Abstract
Objective
We sought to explore whether classification of patients with heart failure and mid-range (HFmrEF) or preserved ejection fraction (HFpEF) according to their left ventricular ejection fraction (LVEF) identifies differences in their exercise hemodynamic profile, and whether classification according to an index of right ventricular (RV) function improves differentiation.
Background
Patients with HFmrEF and HFpEF have hemodynamic compromise on exertion. The classification according to LVEF implies a key role of the left ventricle. However, RV involvement in exercise limitation is increasingly recognized. The tricuspid annular plane systolic excursion/systolic pulmonary arterial pressure (TAPSE/PASP) ratio is an index of RV and pulmonary vascular function. Whether exercise hemodynamics differ more between HFmrEF and HFpEF than between TAPSE/PASP tertiles is unknown.
Methods
We analyzed 166 patients with HFpEF (LVEF ≥ 50%) or HFmrEF (LVEF 40–49%) who underwent basic diagnostics (laboratory testing, echocardiography at rest, and cardiopulmonary exercise testing [CPET]) and exercise with right heart catheterization. Hemodynamics were compared according to echocardiographic left ventricular or RV function.
Results
Exercise hemodynamics (e.g. pulmonary arterial wedge pressure/cardiac output [CO] slope, CO increase during exercise, and maximum total pulmonary resistance) showed no difference between HFpEF and HFmrEF, but significantly differed across TAPSE/PASP tertiles and were associated with CPET results. N-terminal pro-brain natriuretic peptide concentration also differed significantly across TAPSE/PASP tertiles but not between HFpEF and HFmrEF.
Conclusion
In patients with HFpEF or HFmrEF, TAPSE/PASP emerged as a more appropriate stratification parameter than LVEF to predict clinically relevant impairment of exercise hemodynamics.
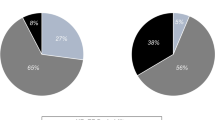
Graphic abstract

Stratification of exercise hemodynamics in patients with HFpEF or HFmrEF according to LVEF or TAPSE/PASP, showing significant distinctions only with the RV-based strategy. All data are shown as median [upper limit of interquartile range] and were calculated using the independent-samples Mann–Whitney U test or Kruskal–Wallis test. PVR pulmonary vascular resistance; max maximum level during exercise.


Similar content being viewed by others
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer PTF, Authors/Task Force Members (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Nauta JF, Hummel YM, van Melle JP, van der Meer P, Lam CSP, Ponikowski P, Voors AA (2017) What have we learned about heart failure with mid-range ejection fraction one year after its introduction? Eur J Heart Fail 19(12):1569–1573. https://doi.org/10.1002/ejhf.1058
Rickenbacher P, Kaufmann BA, Maeder MT, Bernheim A, Goetschalckx K, Pfister O, Pfisterer M, Brunner-La Rocca HP, TIME-CHF Investigators (2017) Heart failure with mid-range ejection fraction: a distinct clinical entity? Insights from the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF). Eur J Heart Fail. https://doi.org/10.1002/ejhf.798
Bristow MR, Kao DP, Breathett KK, Altman NL, Gorcsan J 3rd, Gill EA, Lowes BD, Gilbert EM, Quaife RA, Mann DL (2017) Structural and functional phenotyping of the failing heart: is the left ventricular ejection fraction obsolete? JACC Heart failure 5(11):772–781. https://doi.org/10.1016/j.jchf.2017.09.009
Mele D, Nardozza M, Ferrari R (2018) Left ventricular ejection fraction and heart failure: an indissoluble marriage? Eur J Heart Fail 20(3):427–430. https://doi.org/10.1002/ejhf.1071
Corra U, Agostoni PG, Anker SD, Coats AJS, Crespo Leiro MG, de Boer RA, Harjola VP, Hill L, Lainscak M, Lund LH, Metra M, Ponikowski P, Riley J, Seferovic PM, Piepoli MF (2018) Role of cardiopulmonary exercise testing in clinical stratification in heart failure. A position paper from the Committee on Exercise Physiology and Training of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 20(1):3–15. https://doi.org/10.1002/ejhf.979
