Abstract
The identity of histocompatibility loci, besides human leukocyte antigen (HLA), remains elusive. The major histocompatibility complex (MHC) class I MICA gene is a candidate histocompatibility locus. Here, we investigate its role in a French multicenter cohort of 1,356 kidney transplants. MICA mismatches were associated with decreased graft survival (hazard ratio (HR), 2.12; 95% confidence interval (CI): 1.45–3.11; P < 0.001). Both before and after transplantation anti-MICA donor-specific antibodies (DSA) were strongly associated with increased antibody-mediated rejection (ABMR) (HR, 3.79; 95% CI: 1.94–7.39; P < 0.001; HR, 9.92; 95% CI: 7.43–13.20; P < 0.001, respectively). This effect was synergetic with that of anti-HLA DSA before and after transplantation (HR, 25.68; 95% CI: 3.31–199.41; P = 0.002; HR, 82.67; 95% CI: 33.67–202.97; P < 0.001, respectively). De novo-developed anti-MICA DSA were the most harmful because they were also associated with reduced graft survival (HR, 1.29; 95% CI: 1.05–1.58; P = 0.014). Finally, the damaging effect of anti-MICA DSA on graft survival was confirmed in an independent cohort of 168 patients with ABMR (HR, 1.71; 95% CI: 1.02–2.86; P = 0.041). In conclusion, assessment of MICA matching and immunization for the identification of patients at high risk for transplant rejection and loss is warranted.
Similar content being viewed by others
Main
Kidney transplantation is the only curative treatment for end-stage renal disease1. The fact that the first successful kidney transplantation in man was between identical twins2, along with seminal work in animal models, hinted strongly that a single genetic locus does not govern the clinical outcome of a transplantation, no matter how relevant (such as the major histocompatibility complex (MHC), human leukocyte antigen (HLA)). Indeed, George Snell, in his landmark 1948 study3 (as well as subsequent work by himself, and others), identified several dozen histocompatibility loci in the mouse4, although close to none has been identified to date in any species (including man).
Fast forward to today, and, owing to the development and refinement of country- and continent-wide allocation processes, perioperative handling of the graft and patients, and selective immunosuppressive drugs that improve transplantation survival mainly by alleviating acute T cell-mediated rejection (TCMR), the number of kidney transplantations is continuously increasing worldwide. However, antibody-mediated rejection (ABMR) is recognized as a major cause of late transplantation failure, and its treatment remains challenging5. In addition to the histological findings, a key feature of ABMR is the presence of donor-specific anti-HLA antibodies (DSA)6. Nonetheless, in routine clinical care, cases meeting the histological criteria for ABMR but without detectable anti-HLA DSA could represent more than 50% of rejection events7. These cases might be explained by the presence of pathogenic antibodies that are produced against other, non-HLA, histocompatibility antigens8.
MHC class I chain-related gene A (MICA; GenBank accession: NM_001177519), discovered almost 30 years ago9, encodes a polymorphic non-conventional MHC-encoded class I molecule10. The MICA gene is located, within the HLA complex, 46 kb centromeric to the HLA-B locus9. Close to 400 MICA alleles have been reported to date10. The MICA glycoprotein (Uniprot accession: Q96QC4) is expressed on a restricted number of cell types, mainly epithelial and endothelial cells. MICA binds NKG2D, an activating receptor present on the surface of cytotoxic CD8+ αβ and γδ T lymphocytes as well as certain natural killer (NK) cells10.
Fifteen years ago Zou et al.11 reported the first comprehensive study of the potential involvement of MICA in kidney transplant outcomes. That work, however, was focused only on anti-MICA antibodies and had no information on donor and recipient MICA (mis)matching, a situation that has persisted to date given that no study has analyzed simultaneously the sequence-based molecular MICA matching and the status of both anti-HLA and anti-MICA DSA in a large cohort for which information about all other relevant covariates was available and included in the final analysis (for review see refs. 12,13).
Here, we evaluate the role of MICA matching and donor-specific MICA immunization in a retrospective multicenter French cohort of 1,356 patients who had undergone kidney transplantation. All known covariates relevant to graft failure and acute rejection were considered in the analysis. The results highlight the relevance of both MICA matching and donor-specific immunization for kidney transplantation outcomes.
Results
Baseline characteristics of kidney transplant recipients
The main analysis involved 1,356 patients who underwent kidney transplantation in six French medical centers between 2002 and 2011: 104 in Montpellier, 107 in Paris-Saint-Louis, 188 in Toulouse, 262 in Paris-Necker, 304 in Nancy and 391 in Nantes. The demographics of this study population are listed in Table 1. Most patients were recipients of their first transplant (95%). One hundred and two patients received organs from living donors and 9% of patients received simultaneous kidney–pancreas transplantations. All but two of the relevant covariates for the clinical outcomes analyzed were equally distributed in the MICA-matched and -mismatched patients. There were more retransplantations in the MICA-matched than in the MICA-mismatched groups (10% versus 5%, P = 0.04), and MICA-mismatched transplantations had more HLA mismatches (P < 0.001, P < 0.001 and P = 0.01 for HLA-A, -B and -DRB1 mismatches, respectively; Table 1); both observations are probably due to linkage disequilibrium between MICA and HLA-B.
