Abstract
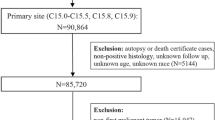
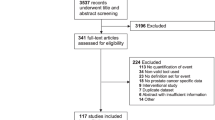
Despite substantial progress in cancer therapy in recent decades, patients with cancer remain at high suicide risk. Data from individual studies have not been comprehensively quantified and specific risk factors are ill-defined. We assessed suicide mortality risk according to cancer prognosis, stage, time since diagnosis, gender, ethnicity, marital status, year of recruitment and geographic region. We searched EMBASE, MEDLINE, PsycINFO, Web of Science, CINAHL and Google Scholar for relevant articles up to February 2021. We used a random effects model, performed meta-regression meta-analysis and assessed heterogeneity and publication bias using I², funnel plots and Egger’s and Begg’s tests. We performed a systematic review including 62 studies and 47,035,065 patients. To avoid patient sample overlap, the meta-analysis was performed on 28 studies, involving 22,407,690 patients with cancer. Suicide mortality was significantly increased compared with the general population (standardized mortality ratio = 1.85, 95% confidence interval = 1.55–2.20). Risk was strongly related to cancer prognosis, cancer stage, time since diagnosis and geographic region. Patients with cancer, particularly those with specific risk factors, should be closely monitored for suicidality and need specialized care to reduce short- and long-term risks of suicide.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data in the published article (and its Supplementary Information) have been presented where possible in aggregated form. Data from primary studies are publicly available within the databases listed in Supplementary Information. The datasets generated and/or analyzed during the current study are available from C.S. (by mail at Corinna.Seliger-Behme@med.uni-heidelberg.de) upon reasonable request as part of a scientific collaboration with adherence to standards of good scientific practice, although restrictions may apply due to privacy reasons and ongoing research projects. Data sharing will require a Materials Transfer Agreement (MTA) and is limited to noncommercial use. Requests will be answered within 4 weeks.
Code availability
All codes were adapted using R software, v.4.0.2 and v.4.1.1. Data sheets were created using Microsoft Excel v.16.57. The codes that support the findings of this study are available from the corresponding author (C.S.) (by mail at Corinna.Seliger-Behme@med.uni-heidelberg.de) upon reasonable request as part of a scientific collaboration with adherence to standards of good scientific practice, although restrictions may apply due to privacy reasons and ongoing research projects. Data sharing will require an MTA and is limited to noncommercial use. Requests will be answered within 4 weeks.
Change history
20 March 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41591-023-02307-6
References
Fitzmaurice, C. et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 5, 1749–1768 (2019).
Carlson, L.E. Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. J. Psychosoc. Oncol. 37, 5–21 (2019).
Visser, M. R. & Smets, E. M. Fatigue, depression and quality of life in cancer patients: how are they related? Support Care Cancer 6, 101–108 (1998).
World Health Organization. Mental health. Suicide data. https://www.who.int/news-room/fact-sheets/detail/suicide (accessed 14 January 2020).
Filiberti, A. et al. Characteristics of terminal cancer patients who committed suicide during a home palliative care program. J. Pain. Symptom Manag. 22, 544–553 (2001).
Cordova, M. J., Riba, M. B. & Spiegel, D. Post-traumatic stress disorder and cancer. Lancet Psychiatry 4, 330–338 (2017).
Shepard, D. S., Gurewich, D., Lwin, A. K., Reed, G. A. Jr. & Silverman, M. M. Suicide and suicidal attempts in the United States: costs and policy implications. Suicide Life Threat. Behav. 46, 352–362 (2016).
Henson, K. E. et al. Risk of suicide after cancer diagnosis in England. JAMA Psychiatry 21, 21 (2018).
Allebeck, P., Bolund, C. & Ringback, G. Increased suicide rate in cancer patients. A cohort study based on the Swedish Cancer-Environment Register. J. Clin. Epidemiol. 42, 611–616 (1989).
Muff Christensen, M. L., Yousaf, U., Engholm, G. & Storm, H. H. Increased suicide risk among Danish women with non-melanoma skin cancer, 1971–1999. Eur. J. Cancer Prev. 15, 266–268 (2006).
Crocetti, E., Arniani, S., Acciai, S., Barchielli, A. & Buiatti, E. High suicide mortality soon after diagnosis among cancer patients in central Italy. Br. J. Cancer 77, 1194–1196 (1998).