Rieth A, Richter MJ, Gall H, Seeger W, Ghofrani HA, Mitrovic V, Hamm CW (2017) Hemodynamic phenotyping based on exercise catheterization predicts outcome in patients with heart failure and reduced ejection fraction. J Heart Lung Transplant 36(8):880–889. https://doi.org/10.1016/j.healun.2017.02.022
Guazzi M, Naeije R (2017) Pulmonary hypertension in heart failure: pathophysiology, pathobiology, and emerging clinical perspectives. J Am Coll Cardiol 69(13):1718–1734. https://doi.org/10.1016/j.jacc.2017.01.051
Guazzi M, Bandera F, Pelissero G, Castelvecchio S, Menicanti L, Ghio S, Temporelli PL, Arena R (2013) Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol 305(9):H1373-1381. https://doi.org/10.1152/ajpheart.00157.2013
Tello K, Wan J, Dalmer A, Vanderpool R, Ghofrani HA, Naeije R, Roller F, Mohajerani E, Seeger W, Herberg U, Sommer N, Gall H, Richter MJ (2019) Validation of the tricuspid annular plane systolic excursion/systolic pulmonary artery pressure ratio for the assessment of right ventricular-arterial coupling in severe pulmonary hypertension. Circ Cardiovasc Imaging. https://doi.org/10.1161/CIRCIMAGING.119.009047
Guazzi M, Dixon D, Labate V, Beussink-Nelson L, Bandera F, Cuttica MJ, Shah SJ (2017) RV contractile function and its coupling to pulmonary circulation in heart failure with preserved ejection fraction: stratification of clinical phenotypes and outcomes. JACC Cardiovasc Imaging 10(10 Pt B):1211–1221. https://doi.org/10.1016/j.jcmg.2016.12.024
Guazzi M, Naeije R, Arena R, Corra U, Ghio S, Forfia P, Rossi A, Cahalin LP, Bandera F, Temporelli P (2015) Echocardiography of right ventriculoarterial coupling combined with cardiopulmonary exercise testing to predict outcome in heart failure. Chest 148(1):226–234. https://doi.org/10.1378/chest.14-2065
Tello K, Axmann J, Ghofrani HA, Naeije R, Narcin N, Rieth A, Seeger W, Gall H, Richter MJ (2018) Relevance of the TAPSE/PASP ratio in pulmonary arterial hypertension. Int J Cardiol 266:229–235. https://doi.org/10.1016/j.ijcard.2018.01.053
Gall H, Felix JF, Schneck FK, Milger K, Sommer N, Voswinckel R, Franco OH, Hofman A, Schermuly RT, Weissmann N, Grimminger F, Seeger W, Ghofrani HA (2017) The Giessen Pulmonary Hypertension Registry: survival in pulmonary hypertension subgroups. J Heart Lung Transplant 36(9):957–967. https://doi.org/10.1016/j.healun.2017.02.016
Kovacs G, Herve P, Barbera JA, Chaouat A, Chemla D, Condliffe R, Garcia G, Grunig E, Howard L, Humbert M, Lau E, Laveneziana P, Lewis GD, Naeije R, Peacock A, Rosenkranz S, Saggar R, Ulrich S, Vizza D, Vonk Noordegraaf A, Olschewski H (2017) An official European Respiratory Society statement: pulmonary haemodynamics during exercise. Eur Respir J 50(5):1700578. https://doi.org/10.1183/13993003.00578-2017
Berry NC, Manyoo A, Oldham WM, Stephens TE, Goldstein RH, Waxman AB, Tracy JA, Leary PJ, Leopold JA, Kinlay S, Opotowsky AR, Systrom DM, Maron BA (2015) Protocol for exercise hemodynamic assessment: performing an invasive cardiopulmonary exercise test in clinical practice. Pulm Circ 5(4):610–618. https://doi.org/10.1086/683815
Kang G, Ha R, Banerjee D (2016) Pulmonary artery pulsatility index predicts right ventricular failure after left ventricular assist device implantation. J Heart Lung Transplant 35(1):67–73. https://doi.org/10.1016/j.healun.2015.06.009
Armstrong HF, Schulze PC, Kato TS, Bacchetta M, Thirapatarapong W, Bartels MN (2013) Right ventricular stroke work index as a negative predictor of mortality and initial hospital stay after lung transplantation. J Heart Lung Transplant 32(6):603–608. https://doi.org/10.1016/j.healun.2013.03.004
