and permissions
About this article
Cite this article
Zhu, D., Li, X., Ma, J. et al. Dorzagliatin in drug-naïve patients with type 2 diabetes: a randomized, double-blind, placebo-controlled phase 3 trial. Nat Med 28, 965–973 (2022). https://doi.org/10.1038/s41591-022-01802-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-01802-6
This article is cited by
-
Analyzing the changing trend of corneal biomechanical properties under different influencing factors in T2DM patients
Scientific Reports (2024)
-
Immunomodulation and immunopharmacology in heart failure
Nature Reviews Cardiology (2024)
-
Should Glucokinase be Given a Chance in Diabetes Therapeutics? A Clinical-Pharmacological Review of Dorzagliatin and Lessons Learned So Far
Clinical Drug Investigation (2024)
-
Diabetic vascular diseases: molecular mechanisms and therapeutic strategies
Signal Transduction and Targeted Therapy (2023)
-
A phase I open-label clinical trial to study drug-drug interactions of Dorzagliatin and Sitagliptin in patients with type 2 diabetes and obesity
Nature Communications (2023)