MICA matching and graft survival
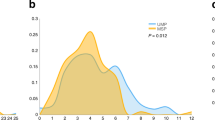
The median follow-up after transplantation was 6.3 years, with a maximum of 12.9 years. The median follow-up was 6.5 and 6.3 years for the MICA-matched and -mismatched patients, respectively. A total of 192 patients (14.2%) had graft failure during follow-up; 1,208 patients (89.1%) survived. Compared with MICA-mismatched patients, MICA-matched patients had a significantly improved graft survival rate (Plog-rank = 0.017), which was the primary endpoint of the study (Fig. 1a). At 5 years after transplantation, graft survival was 96% and 88% for MICA-matched and -mismatched patients, respectively, and this difference in survival rate was also observed when comparing the different mismatching possibilities at the MICA locus (0 versus 1 versus 2 mismatches, Plog-rank = 0.008) (Fig. 1b). The most important impact on graft survival was observed for the case of two mismatches, with rates of 87% and 76% at 5 and 10 years after transplantation, respectively. Based on multivariate Cox regression, MICA mismatching was an independent factor associated with graft loss (HR, 2.12; 95% CI: 1.45–3.11; P < 0.001). Other independent risk factors in the model included age of the donor and recipient, dialysis duration, initial nephropathy, older transplantations, delayed graft function and absence of induction treatment (Table 2). HLA-A, -B and -DRB1 mismatching at a low level of resolution had no impact on graft failure (Extended Data Table 1).
The probability of graft survival is shown for matched versus mismatched patients using the presence or absence of mismatches at the MICA locus (a) or the number of mismatches (b) as classification criteria. P values were determined using the two-sided log-rank test without correction.
To exclude potential bias due to the difference in the resolution of MICA and HLA genotypes, we analyzed a subset of 862 transplants in which both donor and recipient were retrospectively HLA-typed at second-field resolution, which corresponds to allele-level resolution of MICA typing. Multivariate analysis confirmed the HLA-independent association of MICA mismatches with a higher incidence of graft loss (HR, 1.53; 95% CI: 1.07–2.19; P = 0.018; Extended Data Table 2). Other risk factors for graft loss in the model included age of the donor and recipient, dialysis duration, initial nephropathy, pre-transplantation anti-HLA DSA, number of transplantations, absence of induction treatment, depleting induction treatment and HLA-DQB1 mismatches (Extended Data Table 2). We also confirmed the HLA-B-independent effect of MICA by analyzing HLA-B-matched transplantations in this subset of transplants (n = 33), in which MICA mismatches were still associated with lower graft survival (Plog-rank = 0.015, Extended Data Fig. 1).
Finally, MICA eplet mismatches had a similar association with graft loss, but did not reach statistical significance (Plog-rank = 0.11, Supplementary Fig. 1).
Impact of preformed anti-MICA DSA on graft outcome
Although there is no functional analogy between HLA and MICA molecules, however, to establish whether the observed lower graft survival associated with donor–recipient MICA mismatches might be explained by immunization against MICA (similarly to the situation between HLA mismatches and anti-HLA DSA), we analyzed the pre-transplant sera of 524 patients for the presence of anti-MICA DSA. In this subset of patients, the median follow-up was 5.80 years (with a maximum at 9.58 years) in those with anti-MICA DSA, and 6.04 years (with a maximum at 10.09 years) in those without anti-MICA DSA (Supplementary Table 1). Given that acute rejection is a major cause of kidney transplantation failure (HR, 2.64; 95% CI: 2.15–3.25; P < 0.001, Extended Data Table 3), we assessed whether donor-specific immunization against MICA had a role in this clinical event, which was the secondary endpoint of the study. Acute clinical rejection developed in 77 patients: TCMR in 52 (9.9%) and ABMR in 35 (6.7%), and of those 10 were mixed-type rejections (1.9%). The presence of anti-MICA DSA was found to be an independent risk factor for acute rejection, with a borderline but significant effect on TCMR (HR, 2.11; 95% CI: 1.01–4.42; P = 0.047) and a more important effect on ABMR (HR, 3.79; 95% CI: 1.94–7.39; P < 0.001; Fig. 2a and Table 3). Preformed anti-MICA DSA were not associated with graft loss (HR, 1.32; 95% CI: 0.82–2.10; P = 0.25; Table 3). The association of eplet-specific anti-MICA DSA with ABMR was similar to that of all anti-MICA DSA (Supplementary Fig. 2 and Extended Data Table 4).