Medrek SK, Kloefkorn C, Nguyen DTM, Graviss EA, Frost AE, Safdar Z (2017) Longitudinal change in pulmonary arterial capacitance as an indicator of prognosis and response to therapy and in pulmonary arterial hypertension. Pulm Circ. https://doi.org/10.1177/2045893217698715
Oliveira RKF, Faria-Urbina M, Maron BA, Santos M, Waxman AB, Systrom DM (2017) Functional impact of exercise pulmonary hypertension in patients with borderline resting pulmonary arterial pressure. Pulm Circ 7(3):654–665. https://doi.org/10.1177/2045893217709025
Tello K, Richter MJ, Axmann J, Buhmann M, Seeger W, Naeije R, Ghofrani HA, Gall H (2018) More on single-beat estimation of right ventriculoarterial coupling in pulmonary arterial hypertension. Am J Respir Crit Care Med 198(6):816–818. https://doi.org/10.1164/rccm.201802-0283LE
Tedford RJ (2014) Determinants of right ventricular afterload (2013 Grover Conference series). Pulmonary circulation 4(2):211–219. https://doi.org/10.1086/676020
Saouti N, Westerhof N, Helderman F, Marcus JT, Boonstra A, Postmus PE, Vonk-Noordegraaf A (2010) Right ventricular oscillatory power is a constant fraction of total power irrespective of pulmonary artery pressure. Am J Respir Crit Care Med 182(10):1315–1320. https://doi.org/10.1164/rccm.200910-1643OC
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M (2015) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 46(4):903–975. https://doi.org/10.1183/13993003.01032-2015
Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redfield MM (2009) Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol 53(13):1119–1126. https://doi.org/10.1016/j.jacc.2008.11.051
Fonarow GC (2017) Refining classification of heart failure based on ejection fraction. JACC Heart Fail 5(11):808–809. https://doi.org/10.1016/j.jchf.2017.08.011
Cikes M, Solomon SD (2016) Beyond ejection fraction: an integrative approach for assessment of cardiac structure and function in heart failure. Eur Heart J 37(21):1642–1650. https://doi.org/10.1093/eurheartj/ehv510
Tumminello G, Lancellotti P, Lempereur M, D’Orio V, Pierard LA (2007) Determinants of pulmonary artery hypertension at rest and during exercise in patients with heart failure. Eur Heart J 28(5):569–574. https://doi.org/10.1093/eurheartj/ehl561
Kjaergaard J, Akkan D, Iversen KK, Kober L, Torp-Pedersen C, Hassager C (2007) Right ventricular dysfunction as an independent predictor of short- and long-term mortality in patients with heart failure. Eur J Heart Fail 9(6–7):610–616. https://doi.org/10.1016/j.ejheart.2007.03.001
Gorter TM, Hoendermis ES, van Veldhuisen DJ, Voors AA, Lam CS, Geelhoed B, Willems TP, van Melle JP (2016) Right ventricular dysfunction in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail 18(12):1472–1487. https://doi.org/10.1002/ejhf.630
Gorter TM, van Veldhuisen DJ, Bauersachs J, Borlaug BA, Celutkiene J, Coats AJS, Crespo-Leiro MG, Guazzi M, Harjola VP, Heymans S, Hill L, Lainscak M, Lam CSP, Lund LH, Lyon AR, Mebazaa A, Mueller C, Paulus WJ, Pieske B, Piepoli MF, Ruschitzka F, Rutten FH, Seferovic PM, Solomon SD, Shah SJ, Triposkiadis F, Wachter R, Tschope C, de Boer RA (2018) Right heart dysfunction and failure in heart failure with preserved ejection fraction: mechanisms and management. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 20(1):16–37. https://doi.org/10.1002/ejhf.1029
Harjola V-P, Mebazaa A, Čelutkienė J, Bettex D, Bueno H, Chioncel O, Crespo-Leiro MG, Falk V, Filippatos G, Gibbs S, Leite-Moreira A, Lassus J, Masip J, Mueller C, Mullens W, Naeije R, Nordegraaf AV, Parissis J, Riley JP, Ristic A, Rosano G, Rudiger A, Ruschitzka F, Seferovic P, Sztrymf B, Vieillard-Baron A, Yilmaz MB, Konstantinides S (2016) Contemporary management of acute right ventricular failure: a statement from the Heart Failure Association and the Working Group on Pulmonary Circulation and Right Ventricular Function of the European Society of Cardiology. Eur J Heart Fail 18(3):226–241. https://doi.org/10.1002/ejhf.478