Dormer, N. R., McCaul, K. A. & Kristjanson, L. J. Risk of suicide in cancer patients in Western Australia, 1981–2002. Med. J. Aust. 188, 140–143 (2008).
Hem, E., Loge, J. H., Haldorsen, T. & Ekeberg, O. Suicide risk in cancer patients from 1960 to 1999. J. Clin. Oncol. 22, 4209–4216 (2004).
Innos, K., Rahu, K., Rahu, M. & Baburin, A. Suicides among cancer patients in Estonia: a population-based study. Eur. J. Cancer 39, 2223–2228 (2003).
Levi, F., Bulliard, J. L. & La Vecchia, C. Suicide risk among incident cases of cancer in the Swiss Canton of Vaud. Oncology 48, 44–47 (1991).
Misono, S., Weiss, N. S., Fann, J. R., Redman, M. & Yueh, B. Incidence of suicide in persons with cancer. J. Clin. Oncol. 26, 4731–4738 (2008).
Robinson, D., Renshaw, C., Okello, C., Moller, H. & Davies, E. A. Suicide in cancer patients in South East England from 1996 to 2005: a population-based study. Br. J. Cancer 101, 198–201 (2009).
Schairer, C. et al. Suicide after breast cancer: an international population-based study of 723,810 women. J. Natl Cancer Inst. 98, 1416–1419 (2006).
Tanaka, H. et al. Suicide risk among cancer patients: experience at one medical center in Japan, 1978–1994. Jpn. J. Cancer Res. 90, 812–817 (1999).
Yousaf, U., Christensen, M. L., Engholm, G. & Storm, H. H. Suicides among Danish cancer patients 1971–1999. Br. J. Cancer 92, 995–1000 (2005).
Ahn, M. H., Park, S., Lee, H. B., Ramsey, C. M. & Na, R. Suicide in cancer patients within the first year of diagnosis. Psycho-Oncology 24, 601–607 (2015).
Ravaioli, A. et al. Suicide death among cancer patients: new data from northern Italy, systematic review of the last 22 years and meta-analysis. Eur. J. Cancer 125, 104–113 (2020).
Amiri, S. & Behnezhad, S. Cancer diagnosis and suicide mortality: a systematic review and meta-analysis. Arch. Suicide Res. 24, S94–S112 (2020).
Du, L. et al. Incidence of suicide death in patients with cancer: a systematic review and meta-analysis. J. Affect. Disord. 276, 711–719 (2020).
Harris, E. C. & Barraclough, B. M. Suicide as an outcome for medical disorders. Medicine 73, 281–296 (1994).
Brunckhorst, O. et al. Depression, anxiety, and suicidality in patients with prostate cancer: a systematic review and meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 24, 281–289 (2021).
Guo, Z. et al. Incidence and risk factors of suicide among patients diagnosed with bladder cancer: a systematic review and meta-analysis. Urol. Oncol. 39, 171–179 (2020).
Lunny, C., Pieper, D., Thabet, P. & Kanji, S. Managing overlap of primary study results across systematic reviews: practical considerations for authors of overviews of reviews. BMC Med. Res. Method. 21, 140 (2021).
SEER*Explorer: An interactive website for SEER cancer statistics (National Cancer Institute, 2021). https://seer.cancer.gov/explorer.
Roser, M. & Ritchie, H. Cancer (OurWorldInData.org, 2015).
Cancer Resaearch UK. Head and neck cancers survival statistics (Cancer Research UK, 2021).
de Kock, S. et al. Systematic review search methods evaluated using the Preferred Reporting of Items for Systematic Reviews and Meta-Analyses and the Risk Of Bias In Systematic reviews tool. Int. J. Technol. Assess. Health Care 37, e18 (2020).
Allebeck, P. & Bolund, C. Suicides and suicide attempts in cancer patients. Psychol. Med. 21, 979–984 (1991).
Kaceniene, A., Krilaviciute, A., Kazlauskiene, J., Bulotiene, G. & Smailyte, G. Increasing suicide risk among cancer patients in Lithuania from 1993 to 2012: a cancer registry-based study. Eur. J. Cancer Prev. 26, S197–S203 (2017).
Saad, A. M. et al. Suicidal death within a year of a cancer diagnosis: a population-based study. Cancer 125, 972–979 (2019).
Heikkinen, M., Aro, H. & Lönnqvist, J. Recent life events, social support and suicide. Acta Psychiatr. Scand. Suppl. 377, 65–72 (1994).