The cumulative incidence of antibody-mediated rejection is shown for patients with versus those without preformed anti-MICA DSA (a) and for patients with versus those without anti-MICA DSA 1 year after transplantation (b). P values were determined using the two-sided log-rank test without correction.
One year post-transplant anti-MICA DSA and graft outcome
Immunization against MICA was analyzed using 225 serum samples collected 1 year after transplantation. In this subset of patients the median follow-up was 7.37 years (with a maximum at 9.58 years) and 7.34 years (with a maximum at 9.65 years) in those with and without anti-MICA DSA, respectively (Supplementary Table 2).
Although the presence of anti-MICA DSA at 1 year after transplantation was not associated with a higher incidence of graft failure, it was a risk factor for both TCMR (HR, 1.60; 95% CI: 1.01–2.53; P = 0.043) and ABMR (HR, 9.92; 95% CI: 7.43–13.20; P < 0.001; Fig. 2b and Table 3). Moreover, these associations were maintained when considering only the de novo fraction of these antibodies. Interestingly, the presence of de novo anti-MICA DSA was also a risk factor for graft survival (HR, 1.29; 95% CI: 1.05–1.58; P = 0.014; Table 3). Finally, the presence of anti-MICA DSA after transplantation was associated with a higher frequency of MICA mismatches whether considering all DSA present at 1 year after transplantation (0% versus 24.6% in matched versus mismatched patients, P = 0.0017) or only the de novo fraction of these antibodies (0% versus 13.5% in matched versus mismatched patients, P = 0.05).
We also tested whether specific MICA alleles were more prone to elicit DSA than others. For this purpose, we conducted a chi-squared test for equality of proportions on the proportion of individuals developing de novo anti-MICA DSA conditional on the presence of a specific MICA allele in the donor. There was no specific MICA allele that was associated with a higher rate of de novo anti-MICA DSA (Extended Data Table 5). Finally, when considering only eplet-specific anti-MICA DSA, the association with ABMR was similar to that of all anti-MICA DSA (Supplementary Fig. 3 and Extended Data Table 4).
The cumulative incidence of antibody-mediated rejection is shown for patients without DSA, with anti-MICA or anti-HLA DSA, and with both anti-MICA and anti-HLA DSA. The analysis was carried out for preformed (a) and post-transplantation DSA (b). P values were determined using the two-sided log-rank test without correction. Exact P values: a, P = 1.44 × 10−10; b, P = 5.03 × 10−17.
Synergetic effect of anti-MICA and anti-HLA DSA on ABMR
To evaluate the additive or synergetic impact of anti-MICA and anti-HLA DSA on ABMR, we analyzed the cumulative incidence of ABMR as a function of the presence or the absence of these antibodies before and after transplantation, as determined by single-antigen Luminex assays. The presence of anti-MICA or anti-HLA DSA, before and after transplantation, was a risk factor for ABMR (Fig. 3). In addition, both anti-MICA and anti-HLA DSA had an independent effect on ABMR, before and after transplantation (Extended Data Table 6). Interestingly, the risk of developing ABMR was highest when both types of antibodies were present (HR, 25.68; 95% CI: 3.31–199.41; P = 0.002 for preformed antibodies and HR, 82.67; 95% CI: 33.67–202.97; P < 0.001 for post-transplant antibodies; Fig. 3 and Extended Data Table 6).
Anti-MICA DSA and graft survival in an independent cohort
To further evaluate the role of anti-MICA DSA, we analyzed an independent cohort of 168 patients who had an episode of ABMR with or without anti-HLA DSA between 2013 and 2018. The median follow-up time after biopsy was 4.15 years (with a maximum at 7.90 years) and 4.47 years (with a maximum at 8.18 years) in those without (n = 124) and with (n = 44) anti-MICA DSA, respectively (Supplementary Table 3). The presence of anti-MICA DSA at the time of the diagnostic biopsy was associated with a decreased graft survival rate (HR, 1.71; 95% CI: 1.02–2.86; P = 0.041), as shown by a difference of 19% in survival at 6 years between patients with and without MICA DSA (Extended Data Fig. 2a). Of note, the graft survival was worst when both anti-MICA and anti-HLA DSA antibodies were present, confirming a synergetic effect of these antibodies on graft survival (Extended Data Fig. 2b).
Discussion
Here, we report that kidney transplantation from MICA-mismatched donors carries a significantly higher risk of graft failure. The lower graft survival can be explained by an increased rate of ABMR, which is independently associated with anti-MICA DSA. The present data formally define MICA as a bona fide transplantation antigen in kidney organ transplants and provide the rationale for including MICA genotyping and immunization monitoring in the pre- and post-transplantation workup. These results could be contextualized within several key, convergent and divergent, aspects of HLA and MIC genetics and immunobiology.