Champion HC, Michelakis ED, Hassoun PM (2009) Comprehensive invasive and noninvasive approach to the right ventricle-pulmonary circulation unit: state of the art and clinical and research implications. Circulation 120(11):992–1007. https://doi.org/10.1161/CIRCULATIONAHA.106.674028
Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiery JL (2016) Left ventricular heart failure and pulmonary hypertension. Eur Heart J 37(12):942–954. https://doi.org/10.1093/eurheartj/ehv512
Gorter TM, van Veldhuisen DJ, Voors AA, Hummel YM, Lam CSP, Berger RMF, van Melle JP, Hoendermis ES (2018) Right ventricular-vascular coupling in heart failure with preserved ejection fraction and pre- vs. post-capillary pulmonary hypertension. Eur Heart J Cardiovasc Imaging 19(4):425–432. https://doi.org/10.1093/ehjci/jex133
Bosch L, Lam CSP, Gong L, Chan SP, Sim D, Yeo D, Jaufeerally F, Leong KTG, Ong HY, Ng TP, Richards AM, Arslan F, Ling LH (2017) Right ventricular dysfunction in left-sided heart failure with preserved versus reduced ejection fraction. Eur J Heart Fail 19(12):1664–1671. https://doi.org/10.1002/ejhf.873
Ghio S, Guazzi M, Scardovi AB, Klersy C, Clemenza F, Carluccio E, Temporelli PL, Rossi A, Faggiano P, Traversi E, Vriz O, Dini FL, all i, (2017) Different correlates but similar prognostic implications for right ventricular dysfunction in heart failure patients with reduced or preserved ejection fraction. Eur J Heart Fail 19(7):873–879. https://doi.org/10.1002/ejhf.664
Greenberg B (2017) Jumping down the rabbit hole: unravelling the right ventricle in heart failure. Eur J Heart Fail 19(12):1672–1674. https://doi.org/10.1002/ejhf.985
Gorter TM, Obokata M, Reddy YNV, Melenovsky V, Borlaug BA (2018) Exercise unmasks distinct pathophysiologic features in heart failure with preserved ejection fraction and pulmonary vascular disease. Eur Heart J 39(30):2825–2835. https://doi.org/10.1093/eurheartj/ehy331
Acknowledgements
Funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation)—Project Number 268555672–SFB 1213, Project B08. We thank Claire Mulligan, Ph.D. (Beacon Medical Communications Ltd, Brighton, UK), for editorial support funded by the University of Giessen.
Funding
Funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation)—Project Number 268555672–SFB 1213, Project B08.
Author information
Authors and Affiliations
Contributions
Each author has contributed significantly to this work: AJR, MJR, KT: conception and design, analysis and interpretation of data; drafting of the manuscript; final approval of the manuscript submitted. HG, HAG, SG, CBW, WS, SDK, VM, PCS, CWH: analysis and interpretation of data; revising the manuscript critically for important intellectual content; final approval of the manuscript submitted.
Corresponding author
Ethics declarations
Conflict of interest
All authors report that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Ethical approval
The investigation conforms with the principles outlined in the Declaration of Helsinki. All patients enrolled into the registries gave written informed consent, and data collection and analyses were approved by the ethics committee of the Faculty of Medicine at the University of Giessen (Approval No. 186/16, 266/11, 117/16).
Consent to participate
All patients enrolled into the registries gave written informed consent.
Consent for publication
All patients enrolled into the registries gave written informed consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rieth, A.J., Richter, M.J., Tello, K. et al. Exercise hemodynamics in heart failure patients with preserved and mid-range ejection fraction: key role of the right heart. Clin Res Cardiol 111, 393–405 (2022). https://doi.org/10.1007/s00392-021-01884-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01884-1