Zebrack, B. J. et al. Psychological distress and unsatisfied need for psychosocial support in adolescent and young adult cancer patients during the first year following diagnosis. Psycho-Oncology 23, 1267–1275 (2014).
Klaassen, Z. et al. Factors associated with suicide in patients with genitourinary malignancies. Cancer 121, 1864–1872 (2015).
DeNavas-Walt, C., Proctor, B.D. & Smith, J.C. Income, poverty, and health insurance coverage in the United States: 2010. in Current Population Reports (US Census Bureau, 2011).
Jones, G. & Kantarjian, H. The many roads to universal health care in the USA. Lancet Oncol. 20, e601–e605 (2019).
Rehkopf, D. H. & Buka, S. L. The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. Psychol. Med. 36, 145–157 (2006).
Wolfe, A. The pursuit of autonomy. The New York Times Magazine. https://archive.nytimes.com/www.nytimes.com/library/magazine/home/2000050mag-introduction.html (2000).
Centers for Disease Control and Prevention. Suicide and Self-Harm Injury (CDC/National Center for Health Statistics, 2021).
Ritchie, H., Roser, M. & Ortiz-Ospina, E. Deaths—Self-harm by firearm (Global Burden of Disease Collaborative Network, 2017).
Massetti, G. M., Holland, K. M., Jack, S. P. D., Ragan, K. R. & Lunsford, N. B. Circumstances of suicide among individuals with a history of cancer. Psycho-Oncology 27, 1750–1756 (2018).
Rockett, I. R., Samora, J. B. & Coben, J. H. The black–white suicide paradox: possible effects of misclassification. Soc. Sci. Med 63, 2165–2175 (2006).
Gibbs, J. T. African–American suicide: a cultural paradox. Suicide Life Threat. Behav. 27, 68–79 (1997).
Utsey, S. O., Hook, J. N. & Stanard, P. A re-examination of cultural factors that mitigate risk and promote resilience in relation to African American suicide: a review of the literature and recommendations for future research. Death Stud. 31, 399–416 (2007).
Volkers, N. In coping with cancer, gender matters. J. Natl Cancer Inst. 91, 1712–1714 (1999).
Mann, J. J. et al. Suicide prevention strategies: a systematic review. JAMA 294, 2064–2074 (2005).
Klaassen, Z. et al. Cancer diagnosis and risk of suicide after accounting for prediagnosis psychiatric care: a matched-cohort study of patients with incident solid-organ malignancies. Cancer 125, 2886–2895 (2019).
Smailyte, G. et al. Suicides among cancer patients in Lithuania: a population-based census-linked study. Cancer Epidemiol. 37, 714–718 (2013).
Smith, D. P. et al. Increased risk of suicide in New South Wales men with prostate cancer: analysis of linked population-wide data. PLoS ONE 13, e0198679 (2018).
Beauplet, B. et al. Dealing with the lack of evidence to treat depression in older patients with cancer: French Societies of Geriatric Oncology (SOFOG) and PsychoOncology (SFFPO) position paper based on a systematic review. Support Care Cancer 29, 563–571 (2021).
Ostuzzi, G., Matcham, F., Dauchy, S., Barbui, C. & Hotopf, M. Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst. Rev. 4, CD011006 (2018).
Boudreaux, E. D. et al. Improving suicide risk screening and detection in the emergency department. Am. J. Prev. Med. 50, 445–453 (2016).
Kim, S., Lee, H. K. & Lee, K. Which PHQ-9 items can effectively screen for suicide? Machine learning approaches. Int. J. Environ. Res. Public Health 18, 3339 (2021).
Angermeyer, M. C., van der Auwera, S., Carta, M. G. & Schomerus, G. Public attitudes towards psychiatry and psychiatric treatment at the beginning of the 21st century: a systematic review and meta-analysis of population surveys. World Psychiatry 16, 50–61 (2017).
Cavanagh, J. T., Carson, A. J., Sharpe, M. & Lawrie, S. M. Psychological autopsy studies of suicide: a systematic review. Psychol. Med. 33, 395–405 (2003).
Luoma, J. B., Martin, C. E. & Pearson, J. L. Contact with mental health and primary care providers before suicide: a review of the evidence. Am. J. Psychiatry 159, 909–916 (2002).