On the genetic side, one of the major challenges in any association study involving MHC genes is the high degree of linkage disequilibrium within the complex, here exemplified using that between MICA and HLA-B, which are separated by a 46 kb stretch of DNA (Extended Data Table 7 provides an update on linkage disequilibrium between MICA and all classical HLA genes). This could mean that some of the observed associations could indeed be due to linkage disequilibrium rather than being a primary association. However, the contribution of linkage disequilibrium to our results was ruled out by inclusion of all HLA mismatches as covariates in the multivariate Cox model, as well as by the observation of a still-significant association of graft survival with MICA mismatches in the subset of donors and recipients who were allele-matched for HLA-B (Table 2 and Extended Data Fig. 1). This is also in line with an independent assessment of the contribution of MICA mismatching to the outcome of hematopoietic cell transplants14,15.
Despite attention to long-term follow-up, it should also be noted that HLA-A, -B and -DRB1 mismatches had no impact on graft survival in this cohort (Extended Data Tables 1 and 2). This is probably due to the comparatively smaller size of our cohort with respect to large, (multi) continent-wide cohorts, which have been able to show HLA-dependent disease outcome in kidney transplant recipients; for example the Collaborative Transplant Study (CTS), UK Transplant and Eurotransplant, with more than 100,000 donor–recipient pairs16,17. The necessity of having large cohorts to show an HLA-mismatching effect is due to the following: there is only a 15% survival difference at 10 years after transplantation between fully matched kidneys and kidneys mismatched for both alleles at HLA-A, -B and -DRB1 loci18; and the magnitude of this effect has decreased over the years as a positive effect from many allocation policies taking matching into account19. The absence of MICA from these allocation policies may indeed explain why fewer donor–recipient pairs are needed to highlight a significant impact of MICA mismatching on graft outcome and, in consequence, to further incentivize its inclusion in a pre-transplant workup. Interestingly, in the subset of transplants with high-resolution typing of six HLA loci, only HLA-DQB1 mismatches were associated with lower graft survival (HR, 1.71; 95% CI: 1.35–2.17; P < 0.001; Extended Data Table 2). This observation is in line with recent reports showing associations of HLA-DQB1 mismatches with acute rejection20,21 and decreased graft survival22.
On the biological front, despite the fact that both MICA and HLA class I genes and molecules have a similar and unique tri-dimensional structure, major differences exist in their respective functions, for example HLA class I require both the β2-microglobulin and an endogenously derived peptide antigen for proper surface expression, and interact with the T cell receptor, whereas MICA does not require either β2-microglobulin or any peptide cargo for surface expression and interacts with a distinct receptor, NKG2D. Other differences include (and this is despite the fact that after HLA genes, MIC genes are the most polymorphic loci in the human genome) a substantially higher degree of diversity (for example, >8,000 HLA-B alleles versus >300 MICA alleles, vastly higher numbers of polymorphic positions for HLA molecules than MICA; see http://hla.alleles.org/alleles/index.html), and substantially stronger tissue expression for HLA class I than MICA (see comparative RNA sequencing data at https://gtexportal.org/home/multiGeneQueryPage/MICA,HLA-B). Incidentally, the last two facts are probably the reason for the higher antigenicity of HLA compared with MICA molecules, as evidenced by the disparity in the level of mean fluorescence intensity for anti-MICA compared with anti-HLA antibodies.
Independently of the influence of MICA genetic incompatibility on graft outcome, our study equally showed that the presence of pre- and post-transplantation anti-MICA DSA was strongly associated with an increased incidence of ABMR (Fig. 2 and Table 3), an effect that was independent of, and synergetic with, that of anti-HLA DSA (Fig. 3 and Extended Data Table 1). Indeed, because they were also associated with transplantation failure, de novo anti-MICA DSA appeared to be more harmful than preformed antibodies (Table 3). Given that these harmful antibodies are associated with MICA mismatches (0% versus 13.5% of patients with de novo antibodies in MICA-matched and -mismatched transplantations, respectively), they can be anticipated by performing pre-transplant MICA genotyping. Finally, anti-MICA DSA were confirmed to be harmful because they were associated with graft loss in an independent cohort of ABMR patients (Extended Data Fig. 2). Some of these observations were made in two subcohorts (pre-transplant and post-transplant) of the initial (master) cohort. Of note, patient inclusion in each subcohort depended solely on the availability of their sera (Supplementary Tables 1 and 2); and the incidence of the main endpoint analyzed in these subcohorts, ABMR, was not significantly different from that observed in the main cohort, that is: 6.3% in the main cohort versus 6.7% in the pre-transplant cohort (95% CI: 4.6–7.8; P = 0.57) and 6.3% versus 8.1% in the post-transplant subcohort (95% CI: 3.6–9.4; P = 0.17). Importantly, when analyzing the demographics and distribution of covariates in these two subcohorts, similarly to what had been already observed in the main cohort between MICA-matched and -mismatched transplantations, there were more retransplantations in the group with anti-MICA DSA than in the group without anti-MICA DSA (pre-transplant subcohort: 15.6% versus 5.8%, P = 0.005, Supplementary Table 1, and post-transplant subcohort: 14.3% versus 4%, P = 0.02, Supplementary Table 2). This observation could be explained by the fact that patients who had more than one transplantation are generally more immunized. The other unique covariate that was not equally distributed in patients with and without anti-MICA DSA was the proportion of potential recurrent nephropathies (11.7% versus 4.7%, P = 0.03), which was probably due to the fact that there were more retransplantations in these patients with potentially recurrent nephropathies than in those without (13.3% versus 6.9%).
Based on structural accessibility, MICA polymorphic residues can be grouped in small patches of surface-exposed amino acids, called eplets, using HLAMmatchmaker23. According to work by Duquesnoy et al., first for classical HLA molecules24 and later for MICA25, donor-specific eplets are thought to represent surface-accessible polymorphic amino acids prone to elicit DSA. Even though this theory has been verified for HLA (for example ref. 26), when considering MICA eplet mismatches instead of global MICA mismatches and eplet-specific anti-MICA DSA instead of all donor-specific anti-MICA DSA, similar results but no improvements in terms of associations with graft loss or ABMR could be evidenced in our dataset (Supplementary Figs. 1–3 and Extended Data Table 4). This discrepancy with HLA might be explained by the fact that MICA-mismatched alleles considered as matched at the eplet level may have immunogenic characteristics that cannot be identified using the HLAMmatchmaker approach. The limited number of reported eplet validation sera for MICA and the less extensive knowledge of MICA structures and polymorphisms may also be reasons for the non-superiority of associations measured when restricting the analysis to eplets. To sum up, in contrast to the HLA setting, the global and eplet mismatching models performed equally well for MICA. Although immunologically more correct, the eplet model and the number of identified eplets for MICA might still need improvements to demonstrate its superiority over the global mismatching model. The outcomes of this study warrant further detailed investigations on the eplet model for MICA.
In conclusion, molecular typing of MICA in association with screening for anti-MICA antibodies has the potential to lower the incidence of kidney transplantation rejection and loss.
Methods
Study design and oversight
The aim of this retrospective histocompatibility study was to examine whether donor–recipient matching at the MICA locus improves the outcomes of kidney transplantation. Kidney transplant recipients (and their donors) from seven French centers (Montpellier, Paris–Saint-Louis, Toulouse, Paris–Necker, Nancy, Nantes and Strasbourg) were enrolled. Genomic DNA and sera were collected in each participating center in the course of routine medical care and histocompatibility geno- and serotyping. The study was approved by the institutional review boards (IRBs) of Nantes University Hospital (CPP Grand Ouest DC-2011-1399, on behalf of all participating centers, except Strasbourg) and Strasbourg University Hospital (CPP Est number DC-2013-1990). The study was performed according to the principles of the Helsinki declaration. Written informed consent was obtained from all participants of both the initial and the independent cohorts.
Patients and donors
The study population consisted of 1,356 kidney transplant recipients (and donors) from six of the seven centers (Montpellier, Paris–Saint-Louis, Toulouse, Paris–Necker, Nancy and Nantes) who underwent kidney transplantation between 2002 and 2011. The patients who survived and were not lost to follow-up during the study were followed until 1 January 2015. All patients who underwent transplantation and died during the study period were included in the analysis. The transplantation allocation rules were the same for all seven centers and followed the recommendations of the French national agency for organ procurement (Agence de la biomédecine, Paris, France). All transplants were ABO compatible, and cross-matching for immunoglobulin (Ig)G T cell and B cell complement-dependent cytotoxicity was negative for all patients before transplantation. An independent cohort of 168 patients from Strasbourg University Hospital with a biopsy-proven acute ABMR episode that occurred between 2013 and 2018 was also analyzed. These patients had ABMR-specific lesions with (n = 81) or without (n = 87) anti-HLA DSA.