Flüchter, P., Müller, V. & Pajonk, F. G. [Suicidality: procedure in emergency cases]. Med Klin. Intensivmed. Notfmed. 107, 469–475 (2012).
Polanczyk, G. V. Many reasons to talk about suicide. Rev. Assoc. Med Bras. (1992) 63, 557–558 (2017).
McGowan, J. et al. PRESS peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. 75, 40–46 (2016).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 3, e123–e130 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000).
Rethlefsen, M. L. et al. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst. Rev. 10, 39 (2021).
World Health Organization. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization (1992).
Wells G. et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2011).
Acknowledgements
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
M.H. was responsible for conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, validation, visualization and writing (original draft and writing, review and editing). L.H. was responsible for conceptualization, data curation, investigation, resources and writing (review and editing). H.J. was responsible for conceptualization, data curation, formal analysis, investigation, methodology, resources, software, supervision, validation, visualization and writing (review and editing). P.K. was responsible for conceptualization and writing (review and editing). H.K. performed conceptualization, investigation, resources and writing (review and editing). M.L. was responsible for conceptualization, methodology, supervision and writing (review and editing). C.S. performed conceptualization, investigation, methodology, resources, project administration, supervision, validation and writing (review and editing).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Cristiane Decat Bergerot and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Javier Carmona was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Forest plot of individual cancer sites of all studies included in the (A) systematic review and (B) meta-analysis, by magnitude of risk estimate.
ISR2 = 98.86% and IMA2 = 99.03%, P-heterogeneity<0.0001. Abbreviations: SMR, standardized mortality ratio; CI, confidence interval; ISR2, I2-statistic for systematic review; IMA2, I2-statistic for meta-analysis. Squares depict SMR point estimates and error bars their corresponding 95% confidence intervals.
Extended Data Fig. 2 Forest plot of random effects meta-analysis including 62 cohort studies of suicide in cancer patients extracted from all databases.
Studies are listed by magnitude of risk estimate and weighted by their contribution to the summary risk estimate. I2 = 99.55%, P-heterogeneity<0.0001. Abbreviations: SMR, standardized mortality ratio; CI, confidence interval; MF, men and women combined; M, men only; F, women only; RE, risk estimate. Squares depict SMR point estimates and error bars their corresponding 95% confidence intervals.
Extended Data Fig. 3 Summary forest plot of cancer sites, by prognosis based on 62 studies.
Good prognosis was defined as a 5-year survival rate of >90%; medium prognosis was defined as a 5-year survival rate of 50–90%; poor prognosis was defined as a 5-year survival rate of <50%. I2 = 99.00%, P-heterogeneity<0.0001. Abbreviations: SMR, standardized mortality ratio; CI, confidence interval; n, number of studies included in the analysis; cancer sites with n = 1 were not included in the analysis.
Extended Data Fig. 4 Summary forest plot of subgroup analyses of suicide in patients with cancer based on 62 studies.
Abbreviations: SMR, standardized mortality ratio; CI, confidence interval; n, number of studies included in the analysis.
Extended Data Fig. 5 Funnel plot of random effects meta-analysis including 62 risk estimates of suicide in cancer patients.
Two-sided P-value for Begg’s test = 0.42; Two-sided P-value for Egger’s test = 0.4239.
Extended Data Fig. 6 Suicide rates in the general population of countries included in the present meta-analysis, except Taiwan (data not available).
Data presented by country, from 1950 to 2005.
Supplementary information
Supplementary Information
Supplementary Subjects and Methods, Tables 1–6 and References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heinrich, M., Hofmann, L., Baurecht, H. et al. Suicide risk and mortality among patients with cancer. Nat Med 28, 852–859 (2022). https://doi.org/10.1038/s41591-022-01745-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-01745-y
This article is cited by
-
Avoiding lead-time bias by estimating stage-specific proportions of cancer and non-cancer deaths
Cancer Causes & Control (2024)
-
Mitigating long-term and delayed adverse events associated with cancer treatment: implications for survivorship
Nature Reviews Clinical Oncology (2023)
-
Exploring the unseen threat: the neglect of suicide risk in people with cancer
Nature Mental Health (2023)
-
Suicide risk in cancer patients: cancer prognosis and mental health
Supportive Care in Cancer (2023)
-
Suicide risk among adolescents and young adults after cancer diagnosis: analysis of 34 cancer groups from 2009 to 2019
Journal of Cancer Survivorship (2023)