MICA and HLA genotyping
Genotyping of MICA in all donors and recipients was carried out using sequence-based typing: exons 2, 3 and 4 were bidirectionally Sanger-sequenced, and the transmembrane microsatellite polymorphism was genotyped as follows. A fragment spanning exons 2–5 of the MICA gene was amplified using polymerase chain reaction (PCR) on genomic DNA with a forward (5'-CGTTCTTGTCCCTTTGCCCGTGTGC-3') and a reverse (5'-GATGCTGCCCCCATTCCCTTCCCAA-3') primer using the Expand Long Template PCR System (Roche), following the manufacturer’s recommendations. After purification with the QIAquick PCR Purification Kit (QIAGEN), the PCR product was directly sequenced with the BigDye Terminator v3.1 Cycle sequencing kit and run on a 96 capillary ABI3730XL Genetic Analyzer (ThermoFisher Scientific). Sequences were analyzed using Seqscape v2.6 (ThermoFisher Scientific). The MICA-transmembrane (TM) coding region was amplified with a forward primer labeled at the 5' end with 6-carboxyfluorescein (FAM) (5'-CCTTTTTTTCAGGGAAAGTGC-3') and a reverse primer (5'-CCTTACCATCTCCAGAAACTGC-3'), using GoTaq Polymerase (Promega) following the manufacturer’s instructions. To determine the number of triplet repeats in the TM region of the MICA gene, PCR products were run on a 96 capillary ABI3130xl Genetic Analyzer and their sizes were determined using Genemapper v4.0 (ThermoFisher Scientific). MICA-TM genotypes (MICA A4, A5, A5.1, A6 or A9) were determined by comparing the sizes of the obtained fragments with controls of known genotypes27. Final MICA genotypes were assigned using an in-house developed VBA code (Microsoft Excel) compiling sequence data and MICA-TM genotypes. Finally, ambiguous results were resolved by PCR amplification with sequence-specific primers. Upon completion of this procedure, analysis of matching and mismatching between donors and recipients was performed at allele-level resolution (second field in the HLA nomenclature28). HLA genotyping data were retrieved from participating centers, with a first-field resolution for HLA-A, -B and -DRB1 loci. Retrospective second-field-resolution HLA-A, -B, -C, -DRB1, -DQB1 and -DPB1 genotyping was performed by sequence-based typing on a subset of 862 donor–recipient pairs for whom sufficient DNA was available.
Anti-HLA and -MICA antibody testing
In the main cohort we used 524 pre-transplant serum samples and 225 post-transplant (at 1 year) serum samples to evaluate levels of anti-HLA and MICA DSA with the respective LABScreen Single Antigen kits (One Lambda) following the manufacturer’s instructions. The same kits and conditions were used to evaluate anti-HLA and anti-MICA DSA in an independent cohort of 168 patients who had an episode of ABMR at the time of diagnostic biopsy. Antibodies were detected based on the mean fluorescence intensity (MFI) for each bead coated with an HLA or MICA antigen, as normalized to the value measured with the negative control serum using the baseline method. All beads with normalized MFI higher than 500 or 100 were considered positive for HLA and MICA, respectively. The MFI cut-off for positivity of anti-MICA DSA was chosen based on a receiver operating characteristic analysis (Supplementary Fig. 4). The maximum MFI of DSA was defined as the highest ranked donor-specific bead. For the remaining patients, anti-HLA antibody testing was performed using either complement-dependent cytotoxicity, ELISA or Luminex-based tests.
Statistical analyses
The primary endpoint of the study was the post-transplantation time to graft failure, which was censored at the time of the last follow-up or death. The secondary endpoint was the first episode of acute rejection. All acute rejection episodes were biopsy proven and classified according to the Banff classification29. Acute rejection episodes were classified into acute TCMR and ABMR. Delayed graft function was defined as the use of dialysis within 7 days after transplantation, except in the case of one-off dialysis for hyperkalemia or fluid overload, which was not counted as delayed graft function. All statistical models were adjusted for the center effect30 and included the following covariates: donor age, recipient age, donor sex, recipient sex, deceased–living status of donor, recipient body mass index, cause of end-stage kidney disease, year of transplantation, graft rank, type of transplantation, time from dialysis to transplantation, cold ischemia time, delayed graft function, donor and recipient cytomegalovirus status, induction treatment, HLA mismatches, and pre-transplantation anti-HLA class I and II antibodies including those that were donor-specific. Continuous variables were transformed into categorical variables. We used counts and percentages to describe variables. A chi-squared test for independence (or Fisher’s exact test if appropriate) was used to examine the association between the MICA matching variable and each other variable.
Probabilities of graft survival and univariate analysis were assessed using Kaplan–Meier curves and the log-rank test. Cox proportional hazards models were applied to quantify hazard ratios and 95% confidence intervals. The association of factors with graft survival and acute rejection was determined by multivariate Cox regression analysis. Multivariate models were all adjusted for center effects, and all models were evaluated for proportional hazards assumptions. All reported P values were two-sided and were considered to indicate statistical significance if less than 0.05. Statistical analysis was performed using the computing environment R (v4.0.2) with the CRAN survival package (https://cran.rproject.org/web/packages/survival/index.html).
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All requests for raw or processed data will be promptly reviewed by representatives of all centers having participated in the study, and given that the request is reasonable and complies with the French (and the requestor country’s) national laws and regulations, de-identified data will be shared upon the signing of a data transfer agreement. All such requests should be directly addressed to the corresponding author (S.B.) (siamak@unistra.fr). Source data are provided with this paper.
Code availability
The VBA code for MICA typing has been deposited and is available at https://doi.org/10.5281/zenodo.5879173 website.
References
Knechtle, S., Marson, L. & Morris, P. Kidney Transplantation – Principles and Practice (Elsevier, 2019).
Merrill, J. P., Murray, J. E., Harrison, J. H. & Guild, W. R. Successful homotransplantation of the human kidney between identical twins. JAMA 160, 277–282 (1956).
Snell, G. D. Methods for the study of histocompatibility genes. J. Genet. 49, 87–108 (1948).
Snell, G. D. Studies in histocompatibility. Science 213, 172–178 (1981).
Bohmig, G. A., Eskandary, F., Doberer, K. & Halloran, P. F. The therapeutic challenge of late antibody-mediated kidney allograft rejection. Transpl. Int. 32, 775–788 (2019).
Tambur, A. R. et al. Sensitization in Transplantation: Assessment of Risk (STAR) 2017 Working Group meeting report. Am. J. Transplant. 18, 1604–1614 (2018).
Schinstock, C. A. et al. A 2020 Banff Antibody-mediated Injury Working Group examination of international practices for diagnosing antibody-mediated rejection in kidney transplantation: a cohort study. Transpl. Int. 34, 488–498 (2021).
Jackson, A. M., Wiebe, C. & Hickey, M. J. The role of non-HLA antibodies in solid organ transplantation: a complex deliberation. Curr. Opin. Organ Transplant. 25, 536–542 (2020).
Bahram, S., Bresnahan, M., Geraghty, D. E. & Spies, T. A second lineage of mammalian major histocompatibility complex class I genes. Proc. Natl Acad. Sci. USA 91, 6259–6263 (1994).
Carapito, R. & Bahram, S. Genetics, genomics, and evolutionary biology of NKG2D ligands. Immunol. Rev. 267, 88–116 (2015).
Zou, Y., Stastny, P., Susal, C., Dohler, B. & Opelz, G. Antibodies against MICA antigens and kidney-transplant rejection. N. Engl. J. Med. 357, 1293–1300 (2007).
Risti, M. & Bicalho, M. D. MICA and NKG2D: is there an impact on kidney transplant outcome? Front. Immunol. 8, 179 (2017).
Baranwal, A. K. & Mehra, N. K. Major histocompatibility complex class I chain-related A (MICA) molecules: relevance in solid organ transplantation. Front. Immunol. 8, 182 (2017).
Fuerst, D. et al. Matching for the MICA-129 polymorphism is beneficial in unrelated hematopoietic stem cell transplantation. Blood 128, 3169–3176 (2016).
Carapito, R. et al. Matching for the nonconventional MHC-I MICA gene significantly reduces the incidence of acute and chronic GVHD. Blood 128, 1979–1986 (2016).
Susal, C. & Opelz, G. Impact of HLA matching and HLA antibodies in organ transplantation: a collaborative transplant study view. Methods Mol. Biol. 882, 267–277 (2012).
Doxiadis, I. I., Smits, J. M., Persijn, G. G., Frei, U. & Claas, F. H. It takes six to boogie: allocating cadaver kidneys in Eurotransplant. Transplantation 77, 615–617 (2004).
Sasaki, N. & Idica, A. The HLA-matching effect in different cohorts of kidney transplant recipients: 10 years later. Clin. Transpl. 261–282 (2010).
Johnson, R. J. et al. A new UK 2006 National Kidney Allocation Scheme for deceased heart-beating donor kidneys. Transplantation 89, 387–394 (2010).
Lim, W. H. et al. HLA-DQ mismatches and rejection in kidney transplant recipients. Clin. J. Am. Soc. Nephrol. 11, 875–883 (2016).
Khongjaroensakun, N., Kitpoka, P., Wiwattanathum, P., Sakulchairungrueng, B. & Thammanichanond, D. Influence of HLA-DQ matching on allograft outcomes in deceased donor kidney transplantation. Transplant. Proc. 50, 2371–2376 (2018).
Leeaphorn, N. et al. HLA-DQ mismatching and kidney transplant outcomes. Clin. J. Am. Soc. Nephrol. 13, 763–771 (2018).
Duquesnoy, R. J. HLAMmatchmaker: a molecularly based donor selection algorithm for highly alloimmunized patients. Transplant. Proc. 33, 493–497 (2001).
Duquesnoy, R. J. A structurally based approach to determine HLA compatibility at the humoral immune level. Hum. Immunol. 67, 847–862 (2006).
Duquesnoy, R. J., Mostecki, J., Hariharan, J. & Balazs, I. Structurally based epitope analysis of major histocompatibility complex class I-related chain A (MICA) antibody specificity patterns. Hum. Immunol. 69, 826–832 (2008).
Senev, A. et al. Eplet mismatch load and de novo occurrence of donor-specific anti-HLA antibodies, rejection, and graft failure after kidney transplantation: an observational cohort study. J. Am. Soc. Nephrol. 31, 2193–2204 (2020).
Fodil, N. et al. Allelic repertoire of the human MHC class I MICA gene. Immunogenetics 44, 351–357 (1996).
Marsh, S. G. et al. Nomenclature for factors of the HLA system, 2010. Tissue Antigens 75, 291–455 (2010).
Solez, K. et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am. J. Transplant. 8, 753–760 (2008).
Therneau, T .M. & Grambsch, P. M. Modeling Survival Data: Extending the Cox Model (Springer, 2000).
Acknowledgements
The authors thank Y. Foucher (Nantes University, Nantes, France) and P. Ravaud (Paris Descartes University, Paris, France) for discussing the statistical approaches, and E. Nourisson for technical assistance. This work was supported by France’s National Research Agency (Agence Nationale de Recherche; ANR), the Investment for the Future Program (Programme des Investissements d’Avenir; PIA) through a ‘Laboratoire d’Excellence’ (LabEx) TRANSPLANTEX (ANR-11-LABX-0070_TRANSPLANTEX) as well as by Strasbourg’s Interdisciplinary Thematic Institute (ITI) for Precision Medicine, TRANSPLANTEX NG, as part of the ITI 2021–2028 program of the University of Strasbourg, CNRS and INSERM, funded by IdEx Unistra (ANR-10-IDEX-0002) and SFRI-STRAT’US (ANR-20-SFRI-0012), all to S.B. Additional funding was provided by INSERM (UMR_S 1109), the Institut Universitaire de France (IUF), the Fédération Hospitalo-Universitaire (FHU) OMICARE, MSD Avenir ‘Autogen’, all to S.B., and the European regional development fund (European Union) INTERREG V program (project no. 3.2 TRIDIAG and PERSONALIS) to R.C. and S.B.
Author information
Authors and Affiliations
Contributions
R.C. performed the experiments, designed the study, analyzed the data and wrote the manuscript. S.B. designed the study, analyzed the data and wrote the manuscript. C.Süs. performed experiments, analyzed the data and discussed the results. M.U., A.P., A.M., I.K., T.B., X.B. and N.C. performed the experiments and analyzed the data. I.A., M.V., S.M. and B.M.M. performed the statistical analysis. A.W., A.A., A.E., A.K., C.Sub., N.C.-J., A.B., P.P., S.C. and D.C. provided samples and clinical data, interpreted the clinical data and discussed the results. F.D., J.-L.T., E.S., V.G., V.P., L.W., M.N., N.K., C.L., D.G., M.L. and D.A. interpreted the clinical data and discussed results. M.M.-B. and F.B. analyzed the data and reviewed the statistical analysis. M.G., L.F. and J.P. collected the clinical and biological data. All authors contributed to the writing and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
D.A. has a patent ‘In vitro method for determining the likelihood of occurrence of an acute microvascular rejection (AMVR) against a renal allograft in an individual’ (EP19305037.4) issued. S.B. reports grants and personal fees from BIOMICA and personal fees from GenDx. S.C. reports non-financial support from Sanofi and Astellas, and non-financial support from Novartis, outside the submitted work. N.K. reports personal fees from Abbvie, Amgen, Astellas, Biotest, CSL Behring, Chiesi, Gilead, Fresenius Medical care, Merck Sharp and Dohme, Neovii, Novartis Pharma, Sanofi, Sandoz and Shire, outside the submitted work. P.P. reports personal fees from Chiesi, outside the submitted work. All other authors have no competing interests.
Peer review
Peer review information
Nature Medicine thanks Rutger Ploeg and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Anna Maria Ranzoni was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Kaplan–Meier curves for kidney graft survival according to the MICA matching status in HLA-B matched patients as determined by high-resolution HLA-typing.
The probability of graft survival is shown for patients matched versus mismatched at the MICA locus using presence/absence of mismatches. Two-sided log-rank test p-value without correction is shown.
Extended Data Fig. 2 Kaplan–Meier curves for kidney graft survival according to anti-MICA and anti-HLA DSA antibodies in an independent cohort with ABMR.
The probability of graft survival is shown for patients with anti-MICA DSA at the time of biopsy versus those without anti-MICA DSA (panel A) and for patients without DSA, with anti-MICA or anti-HLA DSA, and with both anti-MICA and anti-HLA DSA (panel B). Two-sided log-rank test P values without correction are shown.
Supplementary information
Supplementary Information
Supplementary Figs. 1–4, Supplementary Tables 1–3.
Source data
Source Data Fig. 1
Statistical source data for graft survival curves.
Source Data Fig. 2
Statistical source data for cumulative rejection incidence curves.
Source Data Fig. 3
Statistical source data for graft survival curves.
Source Data Extended Data Fig. 1
Statistical source data for graft survival curves.
Source Data Extended Data Fig. 2
Statistical source data for graft survival curves.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Carapito, R., Aouadi, I., Verniquet, M. et al. The MHC class I MICA gene is a histocompatibility antigen in kidney transplantation. Nat Med 28, 989–998 (2022). https://doi.org/10.1038/s41591-022-01725-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-01725-2
This article is cited by
-
MICA in kidney transplants
Nature Reviews Nephrology (2022)